CONGENITAL TALIPES EUINOVARUS (CTEV): PHYSIOTHERAPY MANAGEMENT
CONGENITAL TALIPES EUINO VARUS (CTEV)
DEFINITION/INTRODUCTION:
- Congenital talipes equinovarus, also known as ‘club foot’, is a congenital foot deformity present at birth. It is one of the most common congenital deformities.
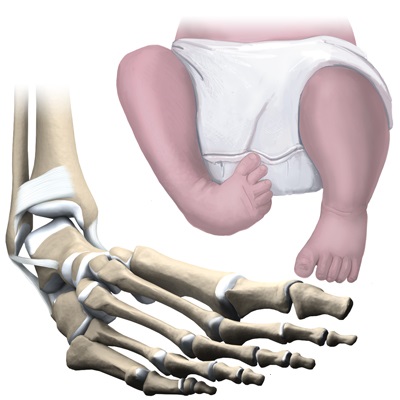
- The foot consists of 26 bones. Most relevant for this congenital deformity are the talus, calcaneus and navicular. The calcaneus and navicular are medially rotated in relation to the talus. The foot is held in adduction and inversion by ligaments and muscles.
- Muscles that are contracted are triceps surae, tibialis posterior, flexor digitorum longus and flexor hallucis longus. Weak peroneal muscles allow the foot to be inverted. The ligaments of the posterior and medial aspect of the ankle are thick and taut.
- Without treatment, a patient with a clubfoot will walk on the outside of the foot which may produce pain and/or disability. A clubfoot is usually smaller than an unaffected (normal) foot. The calf is also usually smaller on the side of the clubfoot. One or both feet may be affected.
TYPES of CONGENITAL TALIPES EUINO VARUS:
- (1) Idiopathic (Unknown Etiology):
- Congenital talipes euino varus(CTEV).
- (2) Acquired:
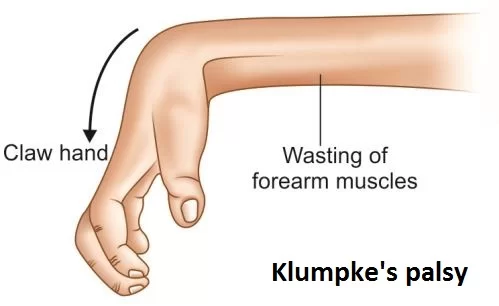
- CNS disease: Spina bifida, poliomyelitis.
- Arthrogryposis.
- Absent bone: Fibula/tibia.
COMPONENTS OF THE DEFORMITY:
- Equinus: At the ankle joint plantar flexion of the forefoot.
- Varus: Primary at sub talar joint but entire tarsus rotated except talus.
- Adduction: Talonavicular and tarso metatarsal joint.
- Cavus: Forefoot plantar flexion.
ANATOMICAL REGION INVOLVEMENT:
- Posterior contracture: Tend Achilles, tibiotalar capsule, talo calcaneal capsule, posterior talo fibular ligament, calcaneo fibulas ligament. These structures resist equinus correction.
- Medial: Most important and most resistant structures tibialis posterior, deltoid, talonavicular capsule and spring ligament.
- Subtalar: Talo calcaneal interosseousligament, bifurcated Y ligament.
- Plantar contractures: Abductor hallucis, intrinsic flexors, quadratusplantae, plantar aponeurosis.
ETIOLOGY:
- Polygenic.
- Multifactorial.
- Abnormal intrauterine forces.
- Arrested fetal development.
- Abnormal muscle and tendon insertions.
- Abnormal rotation of the talus in the mortise.
- Germ plasm defects.
- Neurogenic theory: Reduced motor unit, which counts in the distribution of the common peroneal nerve, may be responsible for clinically demonstrable muscle weakness.
- Myogenic theory: Suggested by the presence of anomalous muscles, e.g. accessory soleus muscle and flexor digitorum accessorious longus muscles, which can produce equinovarus deformity.
- Vascular theory: Diminution of blood flow in the anterior tibial artery and its derivatives.
- Embyonic theory: Developmental defect occurring up to 12 weeks of intrauterine life.
- Chromosonal theory: Presence of some chromosonal defects in unfertilized germ cells.
- Osteogenic theory: Due to some unknown cause, temporary arrest of development occurs in the 7- to 8- week-old embryo, which can lead to clubfoot or other deformities.
- Mechanical block theory: Due to some mechanical obstruction during the intrauterine development period, e.g. intrauterine fibrotic bands, less amniotic fluid, disproportionate uterine cavity, etc, talipes equinovarus can occur.
CLINICAL PRESENTATION/EXAMINATION:
- Smaller stubby feet with shortened first metatarsal ray.
- Equinus deformity with inversion of the heel, adduction and varus of the fore foot.
- Medial border of the foot is concave and elevated, its plantar surface face up ward.
- Lateral border of the foot is convex and depressed down.
- The posterior tuberosity of the heel is upwards, difficult to palpate and less visible.
- Callosity on the dorsal aspect of the fifth metatarsal.
- Bony prominence visible and palpable over the dorsolateral aspect of the foot represents the head and neck of the talus which are partially uncovered by the navicular.
SIGNS AND SYMPTOMS:
- Short Achilles tendon.
- High and small heel.
- No creases behind heel.
- Abnormal crease in middle of the foot.
- Foot is smaller in unilateral affection.
- Callosities at abnormal pressure areas.
- Internal torsion of the leg.
- Calf muscles wasting.
- Deformities don’t prevent walking.
PHYSIOTHERAPY MANAGEMENT:
- Physical therapy for Club Foot will be used to stretch the structures of the foot including the tendons, ligaments, and muscles to adjust the foot and keep it in the proper position. If surgery is needed, physical therapy will be initiated after the procedure to ensure that the correction takes hold.
- Bracing will be a critical component of recovery from a fixed Club Foot.

- Manual Therapeutic Technique (MTT):
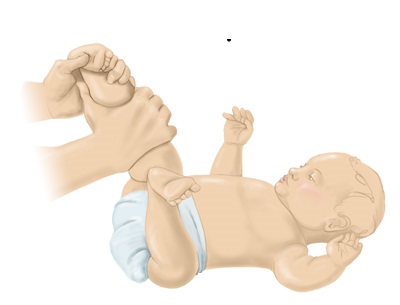
- Hands on care including soft tissue massage, stretching and joint mobilization by a physical therapist to improve alignment, mobility and range of motion of the foot. The use of mobilization techniques also helps to modulate pain.
- Therapeutic Exercises (TE):

- Including stretching and strengthening exercises to regain range of motion and strengthen muscles of the foot and lower extremity to support, stabilize and decrease the stresses place on joint cartilage and the foot joint.
- Stretching Of Opposite Group Of Muscle And Strengthening Of Dorsiflexer’s With Evertor’s Or Invertors According To Varus Or Valgus Deformity.
- ES ( Electrical Stimulation) Mainly SF( Surge Faradic) Group Stimulation in Acuired Deformity show Good Results As Compared To Congenital Deformity.
- SF Current Are in Mostly Dorsiflexer’s With Evertor’s Or Dorsiflexer’s With Invertor’s Group Muscle According to Varus Or Valgus Deformity Are Selected.
- Taping Technique is Also Useful.
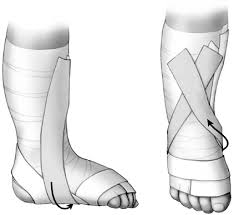 Use Of Taping Technique in CTEV
Use Of Taping Technique in CTEV
- Neuro-muscular Re-education (NMR):
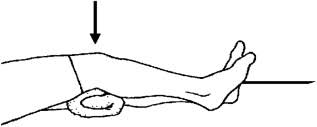
 Cast method in CTEV
Cast method in CTEV
- To restore stability, retrain the lower extremity and improve movement techniques and mechanics (for example, walking, gait training, running or jumping) of the involved lower extremity to reduce stress on the joint surfaces in daily activities.
- Rhythmic and repeated gentle manipulation.
- Strapping and plaster of Paris (POP) cast.
- Education and instructions to the mother and/or parents.
- Modalities including the use of ultrasound, electrical stimulation, ice, cold, laser and others to decrease pain and inflammation of the involved joint.
SURGICAL TREATMENT:
- Indications:
- Late presentation, after 6 months of age.
- Complementary to conservative treatment.
- Failure of conservative treatment.
- Residual deformities after conservative treatment.
- Recurrence after conservative treatment.
- Types (soft tissue and bony operations).
- Time of surgery.
- Selection of the procedure and the incision.
- Post operative care.
- Follow up.
- Complications.
- Soft tissue operations:
- Release of contractures.
- Tenotomy.
- Tendon elongation.
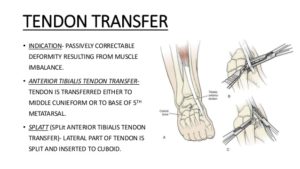
- Tendon transfer.
- Restoration of normal bony relationship.
- Bony operations:
- Indications.
- Usually accompanied with soft tissue operation.
- Types:
- Osteotomy, to correct foot deformity or int. tibial torsion.
- Wedge excision.
- Arthrodesis (usually after bone maturity) one or several joints.
- Salvage operation to restore shape.
Other Deformity Related Article :




nice
Wow, this is excellent…. Keep it up….. Good writing skills, easy and catchy with very good explanation…
its very informative article
still we need management of ctev according to age
Very nice