Diabetic Neuropathy: Physiotherapy Treatment
What is a Diabetic Neuropathy?
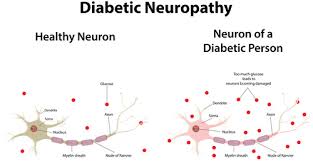
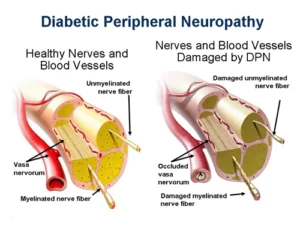
Diabetic neuropathy refers to the damage that affects the nerves of the body in people who have diabetes. It is a progressive disease, and symptoms worsen over a number of years. People who do not control their blood sugar levels and those who have high blood pressure, high blood cholesterol, or who are overweight are more susceptible.
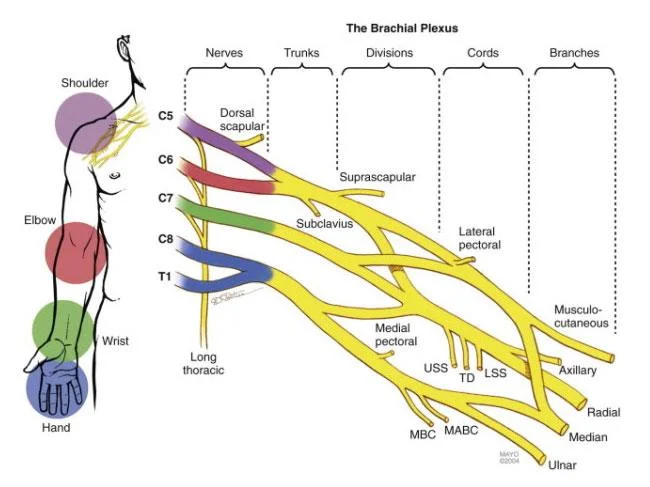
Diabetic neuropathy affects all peripheral nerves including sensory neurons, motor neurons, but rarely affects the autonomic nervous system. Therefore, diabetic neuropathy can affect all organs and systems, as all are innervated. There are several distinct syndromes based on the organ systems and members affected, but these are by no means exclusive. A patient can have sensorimotor and autonomic neuropathy or any other combination. Signs and symptoms vary depending on the nerve(s) affected and may include symptoms other than those listed. Symptoms usually develop gradually over years.
Symptoms in Diabetic Neuropathy
Symptoms may include the following:
- Trouble with balance
- Dysesthesia (abnormal sensation to a body part)
- Diarrhea
- Erectile dysfunction
- Urinary incontinence (loss of bladder control)
- Facial, mouth, and eyelid drooping
- Vision changes
- Dizziness
- Muscle weakness
- Difficulty swallowing
- Speech impairment
- Fasciculation (muscle contractions)
- Anorgasmia
- Retrograde ejaculation (in males)
Diagnosis:
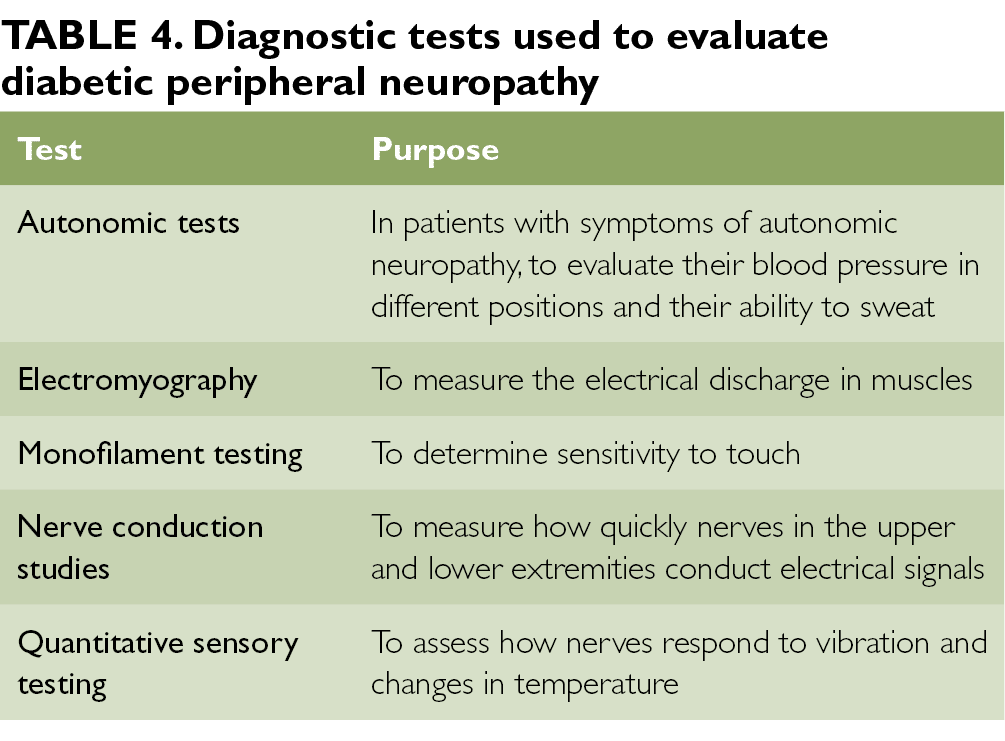
Diabetic peripheral neuropathy is the most likely diagnosis for someone with diabetes who has pain in the leg or foot, although it may also be caused by vitamin B12 deficiency or osteoarthritis.
Assesses the appearance of the feet, presence of ulceration, and ankle reflexes, the most useful physical examination findings for large fiber neuropathy are an abnormally decreased vibration perception to a 128-Hz tuning fork (likelihood ratio (LR) range, 16–35) or pressure sensation with a 5.07 Semmes-Weinstein monofilament (LR range, 11–16). Normal results on vibration testing (LR range, 0.33–0.51) or monofilament (LR range, 0.09–0.54) make large fiber peripheral neuropathy from diabetes less likely. Combinations of signs do not perform better than these 2 individual findings.
Nerve conduction tests may show reduced functioning of the peripheral nerves, but seldom correlate with the severity of diabetic peripheral neuropathy and are not appropriate as routine tests for the condition
Classification of Diabetic Neuropathy:
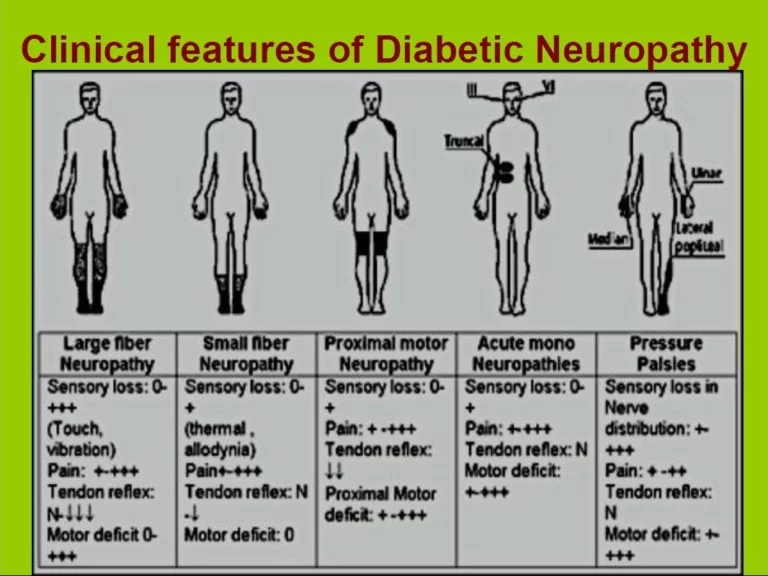
Diabetic neuropathy encompasses a series of different neuropathic syndromes which can be schematized in the following way:
Focal and multifocal neuropathies:
Mononeuropathy
Amyotrophy, radiculopathy
Multiple lesions “mononeuritis multiplex”
Entrapment (e.g. median, ulnar, peroneal)
Symmetrical neuropathies:
Acute sensory
Autonomic
Distal symmetrical polyneuropathy (DSPN), the diabetic type of which is also known as diabetic peripheral neuropathy (DPN) (most common presentation)
Diabetic neuropathy may be categorized as follows:
Sensory neuropathy occurs when nerves that detect touch and temperature are damaged. This form of neuropathy commonly affects the feet and hands.
Motor neuropathy results from damage to the nerves affecting muscle movement.
Autonomic neuropathy follows if the nerves which control involuntary actions, such as digestion or heart rate are affected.
Treatment:
Diffuse neuropathy is treated by bringing blood glucose levels under control and keeping them well-regulated. This can help to prevent problems from this diabetic complication.
Diet, exercise, or medication may be adjusted to reach these goals. Exercise can be particularly effective, helping the patient to improve circulation, strengthen muscles and lose weight.
Smoking should be stopped and the amount of alcohol consumed should be reduced. Taking regular care of your feet and skin is essential.
Nerve damage
Nerve damage in the digestive system can lead to constipation, and sometimes diabetic gastroparesis. The oesophagus may become affected, making the swallowing of food difficult. The urinary tract may also be affected, and at the worst stages, this can cause urinary incontinence.
Also, neuropathy can decrease sexual response in both men and women. The sweat glands may also be affected, and the body may not be able to control temperature properly. Furthermore, the eyes can suffer problems leaving them less sensitive to changes in light.
Proximal neuropathy
Proximal neuropathy affects the hips, buttocks and thighs, and results in weakness of the legs. This type of neuropathy occurs more regularly in type 2 diabetics and in older people. It can weaken the legs, sometimes to the extent of limiting mobility.
Focal neuropathy
Focal neuropathy is manifested in the rapid weakness of a nerve, or group of nerves, leaving the muscles weak and/or in pain.
Focal neuropathy can affect any nerve in the body, but usually occurs in the torso, leg or head. It can cause a variety of complications, including inability to focus, double vision, aching behind the eye, paralysis, lower back pain, pain in various places throughout the body. It is both unpredictable and painful, and usually affects the elderly.
Except for tight glucose control, treatments are for reducing pain and other symptoms.
Medication options for pain control include antiepileptic drugs (AEDs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and capsaicin cream.About 10% of people who use capsaicin cream have a large benefit.
A systematic review concluded that “tricyclic antidepressants and traditional anticonvulsants are better for short term pain relief than newer generation anticonvulsants.” A further analysis of previous studies showed that the agents carbamazepine, venlafaxine, duloxetine, and amitriptyline were more effective than placebo, but that comparative effectiveness between each agent is unclear.
The only three medications approved by the United States’ Food and Drug Administration for diabetic peripheral neuropathy (DPN) are the antidepressant duloxetine, the anticonvulsant pregabalin, and the long-acting opioid tapentadol ER. Before trying a systemic medication, some doctors recommend treating localized diabetic peripheral neuropathy with lidocaine patches.
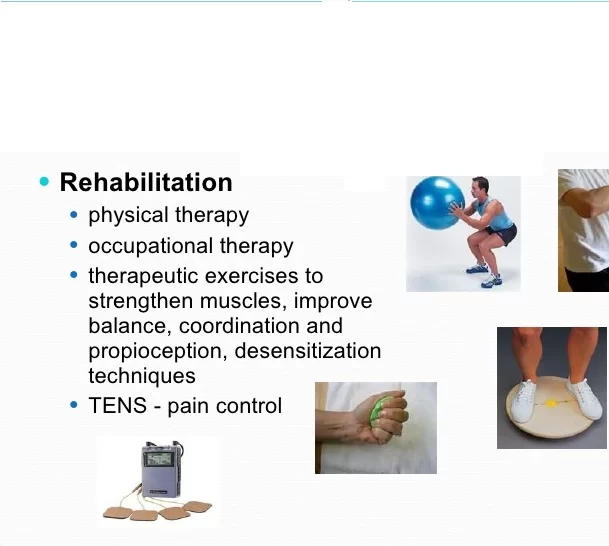
Physiotherapy treatment:
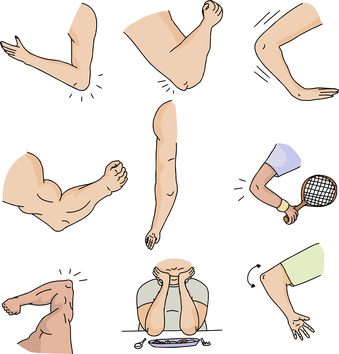
Physiotherapy treatment may help reduce dependency on pain-relieving drug therapies. Certain physiotherapy techniques can help alleviate symptoms brought on from diabetic neuropathy such as deep pain in the feet and legs, tingling or burning sensation in extremities, muscle cramps, muscle weakness, sexual dysfunction, and diabetic foot.

Transcutaneous electrical nerve stimulation (TENS) and interferential current (IFC) use a painless electric current and the physiological effects from low frequency electrical stimulation to relieve stiffness, improve mobility, relieve neuropathic pain, reduce oedema, and heal resistant foot ulcers.
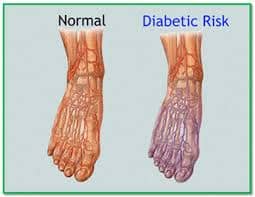
Gait training, posture training, and teaching these patients the basic principles of off-loading can help prevent and/or stabilize foot complications such as foot ulcers. Off-loading techniques can include the use of mobility aids (e.g. crutches) or foot splints. Gait re-training would also be beneficial for individuals who have lost limbs, due to diabetic neuropathy, and now wear a prosthesis.
Exercise programs, along with manual therapy, will help to prevent muscle contractures, spasms and atrophy.
These programs may include general muscle stretching to maintain muscle length and a person’s range of motion. General muscle strengthening exercises will help to maintain muscle strength and reduce muscle wasting.
Aerobic exercise such as swimming and using a stationary bicycle can help peripheral neuropathy, but activities that place excessive pressure on the feet (e.g. walking long distances, running) may be contraindicated.
Heat, therapeutic ultrasound, and hot wax are also useful for treating diabetic neuropathy.
Pelvic floor muscle exercises can improve sexual dysfunction caused by neuropathy.
Tight glucose control:
Treatment of early manifestations of sensorimotor polyneuropathy involves improving glycemic control. Tight control of blood glucose can reverse the changes of diabetic neuropathy, but only if the neuropathy and diabetes are recent in onset. Conversely, painful symptoms of neuropathy in uncontrolled diabetics tend to subside as the disease and numbness progress.
Prognosis:
The mechanisms of diabetic neuropathy are poorly understood. At present, treatment alleviates pain and can control some associated symptoms, but the process is generally progressive.
Complication:
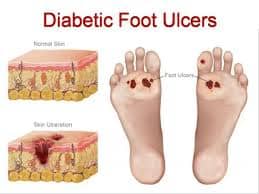
There is an increased risk of injury to the feet because of loss of sensation (diabetic foot). Small infections can progress to ulceration and this may require amputation.
FAQs
Is diabetic neuropathy curable?
Although there is no cure for diabetes, However, neuropathy symptoms are reversed with the help of Physical therapy and proper medical treatment, use of these treatments can improve painful symptoms and prevent complications.
Control blood sugar levels — An important treatment option for diabetic neuropathy is to control blood sugar levels.
What is the main cause of diabetic neuropathy?
One of the long-term side effects of uncontrolled diabetes is diabetic neuropathy. High blood glucose (sugar) levels over time might harm the tiny blood vessels that nourish your body’s nerves. This reduces important nutrients from getting to the nerves. The nerve fibers may then sustain damage or perhaps collapse as a result.
What is the first treatment for diabetic neuropathy?
Some drugs that are used to treat epilepsy also help to relieve nerve pain. Pregabalin (Lyrica) is a good place to start, according to the ADA. Another choice is gabapentin (Gralise, Neurontin). Physiotherapy Treatments are also important to relieve pain and strengthen weak muscles.




9 Comments