Emphysema
What is an Emphysema?
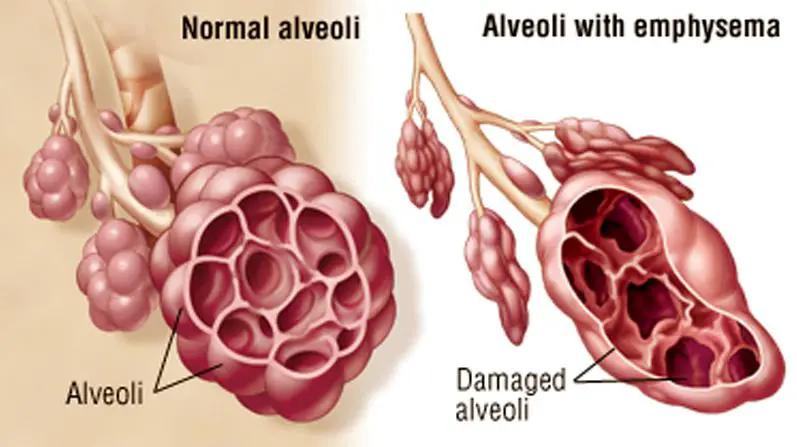
Emphysema is a chronic respiratory disease characterized by the gradual damage and deterioration of the air sacs (alveoli) in the lungs. This condition primarily affects the elasticity of the lung tissue, making it difficult for individuals with emphysema to exhale air efficiently. The main cause of emphysema is long-term exposure to irritants, particularly cigarette smoke, which triggers inflammation and the destruction of lung tissue over time.
As the disease progresses, the damaged air sacs lose their ability to recoil, leading to a reduction in the overall surface area available for gas exchange. This results in impaired airflow and reduced oxygen exchange in the lungs, leading to symptoms such as shortness of breath, chronic cough, and fatigue. Emphysema is often associated with chronic obstructive pulmonary disease (COPD), a collective term for conditions that cause airflow obstruction in the lungs.
While emphysema is typically irreversible, management strategies focus on alleviating symptoms, slowing disease progression, and improving the individual’s quality of life.
Treatment may involve lifestyle modifications, medications, pulmonary rehabilitation, and in severe cases, surgical interventions such as lung volume reduction surgery or lung transplantation. Early diagnosis and intervention are crucial in managing emphysema and mitigating its impact on respiratory function.
DEFINITION
”Emphysema is a condition of the lung characterized by Permanent dilation of the air spaces distal to the terminal bronchioles with destruction of the walls of these airways”.
It is always associated with chronic bronchitis and is difficult to distinguish the two Conditions during life.
CAUSES AND TYPES OF EMPHYSEMA
Causes and predisposing factors-
1- CONGENITAL OR PRIMARY EMPHYSEMA -This may be caused by the alfa1-antitrypsin deficiency. This is a rare inherited condition, which affects one person in 4000 and results in the complete absence of one of the key antiprotease systems in the lung. This consequence is the early development of COPD, especially if the patient is already a smoker. Although alpha1-antitrypsin deficiency is responsible for less than 1 percent of cases of COPD, Its hereditary nature means that is worth diagnosing. It should, therefore, be considered in any young COPD patient.
EMPHYSEMA may be SECONDARY to other factors, such as:
1. Obstructive airway disease -e.g. asthma, cystic fibrosis, and chronic bronchitis.
2. Occupational lung disease e. g. pneumoconiosis.
3. Compensatory to contraction of one section of the lung-e.g. fibrous collapse or removal, when the remaining lung expands to fill the space.
TYPES OF EMPHYSEMA
Emphysema is usually of the panacinar (panlobular) type.
1. CENTRIACINAR EMPHYSEMA
In centrilobular emphysema, the upper zones of the lung are usually affected. This causes gross disturbance of the ventilation /perfusion relationship since there is a relatively well-preserved blood supply to the alveoli, but the amount of oxygen reaching the capillary is decreased owing to the damage to airways proximal to the alveoli.
2. PANACINAR EMPHYSEMA
Predominantly affects the lower lobes and lower lobe involvement is more common in individuals with alfa1-antitrypsin deficiency. This has a less drastic effect on the ventilation/perfusion relationship since the blood supply in the damaged areas is decreased in proportion to the decreased ventilation in those areas.
PATHOPHYSIOLOGY
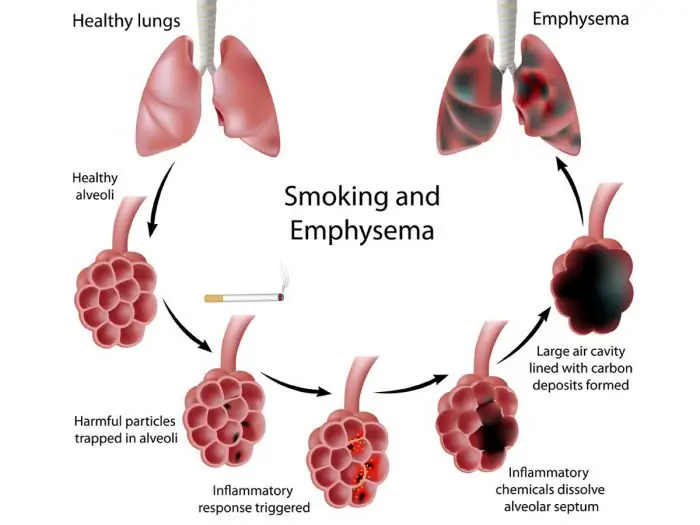
The alveoli and the small distal airways are primarily affected by the disease, followed by effects in the larger airways. Elastic recoil is usually responsible for splinting the bronchioles open. However, with emphysema, the bronchioles lose their stabilizing function therefore causing a collapse in the airways resulting in gas being trapped distally.
There is an erosion in the alveolar septa causing there to be an enlargement of the available air space in the alveoli.
There is sometimes a formation of bullae with their thin walls of diminished lung tissue.
Smoking contributes to the development of the condition initially by activating the inflammatory process. The inhaled irritants cause inflammatory cells to be released from polymorphonuclear leukocytes and alveolar macrophages to move into the lungs. Inflammatory cells are known as proteolytic enzymes, which the lungs are usually protected against due to the action of antiproteases such as alpha1-antitrypsin.
However, the irritants from smoking will have an effect on the alpha1-antitrypsin, reducing its activity. Therefore emphysema develops in this situation when the production and activity of antiprotease are not sufficient to counter the harmful effects of excess protease production. A result of this is the destruction of the alveolar walls and the breakdown of elastic tissue and collagen. The loss of alveolar tissue leads to a reduction in the surface area for gas exchange, which increases the rate of blood flow through the pulmonary capillary system.
CLINICAL FEATURE OF EMPHYSEMA
1. PROGRESSIVE DYSPNEA- Shortness of breath occurs initially on exertion, but as the disease progresses it will gradually occur after less and less activity and finally at rest.
2. RESPIRATORY PATTERN –The patient has a ‘fishlike’ inspiratory gasp, which is followed by prolonged, forced expiration usually against ‘pursed lips’.A ‘flick’ or bounce of the abdominal muscles may be seen on expiration as the outward flow of air is suddenly checked by obstruction of the airways.
3. COUGH WITH SPUTUM-This will be present if the disease is associated with chronic bronchitis or if there is an infection.
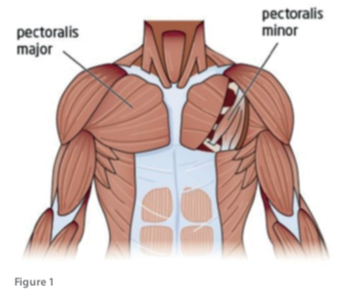
4. CHEST SHAPE-The chest becomes barrel-shaped and fixed in inspiration, with the widening of the intercostal spaces. There may also be indrawing of the lower intercostal spaces and supraclavicular fossa on inspiration. This is also associated with the difficulty of ventilating stiff lungs through narrowed airways. The ribs are elevated by the accessory muscles of respiration and there is a loss of thoracic mobility.
5. POOR POSTURES-There may be a thoracic kyphosis plus elevated and protracted shoulder girdle.
6. POLYCYTHEMIA-This may develop in response to a prolonged decrease in pao2 owing to the ventilation/perfusion imbalance.
7. CORE PULMONALE-This occurs in advanced stages of the disease.
8. LUNG FUNCTION-The FEV1/FVC ratio is usually below 70per cent. RV is increased and lung volume may exceed the predicted total lung capacity(TLC).
Diagnosis
EXAMINATION percussion notes will be normal or hyper-resonant due to air trapping. Auscultation will reveal decreased breath sounds and prolonged expiration.
The chest X-RAY shows low flat diaphragms and hyperinflation.

PROGNOSIS OF EMPHYSEMA-The patients become progressively more disabled, with death ultimately occurring from respiratory failure. Complications of emphysema are pneumothorax due to the rupture of the emphysematous bulla, and congestive cardiac failure.
MEDICAL MANAGEMENT
PRINCIPLES OF TREATMENT
1- Decrease the bronchial irritation to a minimum stop smoking, and avoid dusty, smoky, damp, or foggy atmosphere.
2- Control infections should have a supply of antibiotics at home and receive a vaccination against influenza each winter.
3- Control bronchospasm
4- Control/decrease the amount of sputum
5- Oxygen therapy
6- Long-term oxygen therapy (LTOT)
MEDICATIONS
RELIEVERS-
1- Beta2 agonists-(salbutamol and turbutalin) ,and long acting beta agonist (salmeterol and formoterol) the 2-Anticholinergics-(Ipratropium bromoide and Oxitropium bromide)
3-Xanthen derivatives -(Theophyllin and Aminophyllin)
PREVENTERS-
1- Corticosteroids- (Beclometason, Budesonide)
PHYSIOTHERAPY MANAGEMENT
The goals of treatment include:
- Relieving symptoms
- Slowing progress of the disease
- Improving exercise tolerance (ability to stay active)
- Preventing and treating complications
- Improving overall health
- COPD is not a reversible condition and has no cure yet, but conservative treatment for COPD can slow its progression (smoking cessation being the most important).
- To remove excess bronchial secretion and reduce airflow obstruction.
- To establish a coordinated pattern of breathing
- To promote relaxation and improve posture
- To improve the mobility of the thorax, shoulder girdle, and neck
- To increase exercise tolerance
- To encourage a full and active lifestyle.
Means of COPD Treatment
- POSTURAL DRAINAGE (P.D) is necessary for all patients. In chronic bronchitis, regular postural drainage should be given. In the case of acute emphysema, postural drainage is not necessary but in an infection episode, where sputum may be present PD may be needed. The optimum position must be established with individuals and advice for postural drainage at home.
Clapping and Shaking are effective over the affected lung segments and help to loosen and move the secretions to central airways during expiration. Then ask the patient to take 2-3 coughs to remove the secretions.
If the patient is unable to clear the secretions that are accumulated in the lungs, then increased ventilation and humidification by IPPB conjoint with P.D. are provided. This is very effective for patients. However, in the presence of emphysematous bullae, it is contraindicated because of the risk of causing pneumothorax.
2. ACTIVE CYCLE OF BREATHING TECHNIC
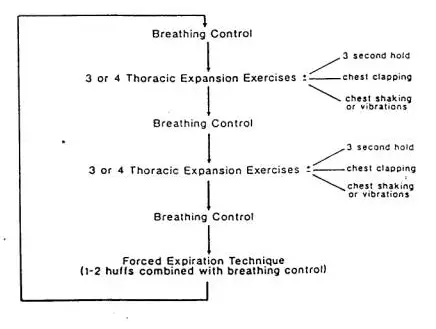
The Active Cycle of Breathing Techniques (ACBT) is an active breathing technique performed by the patient to help clear the sputum of the lungs. The ACBT is a group of techniques that use breathing exercises to improve the effectiveness of a cough, loosen and clear secretions, and improve ventilation.
ACBT consists of three main phases:
- Breathing Control
2. Deep Breathing Exercises or thoracic expansion exercises
3. Huffing OR Forced Expiratory Technique (F.E.T)
Additionally, a manual technique (MT) or positive pressure can be added if and when indicated, to create a more complex cycle to help improve the removal of secretions in the lungs.
- Breathing Control
- Breathing control is used to relax the airways and relieve the symptoms of wheezing and tightness which normally occur after coughing or breathlessness. Breathing should be performed gently through the nose using as little effort as possible. If this is not possible then breathing should be done by mouth. If it is necessary to breathe out through the mouth this should be done with ‘pursed lips breathing’.
- While performing this technique it is important to encourage the patient to use it as an opportunity to reduce any tension they may have, Encouraging the patient to close their eyes while performing Breath Control can also be beneficial in helping to promote relaxation. It is very important to use Breathing Control in between the more active exercises of ACBT as it allows for the relaxation of the airways.
- Breathing Control can also help you when you are short of breath or feeling fearful, anxious, or in a panic. The length of time spent performing Breathing Control will vary depending on how breathless the patient feels.
When using this technique with a patient as part of the ACBT the patient should be instructed to usually 6 breaths. Instructions to patient: Rest one hand on your stomach and keep your shoulders relaxed to drop down. Feel your stomach rise as you breathe in and fall when you breathe out.
Deep breathing is used to get air behind the sputum stuck in small airways:
Relax your upper chest.
Breathe in slowly and deeply.
Breathe out gently until your lungs are empty – don’t force the air out.
Repeat 3 – 4 times, if the patient feels lightheaded then it is important that they revert back to the Breathing Control portion of the cycle.
At the end of the breath in, hold the air in your lungs for 3 seconds (this is known as an inspiratory hold).
Deep breathing/thoracic expansion exercises recruit the collateral ventilatory system assisting, the movement of air distal to mucus plugs in the peripheral airways.
Deep breaths utilize collateral channels and get air behind sputum to mobilize it towards larger airways and towards the mouth. Instructions to patient:
- Relax your shoulders.
- Place both hands on either side of the ribs.
- Breathe in deeply feeling as your ribs expand.
- Breathe out gently as far as you can until your lungs feel empty.
- Deep breathing/thoracic expansion is usually repeated 4 times.
3. Huffing or FET (FORCE EXPIRATORY TECHNIQUE)
The FET is an integral part of the ACBT described by Pryor and Webber.
- A huff is exhaled through an open mouth and throat instead of coughing. Huffing moves sputum from the small airways to the larger airways, from where they are removed by coughing. Coughing alone does not remove sputum from small airways.
- Take a small-medium sized breath in
- Squeeze the breath out by contracting your tummy muscles and keep your mouth and throat open to perform a huff. This small-medium-sized huff helps with the removal of sputum in the lower reaches of the lungs.
- To remove sputum in the higher portions of the lungs take a large breath in.
- Squeeze the air out as before to perform a huff.
- Cough and expectorate any sputum. If no sputum is produced with 1 or 2 coughs, try to stop coughing by encouraging the patient to use Breathing Control, the main technique used in between the more active stages of the ACBT.
2. Take a medium-sized breath in.
Squeeze the breath out fairly hard and fast keeping mouth and throat open. Imagine trying to steam up a mirror or blow a tissue held out in front of you.
Attempt to clear sputum 2-3 times then return to breathing control (Phase one) to relax airways.
Repeat as above except for a larger breath in to remove secretions/sputum in other areas of the lungs.
In case of acute exacerbation of chronic bronchitis physiotherapy must be given vigorously. IPPB has great value in this case. It is given with a mask to improve ventilation. It is important to observe the chest wall movement and level of consciousness. The patient should be observed for any signs of drowsiness after taking the treatment. Assisted ventilation with vigorous chest shacking and postural drainage are more effective. A ventilatory mask providing controlled oxygen therapy is usually required.
3. BREATHING EXERCISE- should be given in the correct way in treatment for COPD. The main emphasis is given to diaphragmatic breathing with relaxed expiration.
Diaphragmatic breathing with decreased upper chest movements and a relaxed shoulder girdle are preferred. Expansion of basal lung segments is taught to ventilate these areas.
Pursed lip breathing with prolonged expiration is given as treatment for COPD especially in the presence of emphysematous bullae.
3. POSTURE CORRECTION Patient should be taught to attain maximal relaxation of the upper chest as well as movements of the lower chest. The main emphasis is on relaxed and controlled diaphragmatic breathing. For maintaining posture the patient should not be kept with a forward head and rounded shoulder.
4. THORACIC MOBILITY EXERCISE is given along with shoulder girdle movements. Free active exercises for the whole spine to prevent kyphosis and fixed inspiration.
Important COPD exercise in sitting is trunk turning with loose arm swinging in rotation for relaxation. It is also essential to emphasize postural awareness so that the patient practices shoulder girdle retraction and lateral rotation of the arm.
5. These patients should be as mobile and active as possible. Their exercise tolerance may be increased by gradually increasing the distances walked both on the flat and upstairs or slopes while practicing breathing control. A graduated exercise program can also be given to these patients during the later part of their stay in the hospital and should be continued at home.
6. In daily life style patients should avoid smoking and be encouraged to keep fit and eat sensibly. For gaining relaxation, swimming helps very much. Jerky and quick movements should be strictly avoided.





Eleven months ago I was diagnosed with chronic obstructive pulmonary disease (COPD). I have had asthma all my life. I have just been to the doctors and seen a senior nurse who has told me I no longer have this lung conditions because Total Cure Herbal Foundation has given me a good health while using their prescription. My breathing is totally great and I don’t feel I need the COPD inhaler anymore,i actually found the herbal foundation on guessbook i managed to give a try on the their herbs which totally save me from this chronic disease.