Motor Neurone Disease (MND)
What is a Motor Neurone Disease (MND)?
Motor neurone diseases (MND) are a group of conditions that cause the nerves in the spine and brain to progressively lose function. They are a rare but serious and incurable form of progressive neurodegeneration.
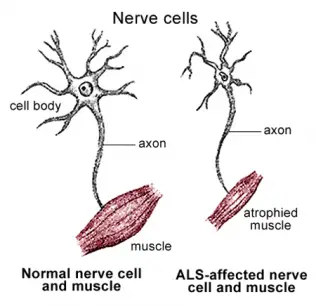
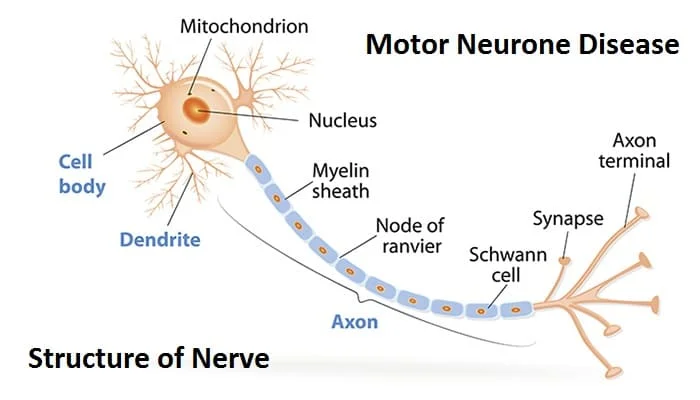
Motor neurons are nerve cells that send electrical output signals to the muscles, affecting the muscles’ ability to function.
Motor neuron disease (MND) can appear at any age, but most patients are over 40 years old at diagnosis. It affects men more than women.
Key points about motor neuron diseases.
Motor neuron diseases (MND) are a group of conditions that affect the nerve cells that send muscles to the brain.
There is a progressive weakening of all the muscles in the body, which eventually affects the ability to breathe.
Genetic, viral, and environmental issues may play a role in causing MND.
There is no cure, but supportive treatment can improve the quality of life.
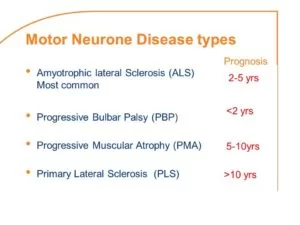
Life expectancy after diagnosis ranges from 3 years to longer than 10 years.
Classification of Motor Neurone Disease:
Motor neuron diseases affect either upper motor neurons (UMN) lower motor neurons (LMN), or both:
Type UMN degeneration LMN degeneration
Amyotrophic lateral sclerosis (ALS) Yes Yes
Hereditary spastic paraplegia (HSP) Yes No
Primary lateral sclerosis (PLS) Yes No
Progressive muscular atrophy (PMA) No Yes
Progressive bulbar palsy (PBP) No Yes, bulbar region
Pseudobulbar palsy Yes, bulbar region No
ALS, or Lou Gehrig’s disease, is the most common type, affecting muscles of the arms, legs, mouth, and respiratory system. The mean survival time is 3 to 5 years, but some people live 10 years or more beyond diagnosis with supportive care.
Progressive bulbar palsy (PBP) involves the brain stem. People with ALS often have PBP too. The condition causes frequent choking spells, and difficulty speaking, eating, and swallowing.
Progressive muscular atrophy (PMA) slowly but progressively causes muscle wasting, especially in the arms, legs, and mouth. It may be a variation of ALS.
Primary lateral sclerosis (PLS) is a rare form of MND that advances more slowly than ALS. It is not fatal, but it can affect the quality of life. In children, it is known as juvenile primary lateral sclerosis.
Spinal muscular atrophy (SMA) is an inherited MND that affects children. There are three types, all caused by an abnormal gene known as SMA1. It tends to affect the trunk, legs, and arms. The long-term outlook varies according to type.
Symptoms of Motor Neurone Disease
MND can be divided into three stages,
- early
- middle
- advanced.
Early-stage signs and symptoms

Symptoms develop slowly and can be confused with symptoms of some other unrelated neurological conditions.
Early symptoms depend upon which body system is affected first. Typical symptoms begin in one of three areas:
the arms and legs, the mouth (bulbar), or the respiratory system.
They include:
- a weakening grip, making it hard to pick up and hold things
- fatigue
- muscle pains, cramps, and twitches
- slurred and sometimes garbled speech
- weakness in the arms and legs
- increased clumsiness and stumbling
- difficulty swallowing
- trouble breathing or shortness of breath
Middle-stage signs and symptoms
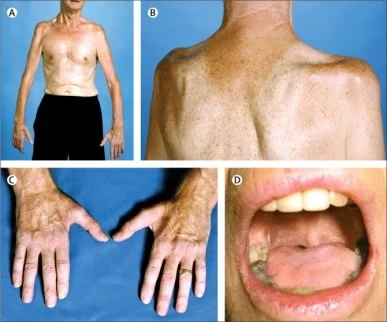
[Motor neuron mobility]
Motor neuron diseases can leave those with the disease severely restricted in mobility.
As the condition progresses, symptoms become more severe.
Muscle pain and weakness increase, and spasms and twinges worsen.
Limbs become progressively weaker.
Limb muscles start to shrink.
Movement in affected limbs becomes more difficult.
Limb muscles may become abnormally stiff.
Joint pain grows.
Eating, drinking, and swallowing become harder.
Drooling occurs, due to problems controlling saliva.
Yawning occurs, sometimes in uncontrollable bouts.
Jaw pain may result from excessive yawning.
Speech problems worsen, as muscles in the throat and mouth become weaker.
The person may show changes in personality and emotional state, with bouts of uncontrollable crying or laughing.
Previously, it was believed MND did not significantly affect brain function or memory, but studies have now shown that up to 50 percent of people with ALS have some type of brain function involvement.
This includes difficulties with memory, planning, language, behavior, and spatial relationships. Up to 15 percent of people with ALS have a form of dementia known as frontotemporal dementia (FTD).
Breathing problems may occur as the diaphragm, the main breathing muscle, deteriorates. There may be a shortage of breath, even when sleeping or resting. Ultimately, breathing assistance will be necessary.
Secondary symptoms include insomnia, anxiety, and depression.
Advanced stage signs and symptoms
Eventually, the patient will be unable to move, eat, or breathe without assistance. Without supportive care, an individual will pass away. Despite the best of care currently available, complications of the respiratory system are the most common causes of death.
Type Of Motor Neurone Disease
Causes of Motor Neurone Disease
Motor neurons send signals from the brain to the muscles and bones, and this makes the muscles move. They are involved in both conscious movements and automatic movements, such as swallowing and breathing.
Some MNDs are inherited while others happen randomly. The exact causes are unclear, but the National Institute of Neurological Diseases and Stroke (NINDS) notes that genetic, toxic, viral, and other environmental factors likely play a role.
Risk factors in MND
Heredity: In the United States (U.S.), around 1 in every 10 cases of ALS is inherited. SMA is also known to be an inherited condition.
Age: After the age of 40 years, the risk rises significantly, although it is still very small. ALS is most likely to appear between the ages of 55 and 75 years.
Sex: Men are more likely to develop an MND.
How is Diagnosis done in MND?
In the early stage, MND can be hard to diagnose, because the signs and symptoms are common to other conditions, such as multiple sclerosis (MS), an inflamed nerve, or Parkinson’s disease.
A primary care physician will normally refer the patient to a neurologist, a doctor who specializes in the diagnosis and treatment of diseases and conditions of the nervous system.
The neurologist will start with a complete history and physical exam of the neurologic system.
Other tests may be helpful.
Blood and urine tests: These analyses can rule out other conditions and detect any rise in creatinine kinase. This is produced when muscle breaks down, and it is sometimes found in the blood of patients with MND.

MRI brain scan: This cannot detect an MND, but it can help rule out other conditions, such as stroke, brain tumor, brain circulation problems, or abnormal brain structure.
Electromyography (EMG) and nerve conduction study (NCS): These are often performed together. An EMG tests the amount of electrical activity within muscles, while NCS tests the speed at which electricity moves through muscles.
Spinal tap, or lumbar puncture: This analyzes the cerebrospinal fluid, the fluid that surrounds the brain and spinal cord.
Muscle biopsy: If the doctor thinks the patient may have a muscle disease, rather than MND, a muscle biopsy may be performed.
After tests, a doctor will normally monitor the patient for some time before confirming that they have MND.
Criteria known as El Escorial criteria can help a doctor check for distinctive neurological signs, that may aid in the diagnosis of ALS.
These include:
- muscle shrinking, weakness, or twitching
- muscle stiffness or abnormal reflexes
- symptoms spreading into new muscle groups
- having no other factors that explain the symptoms
Treatment of Motor Neurone Disease (MND)
There is no cure for MND, so treatments focus on slowing the progression and maximizing patient independence and comfort.
This can include the use of breathing, feeding, mobility, and communication appliances and devices.
Rehabilitation therapy may include physical, occupational, and speech therapy.
Muscle cramps and stiffness
Muscle cramps and stiffness can be treated with physical therapy and medications, such as botulinum toxin (BTA) injections. BTA blocks the signals from the brain to the stiff muscles for about 3 months.
Baclofen, a muscle relaxer, may reduce muscle stiffness. A small pump is surgically implanted outside the body and connected to the space around the spinal cord. A regular dose of baclofen is delivered into the nervous system.
Baclofen blocks some of the nerve signals that cause spasticity. It may help with extreme yawning.
Treatment for drooling
Scopolamine, a drug for motion sickness, may help control symptoms of drooling. It is worn as a patch behind the ear.
Uncontrolled laughter or crying
Antidepressants, called serotonin reuptake inhibitors (SSRIs), may help with episodes of uncontrollable laughter or crying, known as emotional lability.
Speech, occupational, and physiotherapy
Patients with speech and communication difficulties may learn some useful techniques with a qualified speech and language therapist. As the disease advances, patients often need some communication aids.
Physiotherapy and occupational therapy can help maintain mobility and function and reduce stress.
Swallowing difficulties (dysphagia)
As eating and drinking become harder, the patient may need a percutaneous endoscopic gastrostomy (PEG), a feeding tube that is placed on the abdomen, a relatively minor procedure.
Pain Control:
A non-steroidal anti-inflammatory drug (NSAID), such as ibuprofen, will help with mild to moderate pain from muscle cramping as spasms. Drugs such as morphine can help relieve severe joint and muscle pain in the advanced stages.
Breathing problems
Respiratory muscles usually weaken gradually, but a sudden deterioration is possible.
Mechanical ventilation can help with breathing. A machine takes in air, filters it, and pumps it into the lungs often through a tracheostomy, a surgical hole in the neck that allows for assisted breathing.
Some people use complementary therapies, including special diets that are high in vitamins. These will not cure MND, but following a healthy diet can improve overall health and well-being.
Physiotherapy exercise for Motor Neurone Disease:
Every Patient with MND presents with different symptoms and requires Physiotherapy throughout the progression of the disease. Each Patient is assessed by a physiotherapist according to which Treatments are designed. Some of the physiotherapy treatments some common goals are :
Increase muscle strength through strengthening and mobilization exercises
Improve postural alignment through mobilization and strengthening
Improve balance and mobility through assessment of different seating and mobility aids plus postural re-education
Reduce muscle stiffness, spasms, and pain through stretching programmes
Reduce the risk of falls through balance work, gait re-education, and training
Increase independence and quality of life through management of positioning in bed and seating.
Physical exercise can help maintain or improve strength in the muscles not affected by MND, and maintain flexibility in muscles that are affected. It can help prevent stiffness in the joints. Physiotherapy may also help people with breathing difficulties to clear their chests and maintain lung capacity. However, people living with MND can tire very easily and find they need to conserve energy, so strenuous exercise is not normally recommended.
Several people had found physiotherapy and gentle exercise helpful, including hydrotherapy or swimming.
Chest Care in Motor Neurone Disease

Muscle weakness is a common feature in MND and can include the muscles in and around the chest affecting
breathing.
Breathing – INSPIRATION (taking air in )
– EXPIRATION ( breathing out)
The main muscle of inspiration is the diaphragm. It is located between the chest cavity and the abdomen and moves
down in inspiration against the abdominal contents. At the same time,, the ribs move up and out causing an increase in the volume of the chest cavity allowing the lungs to expand.
Expiration is the recoil of these muscles.
It is important to maintain well-aerated lungs to:-
Expand the bases of the lungs to prevent collapse therefore reducing the risk of a chest infection.
Improve the level of oxygen in the body (a lack will manifest as shortness of breath)
Remove any build-up of carbon dioxide
Improve the effectiveness of a cough which will help to remove any secretions.
Prevent stiffness of the ribs and spine.
It is important to monitor your own chest. Any deterioration should be acted on immediately via your G.P,
Physiotherapist. Consultant etc.
To maintain a clear chest you should try to incorporate breathing exercises into your daily routine i.e. first thing in the morning, before each mealtime, and before going to bed. This way you will be regularly expanding your lungs and removing any secretions.
BREATHING EXERCISES (Active Cycle of Breathing)
3 deep breaths
Normal breathing
3 deep breaths
Cough
BREATH STACKING—(for those who find it difficult to take one deep breath)
Inhale until your chest expands slightly.
Hold the breath for 2 seconds.
Breathe in again.
Hold the breath for another 2 seconds without exhaling Repeat one more time then exhale slowly through the
mouth.
Repeat the cycle 4 times.
ASSISTED COUGH – is useful if you can not generate an effective cough. It involves the carer applying pressure to
the sides of the chest to provide external pressure to the cough. (The physiotherapist will demonstrate this)
Positioning
Chest care can, and should, be performed in different positions i.e. sitting standing, side lying, reclining, etc. This will help aerate different areas of the lungs and move secretions.
Gravity can assist in moving the abdominal contents down therefore
making it easier for the diaphragm to move.
Exercise in Motor Neurone Disease

Any form of exercise that will increase the speed or depth of breathing will help to aerate and clear the lungs.
During the night our breathing becomes shallower. If the chest musculature is weakened due to MND this can lead to:
Waking during the night.
Fatigue during the day.
Dreaming
Poor appetite.
Morning headaches.
Confusion.
If this occurs NIV (Non-invasive ventilation) may be discussed.NIV assists breathing via a mask. Initially, it is used during the night and assists the patient to aerate their lungs thus improving the level of oxygen in the body. This in turn makes the patient feel better when awake.
Maintain flexibility of the chest musculature.
FAQs
What were your first signs of MND?
The first signs of MND can vary from person to person, but some common early symptoms include:
Muscle weakness, especially in the arms, legs, hands, or feet
Muscle cramps and twitches
Slurred speech or difficulty swallowing
Tripping or falling more often
Difficulty carrying or lifting objects
Difficulty with fine motor skills, such as buttoning a shirt or tying your shoes
Fatigue or tiredness
Weight loss
Difficulty controlling your emotions
What causes MND disease?
MND is generally thought to be caused by a confluence of genetic, lifestyle, and environmental factors. The majority of MND cases have no apparent cause at first. Approximately 10% of cases are “familial,” which denotes that the illness is inherited.
What are the 3 stages of MND?
There are three phases of MND: early, middle, and advanced. The symptoms of the 3 stages are different. The illnesses differ in severity and advance at varying rates.
How long can people live with MND?
The average life expectancy for people with MND is two to five years from the onset of symptoms. Although, the rate of progression of the disease varies from person to person. Some people live for many years or even decades with the disease, while others may die within a few months.
Where does MND usually start?
Approximately two-thirds of MND patients experience arm or leg pain at initially. This condition is also known as limb-onset disease. A weaker grasp, which can make it difficult to pick up or hold objects, is one of the symptoms.



Plz help me my father was in motor neuron desies plz tell me any treatment plz help me my contact number. +917041777007
I m from Somnath (Gujarat)
My brother suffering from mnd als for last 18 month please help me