Multiple sclerosis (MS): Physiotherapy Treatment
Multiple sclerosis Definition:
Multiple sclerosis (MS) is an autoimmune disease characterized by inflammation, selective demyelination, and gliosis. It can cause both acute and chronic symptoms and can result in a significant disability and impaired quality of life.MS affects approximately 400,000 persons in the united states; worldwide MS affects approximately 2.1 million people.
It was first defined by Dr. Jean Charcot in 1868 by its clinical and pathological characteristics: paralysis and the cardinal symptoms of intension tremor, scanning speech, and nystagmus later termed ”CHARCOT’S TRIAD”. using the autopsy studies he identifies the areas of hardened plaques and termed the disease sclerosis in plaques.
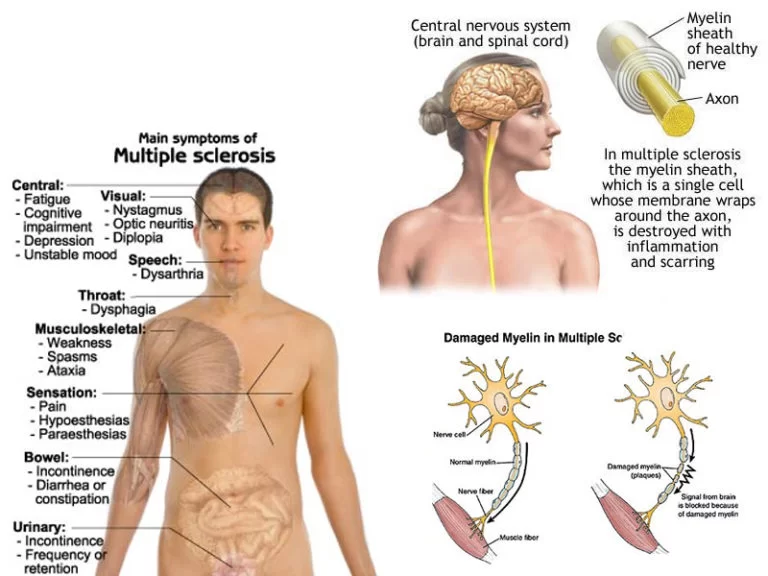
Specific symptoms can include double vision, blindness in one eye, muscle weakness, trouble with sensation, or trouble with coordination. MS takes several forms, with new symptoms either occurring in isolated attacks (relapsing forms) or building up over time (progressive forms). Between attacks, symptoms may disappear completely; however, permanent neurological problems often remain, especially as the disease advances.
Multiple sclerosis is a chronic disease that attacks the central nervous system, it affects the spinal cord, brain, and optic nerve.
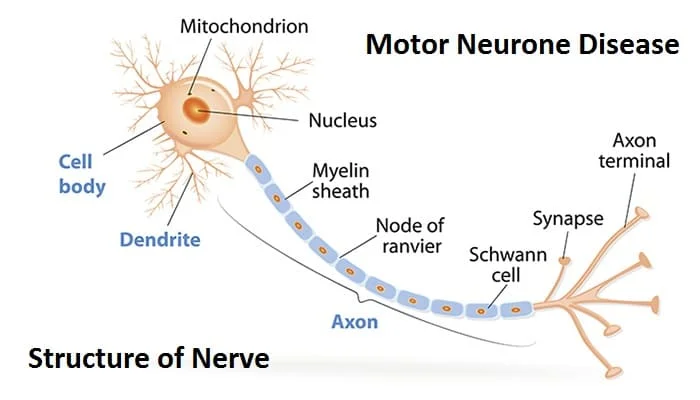
Multiple sclerosis affects the nerve cells.
What is MS ( Multiple Sclerosis)?
In the CNS, nerve fibers are surrounded by a myelin sheath, which protects them. Myelin also helps the nerves conduct electrical signals quickly and efficiently. In MS, the myelin sheath disappears in multiple areas, leaving a scar, or sclerosis.
Multiple sclerosis means “scar tissue in multiple areas.”
The areas where there is no myelin or a lack of myelin are called plaques or lesions. As the lesions get worse, nerve fibers can break or become damaged. As a result, the electrical impulses from the brain do not flow smoothly to the target nerve. When there is no myelin, the fibers cannot conduct the electrical impulses at all. The messages from the brain to the muscles cannot be transmitted.
Multiple sclerosis causes:
The cause of multiple sclerosis is unknown. It’s considered an autoimmune disease in which the body’s immune system attacks its own tissues. In the case of MS, this immune system malfunction destroys myelin (the fatty substance that coats and protects nerve fibers in the brain and spinal cord).
Myelin can be compared to the insulation coating on electrical wires. When the protective myelin is damaged and nerve fiber is exposed, the messages that travel along that nerve may be slowed or blocked. The nerve may also become damaged.
- Autoimmune response: MS is regarded as an autoimmune illness, in which the body’s immune system unintentionally attacks its own central nervous system, specifically the myelin sheath that covers and guards nerve fibers in the brain and spinal cord. Neurological symptoms and impaired nerve communication are caused by demyelination (loss of myelin).
- Hereditary predisposition: There is evidence to suggest that a person’s vulnerability to MS may be influenced by hereditary factors. An elevated risk of the disease has been linked to specific genetic variants.
- Environmental factors: Geographical location, vitamin D levels (through sunlight exposure), and viral infections are some environmental factors that have been connected to an increased risk of MS. For instance, MS is more prevalent in areas farthest from the equator where there is less solar exposure and thus less vitamin D production. In addition, some viral infections have been researched in relation to MS, although no clear causal relationship has been found.
- Smoking: It has been established that smoking is a substantial environmental risk factor for developing MS and that it can affect the level of severity of the disorder.
It isn’t clear why MS develops in some people and not others. A combination of genetics and environmental factors appears to be responsible.
Pathophysiology:
1 . In patients with MS the immune response triggers the activation of immune cells that cross the blood-brain barriers. these cells activate the autoantigens, producing” AUTO- IMMUNE CYTOTOXIC EFFECTS” within the central nervous system. demyelination slows neural transmission and causes nerves to fatigue rapidly.
2. demyelinated areas eventually become filled with fibrous astrocytes and undergo a process called ”GLIOSIS”.
DISEASE COURSE:
Most people with MS have a relapsing-remitting disease course. They experience periods of new symptoms or relapses that develop over days or weeks and usually improve partially or completely. These relapses are followed by quiet periods of disease remission that can last months or even years.
Small increases in body temperature can temporarily worsen signs and symptoms of MS, but these aren’t considered disease relapses.
About 60 to 70 percent of people with relapsing-remitting MS eventually develop a steady progression of symptoms, with or without periods of remission, known as secondary-progressive MS.
The worsening of symptoms usually includes problems with mobility and gait. The rate of disease progression varies greatly among people with secondary-progressive MS.
Some people with MS experience a gradual onset and steady progression of signs and symptoms without any relapses. This is known as primary-progressive MS.
Types of Multiple Sclerosis (MS)
There are four types of MS:
- Clinically isolated syndrome (CIS): This is a single, first episode, with symptoms lasting at least 24 hours.
2. Relapse-remitting MS (RRMS): This is the most common form, affecting around 85 percent of people with MS and involving attacks of new or increasing symptoms.
3. Primary progressive MS (PPMS): Symptoms worsen progressively, without early relapses or remissions. Around 15 percent of cases are PPMS.
4. Secondary progressive MS (SPMS): After initial episodes or relapse and remission, the disease progresses steadily.
Risk Factor:
These factors may increase your risk of developing multiple sclerosis:
Age. MS can occur at any age, but most commonly affects people between the ages of 15 and 60.
Sex. Women are about twice as likely as men are to develop MS.
Family history. If one of your parents or siblings has had MS, you are at higher risk of developing the disease.
Certain infections. A variety of viruses have been linked to MS, including Epstein-Barr, the virus that causes infectious mononucleosis.
Race. White people, particularly those of Northern European descent, are at highest risk of developing MS. People of Asian, African or Native American descent have the lowest risk.
Climate. MS is far more common in countries with temperate climates, including Canada, the northern United States, New Zealand, southeastern Australia and Europe.
Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have thyroid disease, type 1 diabetes or inflammatory bowel disease.
Smoking. Smokers who experience an initial event of symptoms that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS.
Multiple sclerosis symptoms :
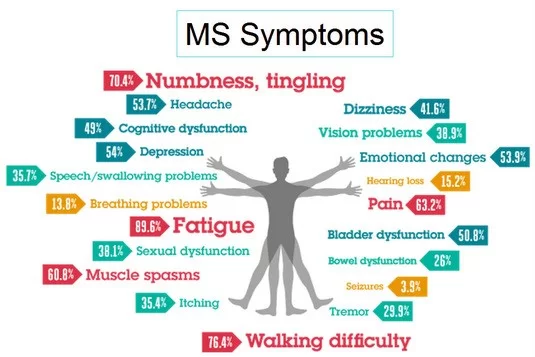
Symptoms of MS vary considerably, depending on the location of the lesion. Early symptoms typically include minor visual disturbance, and paresthesias, progressing to numbness, weakness, and fatigability.
Multiple sclerosis signs and symptoms may differ greatly from person to person and over the course of the disease depending on the location of affected nerve fibers.
They may include:
1. SENSORY- Altered sensations are far more common and can include paresthesias, and numbness of face, body, and extremities.
Numbness or weakness in one or more limbs that typically occurs on one side of your body at a time, or the legs and trunk
2. VISION -Partial or complete loss of vision, usually in one eye at a time, often with pain during eye movement
Prolonged double vision
”MARCUS GUNN PUPIL”
Scotoma
Optic neuritis
Nystagmus
INO-internuclear ophthalmoplegia produces lateral gaze palsy
Tingling or pain in parts of your body
Electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign)
Tremor, lack of coordination, or unsteady gait
Slurred speech
Fatigue
Dizziness
Headache.
trigeminal neuralgia
Paroxysmal limb pain
hyperpathia
chronic neuropathic pain
Musculoskeletal pain
Problems with bowel and bladder function
3. PAIN – Approximately 80% of patients with MS experience pain.almost half experience pain. Anxiety and fear worsen the pain symptoms.
4. MOTOR-
Weakness
Spasticity
5. FATIGUE.
6. COORDINATION AND BALANCE-Ataxia
7. GAIT AND MOBILITY-Ataxic gait
8. SPEECH AND SWALLOWING-Dysarthria
9. COGNITIVE-In MS short-term memory, attention, and concentration, information processing, executive functions, and visuospatial functions are affected.
10. DEPRESSION
11. EMOTIONAL-Pseudobulbar affect.
12. SEXUAL DYSFUNCTION.
13. UTTHOF’S SYMPTOMS
How multiple sclerosis is Diagnosed?
Tests for MS include:
- Neurological examination
2. MRI scanning
3. Evoked potential
4. Lumbar puncture
5. Other tests
The neurologist will use specific criteria to diagnose MS, known as the McDonald criteria.
1-Neurological examination
Your neurologist will ask you lots of questions about your ‘history’, meaning your health problems and symptoms, now and in the past. This helps the neurologist get a better picture of you and can help identify any other problems that may explain current symptoms.
A physical examination checks for changes or weaknesses in your eye movements, leg or hand coordination, balance, sensation, speech or reflexes. Whilst a neurologist may strongly suspect MS at this stage, a diagnosis won’t be given until other test results confirm MS.
2-Magnetic Resonance Imaging (MRI)
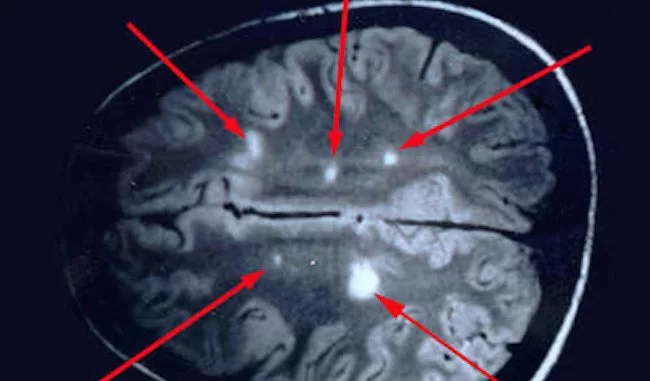
An MRI scanner uses a strong magnetic field to create a detailed image of inside your brain and spinal cord. It is very accurate and can pinpoint the exact location and size of any inflammation, damage or scarring (lesions). MRI scans confirm a diagnosis in over 90 per cent of people with MS.
To get an image of a person’s brain and spinal cord they must lie down and enter a small tunnel in the centre of the MRI scanner. The process can take between 10 and 60 minutes and is painless, though some people can feel a little claustrophobic in the scanner. The Newcastle Upon Tyne Hospitals NHS Foundation Trust has produced a video which explains what to expect when you have an MRI
3-Evoked potentials tests
This painless test involves measuring the time it takes for your brain to receive messages from your eyes, ears and skin. Small electrodes are placed on your head. These check how your brain reacts to sounds you hear in headphones, patterns you see on a screen or sensations you feel on your skin. Messages to and from your brain will be slower if MS has damaged the myelin covering around some of your nerves.
4-Lumbar puncture
This is sometimes called a spinal tap. A needle is inserted in your lower back, into the space around your spinal cord. You have a local anaesthetic for this. A small sample of the fluid around your spinal cord is taken and tested for signs of MS. People with MS often have antibodies in this fluid. Antibodies show your immune system is active in your brain and spinal cord. This is something that isn’t seen in people who don’t have MS.
People often get headaches following a lumbar puncture. The medical staff should advise you on how to manage this. Lumbar punctures are used less now that MRI scans are more common.
5-Other tests
To rule out conditions that are similar to MS, other tests may also be done. These may include blood tests to reveal certain antibodies, and inner ear tests to check your balance.
The McDonald Criteria is distinguished by incorporating clinical evaluation with magnetic resonance imaging (MRI) scans in establishing MS. But, like an earlier approach, it too requires:
Evidence of damage to the central nervous system (CNS; the brain, spinal cord and optic nerves) that is “disseminated in time,” meaning damage that occurs on different dates;
Evidence of damage “disseminated in space,” or found on two or more parts of the CNS.
Multiple sclerosis Treatment
There is no cure for multiple sclerosis. Treatment typically focuses on speeding recovery from attacks, slowing the progression of the disease and managing MS symptoms. Some people have such mild symptoms that no treatment is necessary.
Treatments for MS attacks
1-Corticosteroids, such as oral prednisone and intravenous methylprednisolone, are prescribed to reduce nerve inflammation. Side effects may include insomnia, increased blood pressure, mood swings and fluid retention.
2-Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then mixed with a protein solution (albumin) and put back into your body. Plasma exchange may be used if your symptoms are new, severe and haven’t responded to steroids.
Symptom: Sensory symptoms (parasthesias)
Numbness, tingling, pins and needles
Treatment
No treatment required unless interfering with function; medication if necessary; referral to PT/OT if necessary
Symptom: Primary pain
*Central neuropathic pain – continuous (dysesthesias)
Treatment
Medications:
tricyclic antidepressant medications (amitriptyline, nortriptyline, desipramine); antiepileptic medications (pregabalin, gabapentin)
Other:
topical appliation of capsaic acid cream;behavioral self-management (mindfulness,meditation)
hypnosis,cognitive behavior therapy
*Central neuropathic pain – intermittent (trigeminal neuralgia)
Treatment
Medications
First-line: carbamazepine
Alternate options: oxcarbazepine, lamotrigine, baclofen
Additional options with lower levels of evidence: phenytoin, clonazepam, valproic acid, intranasal lidocaine
Surgery:
radiofrequency rhizotomy; radiofrequency electrocoagulation; glycerol rhizotomy
Psychosocial Implications for each pain symptom
Clumsiness, balance problems, and loss of dexterity from sensory loss
Discomfort that is sometimes excruciating
Increase in fatigue caused by medications and interrupted sleep
NOTE: Many people are still told by doctors that MS does not cause pain, yet pain is a common symptom of MS that is distracting, depressing, and debilitating.
*Symptom: Secondary pain (musculoskeletal)
Resulting from poor posture/balance in ambulatory individuals or improper use/fitting of wheelchair
Treatment
Interventions: Referral to PT: gait and balance training; assessment of all seating (home, automobile, work, and wheelchair/scooter);
Medications:analgesics
Physiotherapy Treatment :
Physiotherapy treatment can play an essential role in keeping a patient with MS active and functional within the community. While there is no cure for multiple sclerosis, exercise appears to be beneficial at multiple levels and it may have an important role to play in delaying negative symptoms of the disease.
Exercises should be chosen according to one’s strengths and weaknesses. It is suggested that exercise therapy does have efficacy in MS.It is to state the best ’dose’ (intensity, frequency and duration) of treatment to achieve optimal beneficial effects of exercise therapy in terms of activities and participation for patients suffering from MS. There was no evidence describing harmful effects of exercise therapy for MS patients. .Exercise is consider as a safe effective means of rehabilitation.
The PT assessment should focus on posture, movement and function, carefully considering how a patient’s performance may be limited by fatigue, pain or other factors. Analyzing these results together with the proper opinion and interest of the person with MS will enable the physiotherapist to set up an individualized program. This program needs to be set up so that it can easily be performed at home. Education is also important to assist patients in managing their programs as independently as possible. Multidisciplinary treatment for MS patients may lead to positive effects.
During the EARLY STAGE of MS patients may present with minimal impairments. At this time, the PT can focus on educating the patient and family members or caregivers on disease progression and compensatory strategies to conserve energy. Physiotherapy emphasize movement outdoors especially in sunlight in order to avail the direct benefits of sunlight in MS.The recent study suggests life time sun exposure appears to reduce the risk of Multiple Sclerosis regardless of race/ethnicity. Study indicates the protective effect of sun exposure in MS is most likely mediated through immunomodulatory mechanisms,
Due to the progressive nature of the disease, those in the MODERATE STAGE might notice impairments at varying degrees and activities of daily living (ADL) may require assistance. At this middle stage,therapy should focus more on improving or maintaining motor functions through strength, endurance, flexibility, balance, respiratory training and assistive device training as well as suggesting environment modifications to the home or assessing mobility aids required to move about in the community to sustain quality of life. Informing the carers about correct postures will prevent further complications. A close collaboration between professional community carers and non-professional caregivers at home is a key factor for the successful management of rehabilitation.
Advanced stages of MS often present with multiple impairments at incresing severity compared to earlier stages. The primary goals of the PT in late stages is to maximize independence through postural and ADL training, respiratory function, safety and prevention strategies for contracture development or pressure wounds, equipment suggestions, and proper transfer techniques.

Exercise in multiple sclerosis :
Active/passive/active assisted exercises(carried with partner or with help of equipment like elastic bands);techniques like Bobath,Vojtas, and Proprioceptive Neuromuscular Techniques; carried out regularly and with sufficient intensity, have evidence of improvement in patients with MS.
The use of therapeutic corticosteroids and inactivity due to fatigue and weakness may lead to osteoporosis and pathological fractures. Weight-bearing exercises can slow down the loss of bone and muscle mass. Resistance training program is recommended for maintaining bone and muscle mass, According to Döring et al. aerobic training seems to have a positive effect on fatigue.
Aerobic exercise training with low to moderate intensity can result in the improvement of aerobic fitness and reduction of fatigue in MS patients,affected with mild or moderate disability.
BALANCE EXERCISE can improve balance.Poor postural control increases risk of falls.MS patients have increased sway in quiet stance, delayed postural perturbations, and reduced ability to move towards limits of stability. These impairments are likely causes of falls. Reduced gait speed, decreased stride length, cadence, and joint movement are observed in most studies of gait in MS. The therapist must identify several factors that may be amenable to intervention to prevent falls in people with MS. Comprehensive exercise interventions can facilitate improvements in balance impairments. Functional balance exercises can extensively impact balance, physical activity and quality of life in adults with multiple sclerosis.
MOTOR IMAGERY is increasingly used in neuro-rehabilitation in order to facilitate motor performance. Motor imagery and rhythmic auditory stimulation can be used for walking rehabilitation in MS patients. Randomized control trial studying the effects of motor imagery showed significant improvement in walking speed, walking distance, perception, and quality of living.

HIPPOTHERAPY has a positive effect on the balance of persons with multiple sclerosis and has the added benefit of enhancing quality of life. A systematic review and meta-analysis of the therapeutic effect of Horseback riding intervention shows positive physical and emotional effects of horse riding in individuals with neuromotor development and physical disabilities. Therapeutic horseback riding improved balance and gait of ambulatory patients with MS. Hippotherapy helps the rider, by providing effective sensory stimulation and rhythmic anterior and posterior swinging motion. It encourages the rider to achieve proper posture and balance.
AQUATIC EXERCISE program could have a positive effect for persons with progressive multiple sclerosis. Interventions that promote general health, improve energy levels and mental health, and faster social interaction in the presence of physical disability are beneficial for individuals with progressive multiple sclerosis. Because of the reduced impact of gravity, aquatic training allows patients with even severe paresis of the lower extremities to perform standing and moving exercises.

In MS patients, the beneficial effects of regular physical activity and exercise on mood and quality of life have been repeatedly reported. Valid data on the effect on cognitive function are hardly available.
Cognitive Behavioral Therapy (CBT) ] :
CBT have a moderately positive effect on fatigue in MS. However, this effect declines after cessation of treatment. Since the short-term effect of CBT on MS-related fatigue is positive, there is a need for more research, to develop interventions that, maintain these short-term effects in the long term.To have good results, it is best that the patient should be referred to a CBT specialist. CBT can also be an effective intervention for reducing moderate depression, over a short-term, in MS patients, which may also improve patient quality of life.
Throughout all stages of MS, PT can offer psychological support to the patient and family/caregiver.
PT Interventions for Common Symptoms of Patients with MS:
PAIN- Patients with MS often experience pain directly from the disease, secondary to medication or other symptoms, or from something completely separate. PT helps relieve pain through exercise, stretching, massage, ultrasound, postural training, or hydrotherapy.
SENSORY DEFICITS-Tapping and verbal cues during exercise and resistance training can help improve proprioception losses. Vision issues, such as blurred or double vision, often occur in patients with MS. PT can offer education on how to be safe at home and offer strategies to improve balance and coordination in dimly lit settings. PT treatment interventions for decreased sensation to light touch include education on awareness, protection, and personal care to desensitize body parts. Pressure-relieving devices are a primary prevention strategy along with proper transfer techniques and daily skin inspections for maintaining skin integrity.
FATIGUE– One of the most debilitating symptoms of MS is experienced by an overwhelming majority of patients: fatigue. PT strategies to help patients combat feelings of excessive tiredness include aerobic exercise, energy conservation, and activity pacing. Aerobic exercise activities is closely monitored by a PT to ensure a patient does not overheat but is able to work on increasing their endurance capacity which will help them be more functional throughout the day. PT’s can also teach energy conservation strategies and activity pacing to help someone sustain their daily activities by minimizing fatigue.
SPASTICITY- The physical and functional limitations spasticity leads to include a variety of impairments which can present as contractures, postural deformities, decubitus ulcers, and more. PT interventions range from cryotherapy and hydrotherapy to therapeutic exercise, stretching, range of motion activities, postural training, and electrical stimulation. A combination of therapeutic interventions is often the route taken.
Balance, Coordination, & Postural Deficits. Ataxia, postural instability, muscle spasms, and generalized muscle weakness all contribute to balance and coordination deficits. PT techniques to address these issues include postural exercise, core strengthening, rhythmic stabilization, static/dynamic balance training, aquatic therapy, proprioceptive loading, and resistance training.
Mobility Issues. Weakness, particularly in the lower extremity, balance deficits, fatigue, posture, contractures, sensation deficits, heat intolerance, among other deficits, can impede an individual’s ability to be mobile. In combination of the treatment previously described, PT’s work to help patient’s overcome their mobility limitations through locomotor and functional training.
Locomotor training focuses on increasing thigh and hip strength along with posture and balance training through walking activities. Orthotics and assistive devices are added as necessary. Functional training involves bed mobility, transfers, and developing strategies with the patient on how to be able to safely navigate around the home and out in the community.
DIETARY MODIFICATION:
Diet plays a huge role in health. Research suggests adding inflammatory fighting foods to diet can help in chronic inflammation.
Number of factors may be thought to play role in triggering inflammation- gluten and dairy products, vitamin D deficiency.A diet rich in whole fresh foods and eliminating dairy, sugar, high salt and processed food is highly recommended.
Many researchers are exploring dietary intervention approaches in MS to improve lifestyle. Probiotics may improve the health of people with MS by reducing disability and improving inflammatory and metabolic parameters according to an Iranian study.
Vitamin D supplementation helps prevention and treatment of MS. Various research studies are studying the effectiveness of vitamin D therapy in MS.
Fish oil supplementation given together with vitamins and dietary advice can improve clinical outcomes in patients with newly diagnosed MS. More research is required to assess the effectiveness of dietary interventions of omega 3 in MS and its interaction with medications used for treating MS.
Dysfunction of mitochondria is thought to play an important role in the mechanism of progression of demyelinating disorders. Observations in animal and histopathological studies suggest that dysfunctional mitochondria are important contributors to the damage and loss of both axons and neurons. The relationship between mitochondrial dysfunction and neurodegeneration in MS is explored. The Ketogenic diet has the potential to treat the neurodegenerative component of progressive MS, though more research is required in this field.
FAQs
What is the main cause of multiple sclerosis?
The immune system wrongly attacks the body’s own central nervous system, specifically the myelin sheath that encases and shields nerve fibers in the brain and spinal cord, in MS, which is categorized as an autoimmune illness. Neurological symptoms and impaired nerve communication are caused by demyelination (loss of myelin).
What are 3 warning signs of MS?
3 warning signs of MS are:
1 – a condition where one side of your body at a time has numbness or weakness in one or more of your limbs.
2 – Tingling.
Certain neck movements, especially bending the neck forward, might cause electric-shock sensations (Lhermitte sign).
3 – Coordination issues with incapacity to walk or an unsteady step.
Can I lead a normal life with MS?
Yes, a large number of MS sufferers can live happy and fruitful lives. Despite the fact that MS is a chronic and possibly life-limiting condition, improvements in medical care, rehabilitation, and support services have greatly enhanced the quality of life for many MS sufferers. Depending on the type of MS, how severe it is, and how well the patient responds to treatment, the effect of MS on a person’s life can vary greatly.
Can multiple sclerosis be cured?
The disease multiple sclerosis (MS) has no recognized cure. Since MS is regarded as a chronic and permanent disorder, it often lasts the entirety of a person’s life. Despite the fact that there is no cure, the condition is being managed and treated very effectively.
Numerous disease-modifying treatments (DMTs) have been created to assist manage symptoms, lessen the frequency and severity of relapses, and delay the course of MS. These drugs reduce inflammation in the central nervous system, a characteristic of MS, and alter the immune system’s reaction.
The quality of life for someone with MS can be greatly enhanced by supportive therapies, lifestyle changes, and medical care alone. Symptom management and functional maintenance can be assisted by physical therapy, occupational therapy, speech therapy, and other rehabilitation treatments. A person’s wellbeing can also be positively impacted by making lifestyle adjustments including exercising frequently, eating a balanced diet, managing stress, and getting enough sleep.
At what age does MS start?
Although MS can develop at any age, it typically shows up between the ages of 20 and 40. Women are affected by it two to three times more often than males. One of the most prevalent causes of neurological disability among young adults in North America, MS affects around one million people in the US.
Is MS treatable if caught early?
By delaying the onset of permanent damage and lowering the incidence of relapses, early treatment is known to benefit long-term health and well-being. Although it is best to begin MS treatment as soon as possible, delaying treatment may also have some advantages.





20 Comments