Plantar Fasciitis: Physiotherapy Treatment, Exercise
What is a Plantar Fasciitis?
Plantar fasciitis is the most common cause of heel pain. It is an inflammation in the plantar fascia, a thick band of connective tissue that runs along the sole of the foot. It often follows an injury, but in some cases, no cause can be found. Although it is not serious, it can be very difficult to get rid of.
It is a common overuse injury, commonly occurring in runners. It has been shown to be associated with increasing age, female gender, increasing BMI, and lack of exercise.
This is known as the ‘fasciitis’ part of the name because, when the plantar fascia is inflamed, it becomes hot and swollen, and can be painful when palpated. The ‘plantar’ part of the name comes from the fact that the pain is in the sole of the foot, on the bottom (plantar surface).
Definition of Planter fasciitis:
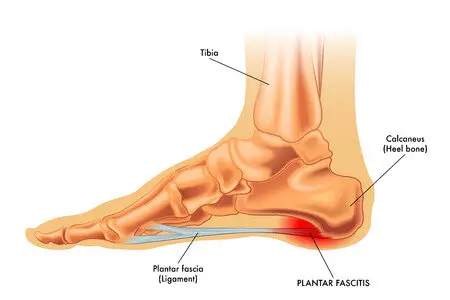
Plantar fasciitis is a disorder that results in pain in the heel and bottom of the foot. The pain is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin and may be worsened by a tight Achilles tendon. The condition typically comes on slowly. In about a third of people, both legs are affected.
Plantar fasciitis is a disorder of the insertion site of the ligament on the bone characterized by micro tears, breakdown of college, and scarring.
Signs and symptoms of Planter fasciitis:
When plantar fasciitis occurs, the pain is typically sharp and usually unilateral (70% of cases). Heel pain is worsened by bearing weight on the heel after long periods of rest. Individuals with plantar fasciitis often report their symptoms are most intense during their first steps after getting out of bed or after prolonged periods of sitting. Improvement of symptoms is usually seen with continued walking. Rare, but reported symptoms include numbness, tingling, swelling, or radiating pain. Typically there are no fevers or night sweats.
If the plantar fascia continues to be overused in the setting of plantar fasciitis, the plantar fascia can rupture. Typical signs and symptoms of plantar fascia rupture include a clicking or snapping sound, significant local swelling, and acute pain in the sole of the foot.
Risk factors:
Including overuse such as from long periods of standing, an increase in exercise, and obesity. It is also associated with inward rolling of the foot and a lifestyle that involves little exercise. While heel spurs are frequently found it is unclear if they have a role in causing the condition.
Identified risk factors for plantar fasciitis include excessive running, standing on hard surfaces for prolonged periods of time, high arches of the feet, the presence of a leg length inequality, and flat feet. The tendency of flat feet to excessively roll inward during walking or running makes them more susceptible to plantar fasciitis. Obesity is seen in 70% of individuals who present with plantar fasciitis and is an independent risk factor.
Achilles tendon tightness and inappropriate footwear have also been identified as significant risk factors.
Pathophysiology:
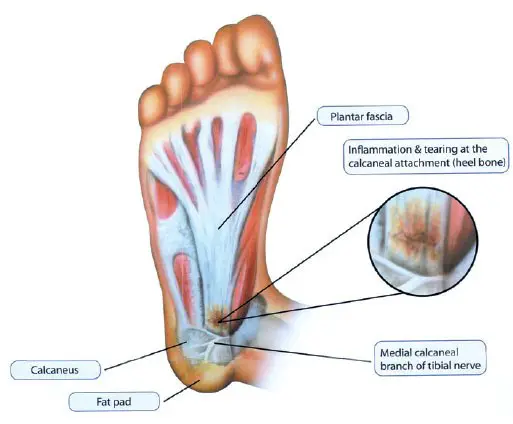
The cause of plantar fasciitis is poorly understood and is thought to likely have several contributing factors. The plantar fascia is a thick fibrous band of connective tissue that originates from the medial tubercle and the anterior aspect of the heel bone. From there, the fascia extends along the sole of the foot before inserting at the base of the toes and supporting the arch of the foot.
Originally, plantar fasciitis was believed to be an inflammatory condition of the plantar fascia. However, within the last decade, studies have observed microscopic anatomical changes indicating that plantar fasciitis is actually due to a noninflammatory structural breakdown of the plantar fascia rather than an inflammatory process.
Due to this shift in thought about the underlying mechanisms of plantar fasciitis, many in the academic community have stated the condition should be renamed plantar fasciosis. The structural breakdown of the plantar fascia is believed to be the result of repetitive microtrauma (small tears). Microscopic examination of the plantar fascia often shows myxomatous degeneration, connective tissue calcium deposits, and disorganized collagen fibers.
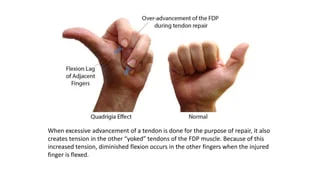
Disruptions in the plantar fascia’s normal mechanical movement during standing and walking (known as the Windlass mechanism) are thought to contribute to the development of plantar fasciitis by placing excess strain on the calcaneal tuberosity. Other studies have also suggested that plantar fasciitis is not actually due to inflamed plantar fascia, but may be a tendon injury involving the flexor digitorum brevis muscle located immediately deep into the plantar fascia.
Diagnosis:
Plantar fasciitis is diagnosed based on the history of the condition as well as the physical examination. Plantar fasciitis will have localized tenderness along the sole of the foot, most commonly at the inside arch of the heel. Usually, no further testing is necessary. X-ray testing can reveal an associated heel spur if present and rule out other causes of heel pain, such as fractures or tumors. Ultrasound imaging can also be helpful in diagnosing plantar fasciitis.
On palpation-
Tenderness is present on the bottom of the heel, closer to the midline, and mild swelling and redness. There may be a presence of nodules within the fascia.
On examination-
Active toe raise or passive dorsiflexion reproduces the symptoms.
Treatment of Planter fasciitis:
Plantar fasciitis is treated according to symptoms, the main goal is to decrease the associated symptoms such as pain, and inflammation, and avoid re-injury. Local ice pack and Hot pack with massage applications to reduce pain and inflammation.
Physical therapy treatment mainly electrotherapy pain relieving modalities with stretching exercises, is used to treat and prevent plantar fasciitis.
Anti-inflammatory medications (NSAIDs), such as ibuprofen (Advil) or cortisone injections, are often helpful. Sports running shoes with soft, cushioned soles can be helpful in reducing irritation of inflamed tissues from plantar fasciitis.
Acute stage Treatment For Plantar Fasciitis
Here are the steps patients should take as a part of Acute stage Treatment For Plantar Fasciitis-
- Rest as you can as possible- Discontinue running and walking for exercise until asymptomatic for 6 weeks. Switch to low-impact exercises like stationary bicycling, swimming, and deep water running with an alpha belt. Weight loss and modification of hard surfaces (cement) to soft surfaces (grass or cinder).
- Anti-inflammatories Medicine – Oral anti-inflammatories have variable results. A brief trial of a cyclooxygenase (COX-2) inhibitor is tried. If a response is not dramatic, this therapy is discontinued because of the possible side effects.
- Ice Pack Hot Pack with Massage- Ice Pack and Hot Pack on the area of inflammation for anti-inflammatory effects. Use ice in a paper or Styroform cup (peeled away) for 10-15 minutes, make sure to avoid frostbite.
- Low-dye Taping- Some patients obtain relief with low-dye taping, but from a practical standpoint, daily taping is difficult to maintain.
- Shoe wear Modification (Running shoes)- Flared, stable heel to help control heel stability. Firm heel counters to control the hindfoot. Soft cushioning of the heel, raising the heel 12-15 mm higher than the sole. Well-molded Achilles pad. Avoid rigid leather dress shoes that increase torque on the Achilles tendon.
- Cushioned Heel Inserts in Treatment For Plantar Fasciitis- Viscoheels. Soft cushions are placed in and out of whatever shoe the patient is wearing. Patients with abnormal biomechanics of the lower extremity, such as pes cavus or pes planus, may benefit from the eventual use of custom cushioned orthotics.
- Plantar Fascia Stretching exercise – Done 2-3 times a day, 8-10 repetitions. Done before first steps in the morning, before standing after a long period of rest. This gives a good result as Treatment For Plantar Fasciitis.

Plantar fasciitis stretching exercise:
Regular stretching exercise of the plantar fascia helps to relieve Planter fasciitis. Below we show a few simple exercises that should be done pain-free and in association with other treatment options with pain-relieving electrotherapy modalities and massage.
Stretching exercise of the plantar fascia
One way the plantar fascia can be stretched is by pulling up on the foot and toes with the hands. Hold the stretch for about 15-30 seconds. Repeat this stretch 8-10 times and aim to stretch 3 times a day
Plantar fascia stretch by rolling
The plantar fascia can be stretched by rolling the foot over a round object such as a ball, weights bar, rolling pin, or can of soup (or similar). Roll the foot repeatedly over the object, applying increasing downward pressure. Using an object that can be cooled in the freezer, such as a bottle or metal can, also applies cold therapy at the same time! This should be continued for 10 minutes per day until you can walk pain-free in the mornings.

Calf- Achilles tendon stretching exercise – A tight Achilles tendon is often implicated as an exacerbating or a causative factor in plantar fasciitis. For this reason, much attention is given to Achilles tendon stretching exercises.
Calf muscle stretching exercise:
Place the leg to be stretched behind and lean forward, ensuring the heel is kept in contact with the floor at all times. Hold the stretch for 10 to 15 seconds and repeat 3 times. This can be repeated 2 to 3 times a day and should not be painful. A stretch should be felt at the back of the lower leg. If not then move the back leg further back. A more advanced version of a calf stretch is to use a step and drop the heel down it.
Calf Stretching on a step

This stretch can be performed to further the stretch on the calf muscles and Achilles tendon. Stand on a step with the toes on the step and the heels off the back. Carefully lower the heels down below the level of the step until you feel a stretch – make sure you have something to hold on to.
Hold for 10-15 seconds.
This should be performed with the knee straight and then repeated with the knee bent to make sure you are stretching both muscles. You should feel a gentle stretch. Be careful not to overdo this one.
Strengthening of the intrinsic foot musculature-
Although the plantar fascia is inert, stress on the structure may be increased when intrinsic musculature is weak. Gripping the towel, or objects on the floor may have a re-education effect on plantar proprioception.
Chronic Stage Treatment For Plantar Fasciitis-
If the acute stage measures fail to relieve symptoms after several months, then before initiating chronic stage measures, reevaluate the patient for other causes of heel pain. Consider a bone scan if a calcaneal stress fracture is suspected. HLA-B27 and rheumatoid disease/seronegative spondyloarthropathy laboratory work-up if other systemic signs or symptoms are evident.
the steps patients should take Here are part of Chronic stage Treatment For Plantar Fasciitis-
1)Casting– In addition to acute stage measures casting has been shown to be helpful in about 50% of the patients. A short-leg walking cast can be used for 1 month with the foot placed in neutral. Evaluate success at 1 month, and consider an additional month of removable cast wear if necessary.

2)Orthotics- Patients with very high or very low arches may benefit from orthotic inserts. A less rigid, accommodative insert is applicable to a more rigid cavus type of foot, which requires more cushion and less hind foot control. A padded but rigid insert is indicated for a more unstable foot with compensatory pronation, which requires more control.
3)Cortisone steroids injection- Injection of cortisone into the area close to the planar fascia often improves pain but may weaken the plantar fascia and lead to rupture. One or possibly two steroid injections should be given in a 3-6 months period and only after failure of acute treatment measures.
4)Night Splints- A 5-degree dorsiflexion night splint has been reported to be beneficial. The splint holds the plantar fascia in a continuously tensed state. The theory behind the use of a night splint is to minimize the change of tension on the fascia that occurs with each day’s new activities.
5)Heel pads
Heel soft pads should relieve heel pain and inflammation and also help to absorb shock forces and distribute them evenly throughout the heel reducing stress.
However, We also recommend that Heel spur pads are effective in reducing foot pressure and reducing foot forces while customized can also be other options to reduce foot peak forces on both sides and are a better option compared to Heel pads.
Pre-fabricated and customized orthotics are therefore useful in distributing even pressure over the foot region through Footwear Modification
Footlogics: It helps in reducing relief from Plantar Fasciitis (heel pain and heel spurs), Achilles Tendinopathy, and also forefoot pain. The main goal is to correct over-pronation, fallen arches, and flat feet.
Insoles study: If you are suffering from heel pain, diagnosed as Severe injury, wore insoles with no other treatments added and all patients maintained their high level of physical activity throughout the study. The study shows that significant pain relief during physical activity when using insoles was found.
5) Physiotherapy Electro-Modalities Used in Treatment For Plantar Fasciitis-
- Iontophoresis
- Ultrasound therapy
- Deep friction massage
- Contrast bath
- TENS
If Symptoms seen for more than 12- 18 months require then the surgical treatment option is the last option you can select.
Surgery
To cure plantar fasciitis and ease your symptoms, the above-mentioned remedies are typically sufficient. Surgery is not often necessary. The following are the two most popular kinds of surgery:
Recession of Gastrocnemius:
To relieve strain on your plantar fascia, your surgeon will stretch your calf muscles.
Plantar fascia release:
To release part of the excess strain, your surgeon will create microscopic incisions (cuts) in your plantar fascia.
The kind of surgery required to treat plantar fasciitis will be discussed with you by your surgeon or healthcare professional.
Complications
If plantar fasciitis is not treated, it may lead to persistent heel pain that interferes with daily activities. To attempt to prevent plantar fasciitis pain, which can cause issues with your feet, knees, hips, or back, you probably need to modify the way you walk.
How to prevent Plantar Fasciitis?
It is advisable to stay away from overusing your feet in order to prevent plantar fasciitis. As a whole:
- Stretch both before and after working out.
- After strenuous work or exercise, give your feet time to relax and recover.
- Put on supportive footwear.
- On hard surfaces, avoid wearing bare feet.
- Every six to nine months, or after you’ve covered 250 to 500 miles of walking or running in them, replace your shoes.
You may not be able to avoid plantar fasciitis if you have a medical condition that increases your risk of getting it.
Prognosis
As soon as you begin treating your plantar fasciitis symptoms, you should start to see improvements. Your plantar fascia will, however, take a few weeks to many months to recover.
Try the same at-home remedies you used before if you feel better but your symptoms come back later. If your symptoms feel worse than they did previously, talk to the doctor.
FAQs
What is the best treatment for plantar fasciitis?
The best treatment for plantar fasciitis often includes a combination of rest, Physical Therapy, stretching and Strengthening exercises, orthotic inserts, and supportive footwear.
Does plantar fasciitis go away?
Although plantar fasciitis is a self-healing condition, the discomfort may not go away for over a year. If left untreated, problems may arise. It is best to consult your physician and begin non-surgical therapy as soon as possible.
Is it OK to walk with plantar fasciitis?
Walking may potentially exacerbate plantar fasciitis and need more time for therapy. Plantar fasciitis may come up even if you’re not walking alone; it can also happen if you’re not wearing the proper shoes or are overexerting yourself.
How long can plantar fasciitis last?
With home therapies, approximately 95% of patients with plantar fasciitis are able to heal within 6 months of the condition starting. Although six months can seem like a long time, they pale in comparison to the recovery period following surgery.
Can hot water reduce plantar fasciitis?
When treating foot pain, think about taking hot baths, but remember these points: Take cold and hot baths alternately. Some runners find that their problems worsen just because of the heat. If you are taking contrasting baths, immerse your heels in cold water to conclude the hot baths.
What is the root cause of plantar fasciitis?
The inflammation of the plantar fascia, a tissue in the foot utilised for walking and other foot motion, is known as plantar fasciitis. Numerous variables, such as shoe type, foot shape, overuse, and walking surface kinds, can lead to plantar fasciitis. Heel pain is the primary sign of plantar fasciitis.



15 Comments