Ulnar Nerve Injury/Palsy/Compression
Introduction
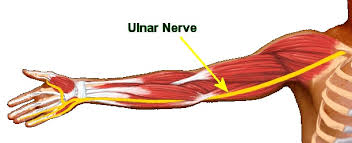
- The ulnar nerve runs all the way from the shoulder to the little finger. The ulnar nerve manages the muscles that allow to make fine movements with the fingers. It also controls some of the muscles of the forearm that allow it to grip things tightly. Unlike most of the other nerves, the ulnar nerve isn’t protected by muscle or bone throughout its course. In some areas, it’s near the surface of the skin. This means that injuries to the ulnar nerve aren’t uncommon. The ulnar nerve is what creates the shock-like sensation when you hit the funny bone in your elbow.
- Sometime lose sensation and have muscle weakness in hand if damage ulnar nerve. This is known as ulnar nerve palsy or ulnar neuropathy. This condition can affect the ability to make fine movements and perform many routine tasks. In severe cases, ulnar nerve palsy can cause muscle wasting, or atrophy, that makes the hand look like a claw. Surgery is sometimes necessary to correct this.
- Ulnar nerve compression is a condition characterized by pressure being placed on the ulnar nerve as it passes along the inner aspect of the elbow (funny bone).
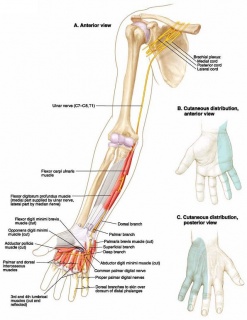
- The ulna nerve originates from several spinal nerves in the neck and travels through the upper arm, into the forearm, hand and fingers. It passes the elbow in a shallow groove situated at the inner aspect of the elbow between the medial epicondyle and olecranon. The ulna nerve is responsible for supplying sensation to the inner aspect of the forearm, the palm of the hand on the little finger side, the little finger and half of the ring finger. It is also responsible for supplying some muscles of the forearm and hand.
- Following a direct impact to the inner aspect of the elbow, the ulnar nerve may be compressed. In addition, damage and inflammation of tissue adjacent to the ulnar nerve may also place pressure on the nerve. When this occurs the condition is known as ulnar nerve compression.
- Ulnar nerve compression can occur at any age and is more common in the dominant arm especially in the case of overuse injuries. Occasionally, it may affect both arms.
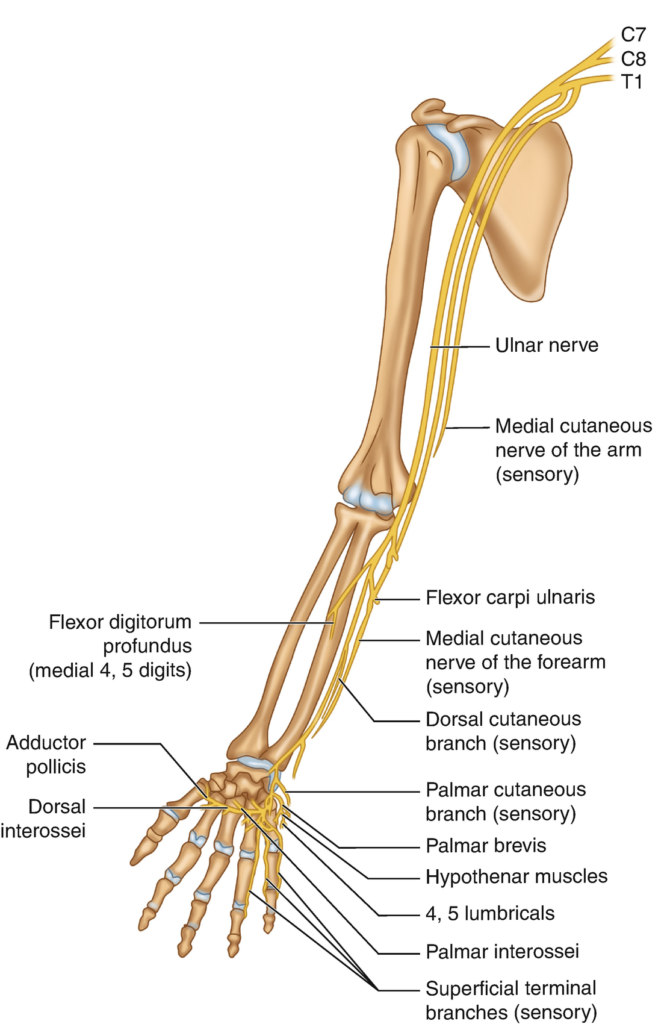
Anatomy Related to Ulnar Nerve Injury
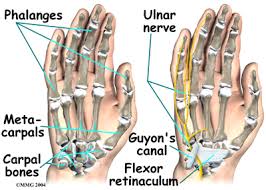
- Ulnar nerve entrapment typically occurs at two main sites: the cubital tunnel and guyon’s canal. Guyon’s canal syndrome, also known as ulnar tunnel syndrome, is much less common than cubital tunnel syndrome.
- The ulnar nerve can also be disrupted at other sites if a fracture of the humerus, radius, or ulna is sustained. Rarely, vascular pathology can lead to compression at atypical sites as well.
- Function of the nerve can be compromised distal to the site of the lesion.
COURSE OF THE ULNAR NERVE
- Originates from the C8-T1 nerve roots.
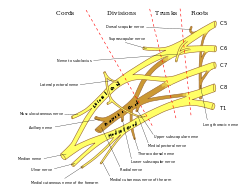
- There is a possible minor involvement of the C7 nerve root as well.
- The ulnar nerve branches off the medial cord of the brachial plexus.
- The ulnar nerve runs just medial to the axillary artery, and continues down the humerus.
- About halfway down the humerus, the ulnar nerve pierces the medial intermuscular septum, and passes back over the medial head of the triceps.
- The nerve continues around the posterior aspect of the medial epicondyle and goes through the ulnar groove.
- It then courses underneath the tendonous arch also known as the cubital tunnel (humeral-ulnar aponeurosis), which is formed by the two heads of the flexor carpi ulnaris, and enters into the anterior compartment of the forearm.
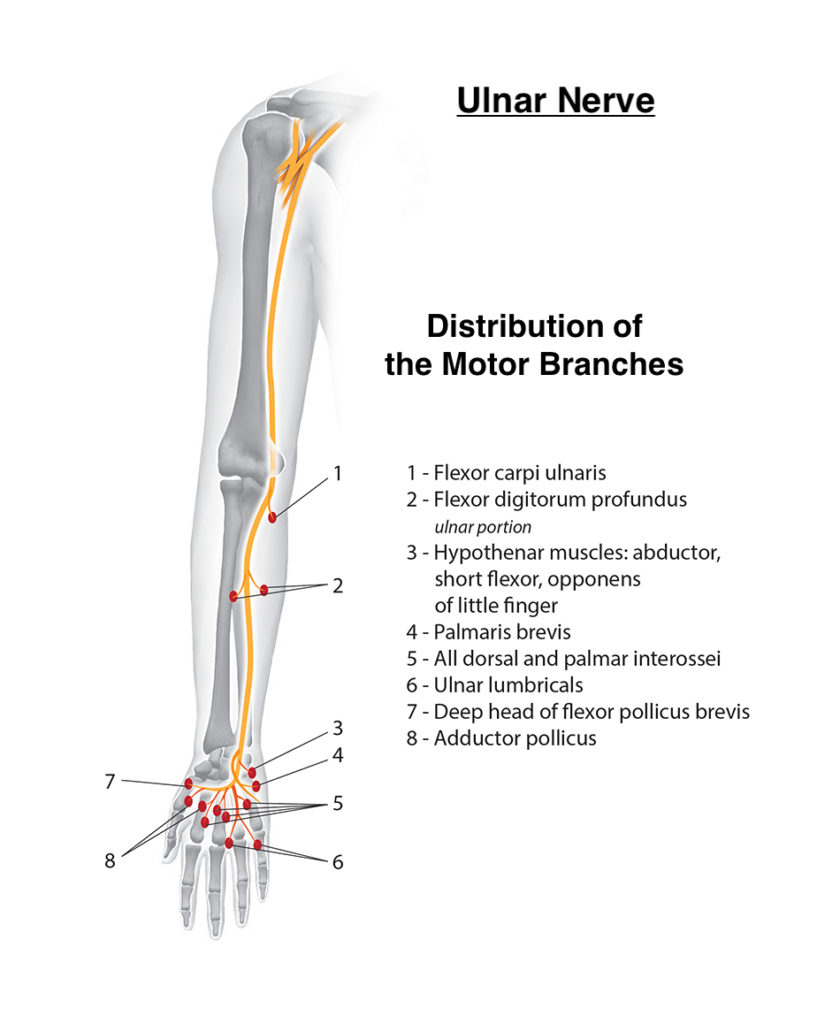
- In the forearm the nerve branches off and innervates:
- Flexor carpi ulnaris: Flexion and Adduction of wrist
- Ulnar portion of the Flexor digitorum profundus: Flexes distal phalanges at distal interphalangeal joints of digits 2-5 and assists with flexion of hand
- Dorsal cutaneous sensory branch – Supplies sensation to the dorsal aspect of the fifth finger and the dorsal medial portion of the 4th finger
- Palmar cutaneous branch of the ulnar nerve – Supplies sensation to the palmar aspect of the fifth finger and the palmar medial portion of the 4th finger.
- The ulnar nerve continues down the forearm medially and enters into the hand though the Guyon’s canal.
GUYON’S CANAL:
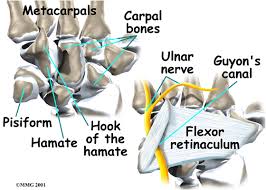
- Proximal wal: Pisiform bone.
- Distal wall: Hook of the hamate.
- Floor: Combination of the thick transverse carpal ligament, the hamate and triquetrum bones.
- Roof: Narrowed by a ligament running from pisiform to hamate.
- In the hand the ulnar nerve branches off into:
- Superficial branch of ulnar nerve – Supplies the Palmaris brevis, steadies and corrugates skin of palm to help with grip
- Deep branch of ulnar nerve – Supplies the interossei, third and fourth lumbricals, the adductor pollicis, and part of the flexor pollicis brevis.
MECHANISMS OF Ulnar Nerve Injury:
- Cubital tunnel syndrome:
- Prolonged compression of the elbow.
- Fracture.
- Overuse of elbow flexion.
- Bone pathologies or abnormalities at the elbow.
- Guyon’s Canal Syndrome:
- Biking hand hold.
- Handlebar palsy.
- Fractures.
- Bone pathologies or abnormalities at the wrist.
- Other sites of ulnar nerve compression:
- Trauma resulting in fracture/dislocation
CLINICAL PRESENTATIONS in Ulnar Nerve Injury:
- Symptoms of ulnar nerve entrapment depend on the diagnosis, or location of the lesion.
Cubital tunnel syndrome:
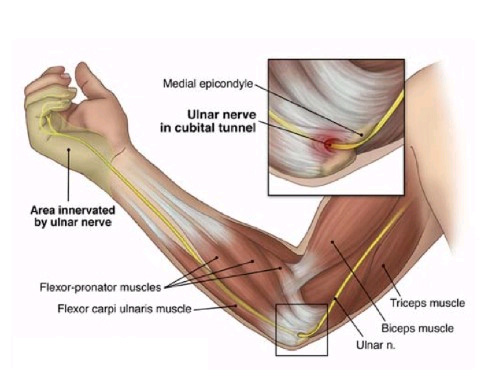
- Is considered a repetitive stress injury where the ulnar nerve becomes entrapped with the cubital tunnel which is formed by the medial epicondyle, flexor carpi ulnaris and ligaments of the olecranon process of the ulna.
- Primarily affects anyone whose motions incorporate repetitive or prolonged elbow flexion such as leaning on the elbows.
- Cubital Tunnel Syndrome can present in different grades of severity:
- Grade I: Mild symptoms
- Intermittent paresthesia.
- Minor hypoesthesia of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits.
- No motor changes.
- Grade II: Moderate and persistent symptoms
- Paresthesia.
- Hypoesthesia of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits.
- Mild weakness of ulnar innervated muscles.
- Early signs of muscular atrophy.
- Grade III: Severe symptoms
- Paresthesia.
- Obvious loss of sensation of the dorsal and palmar surfaces of the fifth and medial aspect of fourth digits.
- Significant functional and motor impairment.
- uscle atrophy of the hand intrinsics.
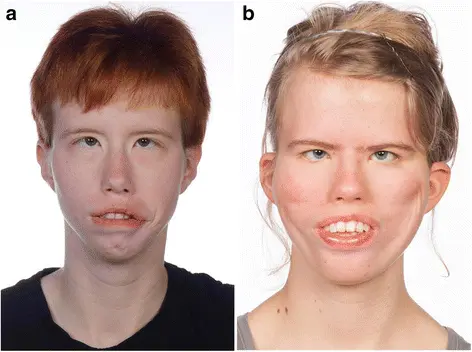
- Possible digital clawing of fourth and fifth digits (Sign of Benediction).
Guyon’s canal syndrome :
- The ulnar nerve becomes entrapped between the hook of the hamate and the transverse carpal ligament which makes up the Guyon’s canal. Guyon’s canal syndrome is considered an overuse injury which is commonly caused by direct pressure on a handlebar (ie. Bicyle handlebar, weight lifting, construction equipment) and therefore, is sometimes referred to as “handle barpalsy”. It can also result from excessive gripping, twisting, or repeated wrist and hand motions. Also, entrapment may develop if the hand is flexed and ulnar deviated for prolonged periods of time.
- Symptoms caused by this syndrome consist of:
- Muscular atrophy: Primarily the hypothenar muscles and interossei with muscle sparing of the thenar group:
- weakened finger abduction and adduction (interossei).
- weakened thumb adductor (adductor pollicis).
- Sensory loss and pain:
- May involve the palmar surface of the fifth digit and medial aspect of the fourth digit.
- Dorsum of medial aspect of the fourth finger and the dorsum of the fifth finger don’t have sensory loss.
- Ulnar Claw may present (sign of Benediction)

SYMPTOMS OF Ulnar Nerve Injury/ PALSY/ COMPRESSION:
- The symptoms associated with Ulnar palsy,
- A loss of sensation in your hand, especially in your ring and little fingers.
- A loss of coordination in your fingers.
- A tingling or burning sensation in your hand.
- Pain.
- Hand weakness that may get worse with physical activity.
- A loss of grip strength.
- The lack of strength in hand can affect daily activities, such as gripping a glass and holding a pencil.
- Over time, the lack of control and sensation can cause the muscles in hand to tighten, leading to a claw-like deformity. This usually only occurs in severe cases of ulnar nerve palsy.
- The symptoms associated with ulnar nerve compression,
- May develop suddenly or gradually over a period of time. Symptoms may include an ache or pain at the back or inner aspect of the elbow and forearm, pins and needles, numbness or a burning sensation may also be present in a similar area or into the palm on the little finger side of the hand, the little finger and half of the ring finger.
- Tenderness and an increase in symptoms may be experienced when firmly pressing or tapping the nerve at the inner aspect of the elbow.
- Occasionally, in more severe cases, weakness of the hand and fingers may also be present.
- In patients with inflammation contributing to the condition, symptoms may be worse at night or first thing in the morning.
- Occasionally, ulnar nerve compression may be associated with neck or upper back pain on the same side. In severe cases of ulnar nerve compression, obvious wasting of the muscles of the hand and forearm may be detected.
CAUSES OF Ulnar Nerve Injury/ PALSY/COMPRESSION:
- The cause of ulnar nerve palsy isn’t always known. However, damage to the ulnar nerve can occur due to:
- An illness that damages to the nerve.
- An injury to the nerve.
- Excess pressure on the nerve.
- Nerve pressure due to swelling.
- An elbow fracture or dislocation.
- Damage to the ulnar nerve is like cutting a telephone cord. The messages from your brain can’t be properly transmitted to their targets in your hand and arm nor can they be received from the hand.
- Ulnar nerve compression most commonly occurs due to a direct impact to the nerve as it passes the inner aspect of the elbow. This is particularly common during a fall onto the elbow or due to a direct impact from an object or person. This may injure and compress the nerve directly or damage adjacent tissue causing inflammation, swelling and subsequent secondary compression of the nerve. Adjacent tissue may also be damaged due to overuse (such as excessive gripping activities) again placing pressure on the ulnar nerve due to inflammation, swelling and scar tissue formation.
- Ulnar nerve compression may also occur due to excessive traction to the nerve. This is particularly common in the throwing athlete whereby their elbow is subject to excessive valgus forces in the cocking phase of throwing.
- The nerve may also be compressed as is passes through one of the muscles of the forearm (flexor carpi ulnaris) typically due to muscle over development (associated with weight training) or overuse and subsequent inflammation and scar tissue formation.
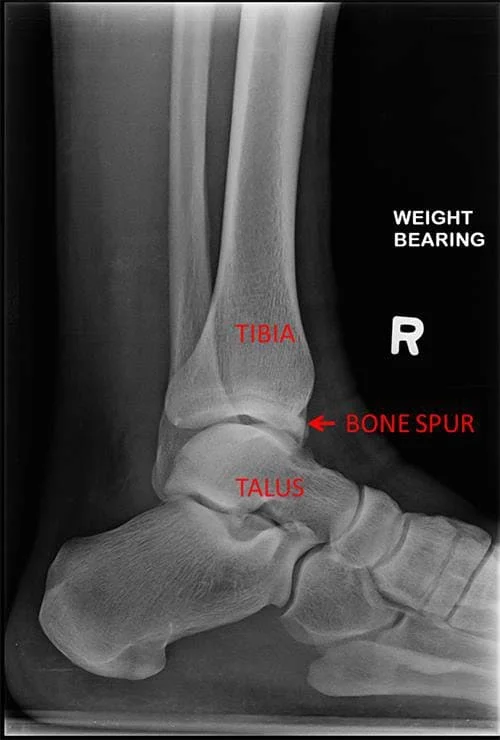
- Bony irregularities (such as spurs) within the groove between the olecranon and medial epicondyle may also contribute to ulnar nerve compression and is typically associated with overuse injuries in the throwing athlete.
- A history of wrist, elbow, shoulder, neck or upper back injury may also increase the likelihood of a patient developing this condition.
- The above factors alone or in combination with each other may contribute to the development of ulnar nerve compression.
Contributing factors to Ulnar Nerve Injury:
- Excessive training or activity (e.g. throwing sports).
- Excessive muscle hypertrophy (particularly of the flexor carpi ulnaris).
- Muscle weakness.
- Muscle tightness.
- Joint tightness.
- Poor sporting technique (e.g. throwing).
- Inadequate warm-up.
- Injury to the neck, upper back, and nerves, upper arm, elbow, or forearm.
DIAGNOSTIC PROCEDURE in Ulnar Nerve Injury:
- Blood tests.
- Imaging tests, such as a CT or MRI scan.
- Nerve conduction tests.
- X-rays.
- Cubital tunnel syndrome physical exam:
- Rule out other diagnoses which could refer to the elbow (listed below).
- ROM of the elbow (flexion may be limited secondary to pain).
- MMT of the ulnar nerve muscles innervated distal to the cubital tunnel.
- Sensory exam of the cutaneous ulnar nerve distribution (palmar 5th digit and ulnar side of the 4th digit may be diminished).
- Upper limb tension test for the ulnar nerve.
- Special test includes,
- Tinnel’s sign at the cubital tunnel.
- Elbow flexion test.
- Pressure provocative test.
- Card test.
- Guyon’s cannal syndrome physical exam:
- Rule out other diagnoses which could refer to the elbow (listed below) .
- ROM of the wrist and digits.
- MMT of ulnar nerve muscles innervated distal to Guyon’s Canal.
- Sensory exam of the ulnar nerve cutaneous distributiondistal to Guyon’s Canal.
- Muscle wasting of intrinsic hand muscles.
- Special tests includes,
- Card test.
- Froment’s sign.
- Tinnel’s sign at guyon’s canal.
- Ulnar neurodynamic test (ULTT3) may increase the patient’s symptoms.
TREATMENTS in Ulnar Nerve Injury:
- Over-the-counter pain relievers.
- Medications to reduce nerve spasms, such as gabapentin, carbamazepine or phenytoin.
- Corticosteroids to reduce inflammation.
- A splint to support the hand and reduce painful symptoms.
- Physical therapy to increase muscle strength and function.
- Occupational therapy to minimize further injury.
- Doctor may also recommend surgery if the nerve damage is extensive, extremely painful, or not improving.
- Surgery is also often necessary if you find it difficult to go about your daily life due to the nerve palsy.
- One surgical procedure involves tendon transfer. During a tendon transfer surgery, a functioning tendon is moved from its original bone attachment to a new one. This can help restore muscle function, allowing you to perform routine activities once again.
- The results of surgery are generally good, but nerves heal slowly, so a full restoration of wrist and hand function can take months. Even after surgery, you may still have a loss of sensation and movement in your hands.
Physiotherapy Treatment and Exercise:
- Soft tissue massage
- Dry needling
- Electrotherapy
- Bracing or splinting
- Joint mobilization
- Neural mobilization
- Ice or heat treatment
- Progressive exercises to improve flexibility and strength
- Education
- Training and activity modification advice
- Technique correction
- Anti-inflammatory advice
- Devising an appropriate return to activity plan
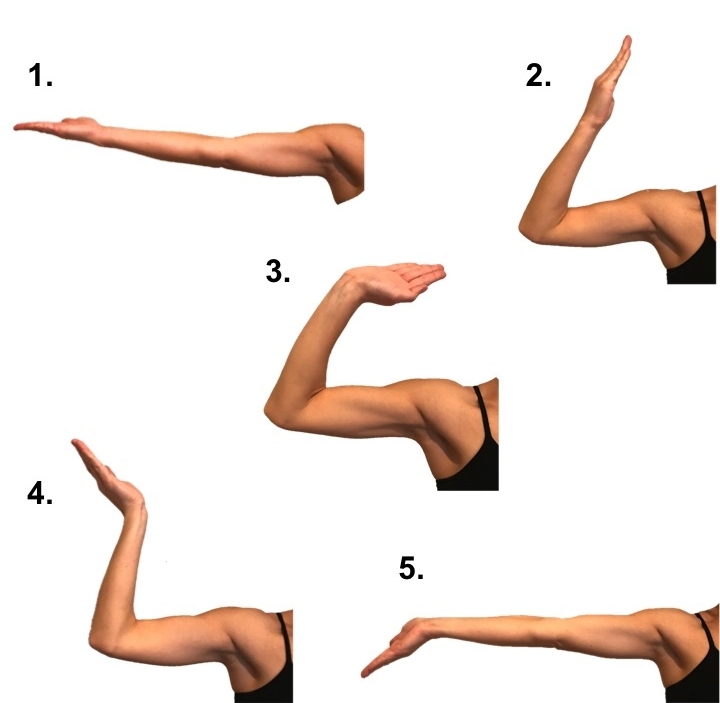
- Exercises such as,
- Wrist flexor stretch.
- Wrist and finger extensor stretch.
- Elbow flexibility exercises.
- Elbow strengthening exercises.
Electrical Stimulation :
ES Plays important role in nerve injury , When Patient comes with Nerve Injury Require RD Test according to which IG/SF Current is applied. if RD Test is Positive then Galvanic Current and if Negative Then Faradic Current or Mix of IG/SF is decided upon test result and recovery Progress Mostly Faradic current is more useful for strengthening of muscle from Grade 1 to 3 after that only exercise require.
Strengthening Exercise :
Strengthening Exercise is Depends Upon MMT of Muscle supplied By Ulnar Nerve and according to which strengthening exercise planning is done. If Muscle grade is “zero” – Passive movement , Grade 1 to 3 – Active Assisted Strengthening Exercise And After 3 to 5 Grade Require weight Cuff to strengthen Muscle.
Stretching Exercise :
Muscle which are tight require careful inspection , Make list of tight muscle according to which stretching exercise are performed and stretching also depends upon grade of muscle. if muscle is below 3 grade power then stretching exercise repetition time reduced and muscle grade above 3 grade require enough stretching exercise.





I have ulnar nerve palsy. Please help me
Hii