Lower Extremity Functional Scale (LEFS)
Introduction
The Lower Extremity Functional Scale (LEFS) is a patient-reported outcome measure (PROM) used to assess lower extremity function in individuals with musculoskeletal disorders or injuries. It is a 20-item questionnaire that evaluates activities of daily living (ADLs) related to standing, walking, balance, and stair climbing.
Each item is scored on a 4-point scale ranging from “0” (unable to do) to “3” (can do without difficulty). Higher scores denote better function. The total score runs from 0 to 80.
One outcome measure used to evaluate the functional status of people with impairments to their lower extremities is the LEFS.
This technique, which covers walking, stair climbing, balancing, and standing, aids in assessing the physical function and disability associated with lower extremity deficits. This is used for measuring a person’s development over time in research projects as well as clinical settings due to its dependability.
The Lower Extremity Functional Scale aids in measuring the degree of difficulty people encounter when carrying out tasks. The score goes from 20 (easy) to 80 (impossible to act).
The Lower Extremity Functional Scale (LEFS) is a valuable tool for assessing lower extremity function and evaluating the effectiveness of treatment interventions in patients with musculoskeletal disorders. It serves several important purposes in clinical practice and research:
- Measuring Functional Impact: The LEFS quantifies an individual’s ability to perform everyday activities that rely on lower extremity function. This includes tasks like walking, climbing stairs, maintaining balance, and sitting down. By assessing these activities, the LEFS provides insight into how a lower extremity condition affects a person’s daily life.
- Tracking Functional Progress: The LEFS allows clinicians to monitor changes in functional status over time. This is particularly useful for evaluating the effectiveness of rehabilitation interventions or tracking the progression of chronic conditions. By comparing LEFS scores at different points in time, clinicians can determine whether a patient is improving, maintaining, or experiencing functional decline.
- Evaluating Treatment Effectiveness: The LEFS serves as a tool to assess the effectiveness of different treatment interventions, such as physical therapy, occupational therapy, or assistive devices. By comparing LEFS scores before and after treatment, clinicians can determine whether a particular intervention has led to improvements in functional status.
- Informing Patient Care Decisions: LEFS scores provide valuable information that guides patient care decisions. For instance, clinicians can use LEFS scores to determine the level of assistance a patient may need with daily activities, make informed decisions about discharge planning, and establish functional goals for rehabilitation.
- Assessing Quality of Life: The LEFS indirectly reflects an individual’s quality of life by measuring their ability to perform essential daily tasks. A person’s ability to independently perform these activities contributes significantly to their overall well-being and quality of life.
Overall, the LEFS is a versatile and valuable tool for clinicians and researchers working with individuals with lower extremity impairments. It provides a standardized and reliable measure of functional status, allowing for informed decision-making, treatment evaluation, and patient care planning.
Who Can Use This Lower Extremity Functional Scale Printable?
Medical professionals can examine the functional state of patients with lower extremity impairments with the help of the convenient LEFS instrument. It is appropriate for the following and can be used in a range of clinical settings:
- Physical therapists
- Occupational therapists
- specialists in rehabilitation
- Medical professionals
- Other medical specialists
In clinical studies, LEFS can also be used by researchers to assess the effectiveness of interventions and therapies.
Objective LEFS
The Lower Extremity Functional Scale (LEFS) is a self-reported questionnaire that measures a person’s ability to perform activities of daily living (ADLs) related to lower extremity function. It is a 20-item questionnaire that is scored on a 4-point scale, with higher scores indicating better function. The LEFS is a reliable and valid measure of lower extremity function and has been used in a variety of research studies.
The objective of the LEFS:
- To assess a person’s lower extremity function and ability to perform ADLs.
- To track changes in lower extremity function over time.
- To evaluate the effectiveness of treatment interventions.
The LEFS is a valuable tool for clinicians and researchers working with individuals with lower extremity impairments. It is a reliable, valid, and easy-to-administer measure that can be used to assess functional status, track progress, and evaluate treatment effectiveness.
Here is a table summarizing the objective of the LEFS:
| Objective | Description |
|---|---|
| Assess lower extremity function | The LEFS can be used to assess a person’s ability to perform activities of daily living (ADLs) related to lower extremity function. |
| Track changes in lower extremity function over time | The LEFS can be used to track changes in a person’s lower extremity function over time. This can be helpful for monitoring the progress of treatment or rehabilitation. |
| Evaluate the effectiveness of treatment interventions | The LEFS can be used to evaluate the effectiveness of treatment interventions for lower extremity impairments |
Scoring the LEFS
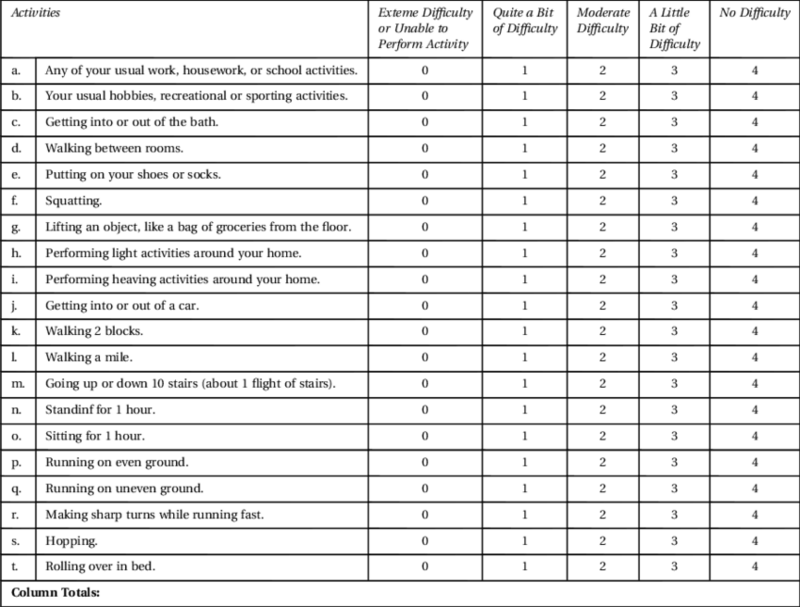
The Lower Extremity Functional Scale (LEFS) is scored by assigning points to each item based on the patient’s self-reported ability to perform the activity. Each item is graded on a four-point scale:
- 0: Unable to do
- 1: Can do with assistance
- 2: Can do with some difficulty
- 3: Can do without difficulty
The final score is determined by adding the scores from all 20 items. The maximum possible score is 80, and higher scores indicate better functional status.
Here is an example of how to score the LEFS:
| Item | Patient’s Response | Score |
|---|---|---|
| Everything you typically do for a job, household, or school. | I can do all of my usual work and activities without difficulty. | 3 |
| Your usual hobbies, recreational, or sporting activities. | I can do most of my usual hobbies, but I have some difficulty with strenuous activities. | 2 |
| Getting into or out of the bath. | I can get into and out of the bath without assistance, but I need to be careful. | 2 |
| Walking on a flat surface. | I can walk on a flat surface for more than 10 minutes without stopping. | 3 |
| Walking downstairs. | I can walk up stairs without assistance, but I need to take one step at a time and hold onto the railing. | 2 |
| I can walk downstairs without assistance, but I need to be careful and take my time. | I can walk upstairs without assistance, but I need to take one step at a time and hold onto the railing. | 2 |
| Standing for more than 10 minutes. | I can stand for more than 10 minutes without discomfort. | 3 |
| Sitting for more than 10 minutes. | I can sit for more than 10 minutes without discomfort. | 3 |
| Getting out of a chair. | I can get out of a chair without assistance. | 3 |
| Putting on shoes and socks. | I can put on my shoes and socks without assistance. | 3 |
| Getting dressed. | I can get dressed without assistance. | 3 |
| Bathing. | I can bathe myself without assistance. | 3 |
| Eating. | I can eat without assistance. | 3 |
| Toileting. | I can use the toilet without assistance. | 3 |
| Getting in and out of bed. | I can get in and out of bed without assistance. | 3 |
In this example, the patient’s total score is 70. This indicates that the patient has good functional status, but they may have some difficulty with strenuous activities.
Interpretation of LEFS scores
The interpretation of LEFS scores is as follows:
| Score | Interpretation |
|---|---|
| 80-76 | Very good functional status |
| 75-71 | Good functional status |
| 70-66 | Fair functional status |
| 65-61 | Poor functional status |
| 60 or less | Very poor functional status |
A score of 80-76 indicates that the patient has a very good functional status and can perform most activities of daily living (ADLs) without difficulty. A score of 75-71 indicates that the patient has good functional status and can perform most ADLs without assistance, but may have some difficulty with more strenuous activities. A score of 70-66 indicates that the patient has fair functional status and can perform most ADLs, but may need some assistance with more difficult tasks. A score of 65-61 indicates that the patient has poor functional status and may need assistance with many ADLs. A score of 60 or less indicates that the patient has a very poor functional status and may need assistance with most ADLs.
It is important to keep in mind that these are just general guidelines, and the interpretation of an LEFS score may vary depending on the individual’s age, gender, and overall health status. For example, an older adult may be considered to have good functional status with a score of 70, while a younger adult may be considered to have fair functional status with the same score.
Here are some additional factors to consider when interpreting LEFS scores:
- The patient’s self-report: The LEFS is a self-report measure, which means that it is based on the patient’s own perception of their functional status. This can be affected by a number of factors, such as pain, muscle fatigue, and motivation.
- The patient’s baseline functional status: The LEFS is not a standardized measure, so it is important to consider the patient’s baseline functional status before interpreting their score. A patient who starts with poor functional status may have a more difficult time improving their score, even if they make significant progress.
- The patient’s goals: The interpretation of a LEFS score will also depend on the patient’s goals. For example, a patient who is trying to return to work may need a higher score than a patient who is trying to maintain their independence at home.
Overall, LEFS scores are a valuable tool for assessing lower extremity function and tracking progress over time. However, it is important to interpret scores with caution and to consider all of the factors that may affect a patient’s functional status.
Why Are Physical Therapists So Following This Assessment?
Physical therapists frequently use LEFS as an assessment tool since it is:
Dependable and accurate
A tool used by physicians and physical therapists to assess a patient’s ability to do lower-body tasks is the LEFS. It can be applied again and again with consistent outcomes. Additionally, it measures the functional state of people with impairments to their lower extremities correctly.
Responsive to change
It can identify both little and major changes in your patient’s functional status over time because it is responsive to change. Because of this, it’s the perfect instrument for monitoring development and assessing how well therapies are working.
Method of Use LEFS
Here are the steps on how to administer the Lower Extremity Functional Scale (LEFS):
- Obtain Patient Consent: Before administering the LEFS, obtain informed consent from the patient. Explain the purpose of the questionnaire and assure them that their responses will be kept confidential.
- Provide Instructions: Provide clear instructions to the patient. Inform them that the LEFS assesses their ability to perform everyday activities related to their lower extremities. Read each question aloud and clarify any doubts they may have.
- Self-Report Responses: Allow the patient to self-report their responses to each question. Encourage them to answer honestly based on their current level of functioning.
- Scoring: Each item on the LEFS is scored on a 4-point scale ranging from 0 (unable to do) to 3 (can do without difficulty). Assign the appropriate score based on the patient’s response.
- Total Score: Calculate the total score by summing the scores for all 20 items. A higher total score indicates better functional status.
- Interpretation: Interpret the total score using the established guidelines:
- 80-76: Very good functional status
- 75-71: Good functional status
- 70-66: Fair functional status
- 65-61: Poor functional status
- 60 or less: Very poor functional status
- Documentation: Document the patient’s responses, scores, and interpretation in their medical record.
- Consider repeating the LEFS periodically to track changes in functional status over time.
How to Apply This Functional Scale for Lower Extremity
There are twenty questions on this LEFS worksheet to assist you in assessing the lower extremity functionality of your patient. To get started, take these actions:
Step 1: Get the evaluation
By using the provided link, you can obtain a copy of the LEFS assessment. Print it off or save a digital copy for your patient after you’ve downloaded it.
Step 2: Provide a copy to your patient.
Give the patient a copy of the LEFS and describe its operation to them. Inform them that the answers to each question range from 0 to 4, where 0 represents no difficulty and 4 represents complete incapacity to complete the task.
Step 3: Request that your patient finish the evaluation
Allow your patient enough time and space to finish the LEFS on their own. Motivate them to provide truthful and precise answers to every question.
Step Four: Determine the final score
Add together all the numbers to determine your patient’s final score after they have finished the assessment. Scores go from 0 to 80, where 0 denotes no difficulty and 80 denotes complete incapacity to complete the task.
Step Five: properly store the worksheet
If you want to guarantee that you can access the worksheet again if necessary, make sure to store it correctly. It might be a good idea to record your patient’s LEFS score in their health record.
Here are some additional tips for administering the LEFS:
- Ensure a quiet and private environment for the patient to complete the questionnaire.
- To minimize misunderstandings, use basic and plain language.
- Provide assistance or clarification if the patient has difficulty understanding the questions.
- Respect the patient’s pace and allow them sufficient time to respond to each question.
- Thank the patient for their cooperation and participation
What Is The Typical Use of A LEFS?
When assessing a person’s functional level and monitoring their advancement over time, lower extremity impairment sufferers usually use the LEFS. It can be applied to:
Determine the functional status of those who have impairments to their lower extremities.
This scale assesses your patient’s ability to do lower-body tasks such as standing and walking. It can assist you in determining the degree of difficulty your patient experiences with each task.
Monitor development over time
The lower extremity functional scale can be used to track how well physical therapy interventions are working. It makes it possible to comprehend how your patient reacts to their treatments better.
Assess each person’s degree of difficulty
The LEFS can offer helpful details about a person’s challenges with particular activities. This can assist you in taking a deeper look at your patient’s day-to-day functioning and helping to customize the best interventions.
Clinical Applications of the LEFS
The Lower Extremity Functional Scale (LEFS) is a versatile tool that can be used in a variety of clinical settings. Some specific applications of the LEFS include:
Pre- and post-operative assessment of orthopedic patients:
- The LEFS can be used to assess the functional status of patients before and after surgery to determine whether there has been an improvement in their ability to perform everyday activities.
Monitoring progress in patients with chronic lower extremity impairments:
- The LEFS can be used to monitor the progress of patients with chronic conditions such as osteoarthritis, rheumatoid arthritis, and multiple sclerosis. This can help to determine whether treatment is effective and whether adjustments to treatment are needed.
Evaluating the effectiveness of rehabilitation interventions:
- The LEFS can be used to evaluate the effectiveness of different rehabilitation interventions, such as physical therapy, occupational therapy, and orthotics.
Making decisions about discharge planning and home care:
- The LEFS can be used to assess the needs of patients who are being discharged from the hospital or who are being transitioned to home care. This information can help to ensure that patients have the resources they need to care for themselves at home.
Here are some examples of how the LEFS can be used in clinical practice:
A physical therapist can use the LEFS to:
- Assess a patient’s functional status before starting a new treatment program.
- Track a patient’s progress over time to determine whether the treatment program is effective.
- Make decisions about the goals of the treatment program.
An occupational therapist can use the LEFS to:
- Assess a patient’s ability to perform everyday activities, such as cooking, bathing, and dressing.
- Help a patient develop strategies for coping with their lower extremity impairments and maintaining their independence.
- Make recommendations for home modifications or assistive devices.
A physician can use the LEFS to:
- Monitor the progress of a patient with a chronic lower extremity condition.
- Evaluate the effectiveness of different treatment options.
- Make decisions about whether to refer a patient to a physical therapist or occupational therapist.
Overall, the LEFS is a valuable tool for clinicians working with individuals with lower extremity impairments. It can be used to assess functional status, track progress, evaluate treatment effectiveness, and make informed decisions about patient care.
Benefits of the LEFS
Healthcare workers can take advantage of several advantages provided by LEFS, such as:
Give an indication of the degree of hardship a person is facing.
The LEFS can offer insightful information about a person’s challenges with particular activities. This can assist you in developing the most effective solutions for your patient’s requirements by helping you better understand how they manage their everyday lives.
It is applicable in numerous clinical situations.
A useful assessment tool for medical professionals to assess the functional status of patients with lower extremity deficits is the Lower Extremity Functional Scale. It can be applied in therapeutic applications such as occupational therapy, physical therapy, rehabilitation, and routine doctor visits.
Assist in customizing therapies that are most advantageous to each individual
Despite forgoing a more thorough examination of your patient’s reactions to their therapies, LEFS allows you to track the efficacy of your interventions.
totally digital
There is no need for you to print off or carry around paper copies of this LEFS worksheet because it is fully digital. If your patient is unable to attend their in-person appointment, you can give them a digital copy of the worksheet and ask them to complete it.
The LEFS is a valuable tool for clinicians working with individuals with lower extremity impairments. It has several benefits, including:
- Reliability and validity: The LEFS has been shown to be a reliable and valid measure of lower extremity function, meaning that it produces consistent results and measures what it is intended to measure.
- Sensitivity to change: The LEFS is sensitive to changes in functional status over time, meaning that it can detect small changes in a person’s ability to perform everyday activities.
- Ease of administration: The LEFS is a brief and easy-to-administer questionnaire, making it a practical tool for use in clinical settings.
- Patient-centeredness: The LEFS is a patient-centered measure that reflects the patient’s own perception of their functional status, which is important because the patient is the best source of information about how their condition is affecting their life.
These benefits make the LEFS a valuable tool for assessing lower extremity function, tracking progress, evaluating treatment effectiveness, and making informed decisions about patient care.
Here is a table summarizing the benefits of the LEFS:
| Benefit | Description |
|---|---|
| Reliability and validity | The LEFS has been shown to be a reliable and valid measure of lower extremity function. |
| Sensitivity to change | The LEFS is sensitive to changes in functional status over time. |
| Ease of administration | The LEFS is a brief and easy-to-administer questionnaire. |
| Patient-centeredness | The LEFS is a patient-centered measure that reflects the patient’s own perception of their functional status |
Reliability LEFS
The Lower Extremity Functional Scale (LEFS) is a well-established and reliable tool for assessing lower extremity function in individuals with musculoskeletal disorders or injuries. It has been shown to have strong internal consistency, test-retest reliability, and inter-rater reliability.
Internal Consistency:
The LEFS has excellent internal consistency, with Cronbach’s alpha coefficients ranging from 0.93 to 0.96 across different studies. This means that the items on the LEFS are all measuring a similar concept and that the scale is consistent in its ability to assess lower extremity function.
Test-Retest Reliability:
The LEFS has good test-retest reliability, with intraclass correlation coefficients (ICC) ranging from 0.79 to 0.89. This means that the LEFS is consistent in its ability to measure lower extremity function over time, even when administered at different times.
Inter-Rater Reliability:
The LEFS has good inter-rater reliability, with weighted kappa coefficients ranging from 0.78 to 0.88. This means that different raters are consistent in their scoring of the LEFS, even when assessing the same patients.
Overall, the LEFS is a reliable tool for assessing lower extremity function. It has strong internal consistency, good test-retest reliability, and good inter-rater reliability. This means that the LEFS can be used to track changes in lower extremity function over time and that it can be used to compare the functional status of different patients.
Here is a table summarizing the reliability of the LEFS:
| Type of Reliability | Coefficient Range | Interpretation |
|---|---|---|
| Internal Consistency | 0.93 to 0.96 | Excellent |
| Test-Retest Reliability | 0.79 to 0.89 | Good |
| Inter-Rater Reliability | 0.78 to 0.88 | Good |
Validity OF LEFS
The Lower Extremity Functional Scale (LEFS) is a valid tool for assessing lower extremity function in individuals with musculoskeletal disorders or injuries. It has been shown to have strong content validity, construct validity, and criterion validity.
Content Validity:
The LEFS has good content validity, meaning that the items on the scale are relevant to the concept of lower extremity function and cover a broad range of activities of daily living (ADLs) that require lower extremity function.
Construct Validity:
The LEFS has strong construct validity, meaning that it correlates well with other measures of lower extremity function, such as gait speed, balance, and muscle strength. It also correlates well with measures of health-related quality of life (HRQoL), indicating that it captures the impact of lower extremity function on daily life.
Criterion Validity:
The LEFS has good criterion validity, meaning that it can distinguish between individuals with different levels of lower extremity function. For example, it can discriminate between patients with different diagnoses, such as osteoarthritis, rheumatoid arthritis, and low back pain. It can also discriminate between patients with different levels of severity of the same condition.
Overall, the LEFS is a valid tool for assessing lower extremity function. It has strong content validity, construct validity, and criterion validity. This means that the LEFS accurately measures what it is intended to measure and that it is a useful tool for clinicians and researchers working with individuals with lower extremity impairments.
Here is a table summarizing the validity of the LEFS:
| Type of Validity | Evidence | Interpretation |
|---|---|---|
| Content Validity | Item selection process, expert review | Good |
| Construct Validity | Correlations with other measures of lower extremity function and HRQoL | Strong |
| Criterion Validity | Ability to discriminate between individuals with different levels of lower extremity function | Good |
Responsiveness OF LEFS
The Lower Extremity Functional Scale (LEFS) is a responsive tool for assessing changes in lower extremity function over time. It has been shown to be sensitive to changes in function in individuals with musculoskeletal disorders or injuries.
Responsiveness to Change:
The LEFS has good responsiveness to change, meaning that it can detect small improvements or declines in lower extremity function over time. This has been demonstrated in numerous studies, including a meta-analysis that found that the LEFS had an average standardized response mean (SRM) of 0.83.
Responsiveness to Different Treatment Interventions:
The LEFS has been shown to be responsive to a variety of treatment interventions, including physical therapy, occupational therapy, and medication. This means that the LEFS can be used to evaluate the effectiveness of these interventions in improving lower extremity function.
Responsiveness to Different Patient Populations:
The LEFS has been shown to be responsive to changes in lower extremity function in a variety of patient populations, including individuals with osteoarthritis, rheumatoid arthritis, and low back pain. This means that the LEFS can be used to assess the functional status of a wide range of patients with lower extremity impairments.
Overall, the LEFS is a responsive tool for assessing changes in lower extremity function over time. It has been shown to be sensitive to small improvements or declines in function, and it has been demonstrated to be responsive to a variety of treatment interventions and patient populations.
Here is a table summarizing the responsiveness of the LEFS:
| Type of Change | SRM | Interpretation |
|---|---|---|
| Change in LEFS score | 0.83 | Good |
| Response to treatment interventions | Yes | Yes |
| Response to different patient populations | Yes | Yes |
Limitations of the LEFS
The LEFS is a valuable tool for assessing lower extremity function, but it does have some limitations. These limitations include:
- Self-report measure: The LEFS is a self-report measure, which means that it is based on the patient’s own perception of their functional status. This can be affected by a number of factors, such as pain, fatigue, and motivation.
- Limited assessment of function: The LEFS does not assess all aspects of lower extremity function, such as strength, balance, and coordination. This means that the LEFS may not be able to fully capture the functional limitations of a person with a lower extremity impairment.
- Limited sensitivity in high-functioning individuals: The LEFS may not be sensitive enough to detect small changes in functional status in high-functioning individuals. This means that the LEFS may not be able to accurately measure the progress of a person who is already close to their maximum level of function.
Despite these limitations, the LEFS is a valuable tool for clinicians working with individuals with lower extremity impairments. It is a reliable, valid, and easy-to-administer measure that can be used to assess functional status, track progress, evaluate treatment effectiveness, and make informed decisions about patient care.
Here is a table summarizing the limitations of the LEFS:
| Limitation | Description |
|---|---|
| Self-report measure | The LEFS is a self-report measure, which means that it is subject to the biases of the individual completing the questionnaire. |
| Limited assessment of function | The LEFS does not assess all aspects of lower extremity function, such as strength, balance, and coordination. |
| Limited sensitivity in high-functioning individuals | The LEFS may not be sensitive enough to detect small changes in functional status in high-functioning individuals |
Results: The LEFS scores had strong test-retest reliability (R =.94 [95% lower limit confidence interval (CI) =.89]). Correlations between the LEFS and the SF-36 physical function subscale and physical component score were.80 (95% CI =.73) and.64 (95% CI =.54), respectively. The association between the prognosis rating of change and the LEFS was stronger than the link between the prognostic rating of change and the SF-36 physical function score. The possible error associated with a LEFS score at a particular moment in time is +/-5.3 scale points (90% CI), the smallest detectable change is 9 scale points (90% CI), and the smallest clinically significant difference is 9 scale points (90% CI).
Contraindication of LEFS
Here are some of the contraindications of the LEFS:
- Cognitive impairment: The LEFS is a self-report questionnaire, which means that it relies on the patient’s ability to understand and complete the questionnaire. Patients with cognitive impairment may not be able to complete the questionnaire accurately.
- Severe pain: Pain can affect a patient’s ability to perform activities of daily living (ADLs). If a patient is in severe pain, they may not be able to complete the LEFS accurately.
- Language barriers: The LEFS is available in several languages, but it is important to ensure that the patient is able to understand the questions and instructions in their native language.
If you are concerned about any of the contraindications of the LEFS, please consult with your doctor or physical therapist. They can help you determine if the LEFS is an appropriate tool for you to use.
Adaptation in different countries LEFS
The Lower Extremity Functional Scale (LEFS) has been adapted and translated into multiple languages for use in different countries. This allows clinicians and researchers to assess lower extremity function in individuals from diverse backgrounds and compare results across different populations.
Here are some examples of countries where the LEFS has been adapted:
- Brazil: The Brazilian Portuguese version of the LEFS has been shown to have good reliability, validity, and responsiveness. It has been used in studies of individuals with osteoarthritis, rheumatoid arthritis, and low back pain.
- China: The Chinese version of the LEFS has also been shown to have good reliability, validity, and responsiveness. It has been used in studies of individuals with hip osteoarthritis, knee osteoarthritis, and stroke.
- France: The French version of the LEFS has been used in studies of individuals with osteoarthritis, rheumatoid arthritis, and fibromyalgia.
- Germany: The German version of the LEFS has been used in studies of individuals with osteoarthritis, rheumatoid arthritis, and low back pain.
- Japan: The Japanese version of the LEFS has been used in studies of individuals with hip osteoarthritis, knee osteoarthritis, and stroke.
- Spain: The Spanish version of the LEFS has been used in studies of individuals with osteoarthritis, rheumatoid arthritis, and fibromyalgia.
- Turkey: The Turkish version of the LEFS has been used in studies of individuals with hip osteoarthritis, knee osteoarthritis, and low back pain.
The adaptation of the LEFS into different languages is an important step in ensuring that it can be used effectively in a global context. By making the LEFS accessible to clinicians and researchers in different countries, we can improve the assessment of lower extremity function and the development of effective treatment interventions for individuals with musculoskeletal disorders or injuries.
Conclusion of LEFS
The Lower Extremity Functional Scale (LEFS) is a well-established and effective tool for assessing lower extremity function in individuals with musculoskeletal disorders or injuries. It is a brief and user-friendly questionnaire that can be easily administered and scored, making it a practical tool for clinical settings. The LEFS has been shown to be reliable and valid in measuring lower extremity function in a variety of populations and across different musculoskeletal conditions. It is sensitive to change over time, allowing for the assessment of progress and the evaluation of treatment effectiveness. Additionally, the LEFS is applicable to a wide range of patients, including those with cognitive impairments or language barriers.
Despite its strengths, the LEFS is not without its limitations. As a self-report measure, it is subject to the biases of the individual completing the questionnaire. Additionally, the LEFS does not assess all aspects of lower extremity function, and it may not be sensitive to subtle changes in function. However, these limitations are outweighed by the LEFS’s many benefits, making it a valuable tool for clinicians working with individuals with lower extremity impairments.
In summary, the LEFS is a reliable, valid, and user-friendly tool for assessing lower extremity function. It is a valuable tool for clinicians, researchers, and patients in evaluating the impact of musculoskeletal conditions on daily life and tracking progress over time.
FAQs
The functional status scale is rated in what way?
The Functional Status Score for the Intensive Care Unit (FSS-ICU) is a 5-item performance-based assessment that uses an 8-point ordinal scale to assess physical function in ICU patients.
The functional status scale is rated in what?
The Functional Status Score for the Intensive Care Unit (FSS-ICU) is a 5-item performance-based assessment that uses an 8-point ordinal scale to assess physical function in ICU patients.
What exactly is a lower limb stability test?
For balance, the patient stands on one leg with no upper extremity support, hands at hips or out to the side. The patient squats to a maximum depth on one leg and then returns to standing. During the squatting effort, the patient is not permitted to brace the opposing leg against the squatting leg or the floor.
What is a representation of a functional status?
The underlying structure of functional status is a complicated hierarchy that begins with particular physical actions (e.g., lifting, walking) and progresses to higher-level activities (e.g., performing vocational and social duties).
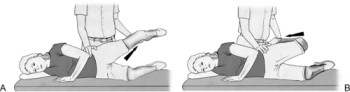
How is lower extremity tone measured?
Tones for testing:
Allow the patient to ‘go floppy’ with their legs.
Rotate the ‘floppy’ leg both inside and externally. Look for any signs of increased or decreased tone.
Then, using one of your hands, elevate the knee off the bed. Take note of if the ankle also rises off the bed, indicating increasing tone.
What are the eight elements of a functional assessment?
Vision and hearing, mobility, continence, nutrition, mental status (cognition and affect), affect, home environment, social support, and ADL-IADL are all components of functional evaluation. ADLs (activities of daily living) are fundamental tasks such as transferring, ambulating, bathing, and so on.
What is the most effective functional evaluation tool?
THE BEST TOOL: The Katz Index of Independence in Activities of Daily Living, often known as the Katz ADL, is the best tool for assessing functional status since it measures the client’s capacity to undertake activities of daily living independently.
References
- Lower Extremity Functional Scale (LEFS). (n.d.). Physiopedia. https://www.physio-pedia.com/Lower_Extremity_Functional_Scale_(LEFS)#/media/File:Lower_Extremity_Functional_Scale.png
- The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. (1999, April 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/10201543/
- Lower Extremity Functional Scale (LEFS) & Example | Free PDF Download. (n.d.). https://www.carepatron.com/templates/lower-extremity-functional-scale