Vitamin B2 (Riboflavin)
Introduction
Vitamin B2, or riboflavin, is a vitamin that can be purchased as a dietary supplement or found in food.
It is necessary for the synthesis of flavin adenine dinucleotide and flavin mononucleotide, the two main coenzymes.
These coenzymes play a role in normal growth and development, cellular respiration, energy metabolism, and antibody formation.
The metabolism of folate, vitamin B6, and niacin also depends on the coenzymes. When taken orally, riboflavin is indicated to treat corneal thinning and may lower the frequency of adult migraine headaches.
In most cases, deficits in other vitamins and nutrients coexist with rare cases of riboflavin insufficiency.
Oral supplements or injections can be used to treat or prevent it. Water-soluble vitamin riboflavin does not store it when taken in excess of nutritional needs; instead, it is either promptly expelled in urine, giving it a brilliant yellow tinge, or it is not absorbed at all.
Meat, poultry, eggs, dairy products, green vegetables, mushrooms, and almonds are natural sources of riboflavin.
Certain nations mandate adding it to grains. In 1920, riboflavin was found; it was separated in 1933 and synthesized for the first time in 1935.
It is a water-soluble, crystalline powder that is yellow-orange in color when it is pure and solid. It serves as a food coloring agent in addition to being a vitamin.
Animals do not engage in biosynthesis; only plants, fungi, and microbes do. Originally produced using a chemical technique, commercial riboflavin production now uses a fermentation process involving genetically modified bacteria and fungus strains.
Definition
One of the B vitamins is riboflavin or vitamin B2. It is a water-soluble vitamin.
Whereas riboflavin is a single chemical component, folate and vitamin B6 are found in numerous chemically related forms known as vitamers.
It is an initiating molecule for the synthesis of the coenzymes flavin adenine dinucleotide (FAD) and flavin mononucleotide (FMN, also called riboflavin-5′-phosphate).
The more prevalent kind of flavin, known as FAD, has been shown to bind to 75% of the flavin-dependent protein-encoded genes in the flavoproteome, or the genome of all species, and to function as a co-enzyme for 84% of the flavoproteins expressed in humans.
Riboflavin is a yellow-orange crystalline powder with a faint odor and harsh taste when it is pure and solid.
It is somewhat soluble in alcohols and soluble in polar solvents like water and aqueous sodium chloride solutions.
Organic solvents that are non-polar or only slightly polar, like acetone, benzene, or chloroform, do not dissolve it.
If riboflavin is not exposed to light, it remains heat stable whether it is in solution or in dry storage as a powder. It releases hazardous fumes containing nitric oxide when heated to break down.
Functions
The synthesis of FMN and FAD, two important coenzymes, depends on riboflavin. These coenzymes play a role in the synthesis of antibodies.
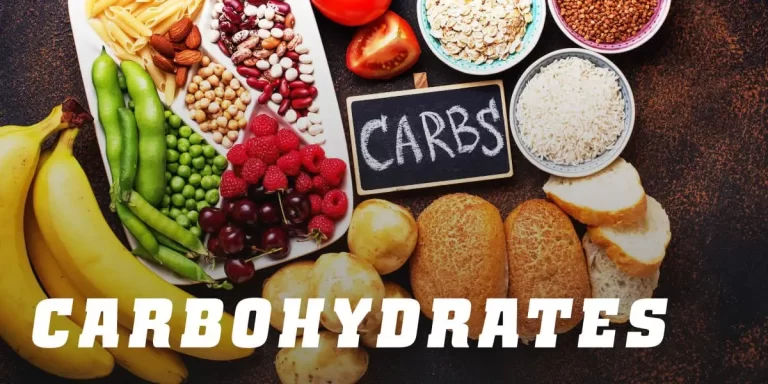
Growth and development, respiration of cells, and energy metabolism. The metabolism of lipids, proteins, and carbohydrates depends on riboflavin.
Tryptophan is converted by FAD to niacin (vitamin B3), while FMN is needed to convert vitamin B6 to the coenzyme pyridoxal 5′-phosphate.
Homocysteine levels rise in riboflavin-deficient individuals, increasing the risk of cardiovascular illnesses. Riboflavin is involved in sustaining normal circulation levels of homocysteine.
Redox Reactions
The processes called redox reactions entail the transfer of electrons. About 70–80 flavoenzymes in humans (and hundreds more in all organisms, including those encoded by the genomes of bacteria, fungi, and archaea) are responsible for one- or two-electron redox reactions.
That takes advantage of the ability of flavins to be converted between oxidized, half-reduced, and fully reduced forms.
These reactions are supported by the flavin coenzymes. The activity of glutathione reductase, a crucial enzyme in the synthesis of the endogenous antioxidant glutathione, likewise depends on FAD.
Micronutrient Metabolism
The metabolism of niacin, vitamin B6, and folate is mediated by riboflavin, FMN, and FAD. The FAD-dependent enzyme kynurenine 3-monooxygenase is involved in the synthesis of the niacin-containing coenzymes, NAD and NADP, from tryptophan.
A diet low in riboflavin can lead to a reduction in NAD and NADP synthesis, which in turn can exacerbate niacin insufficiency.
Transformation of vitamin B6 into pyridoxal, its coenzyme FMN is necessary for the enzyme pyridoxine 5′-phosphate oxidase, which is involved in 5′-phosphate synthase.
FAD is necessary for 5,10-methylenetetrahydrofolate reductase, an enzyme involved in the metabolism of folate, to convert homocysteine into the amino acid methionine.
The dietary mineral iron, which is necessary for the synthesis of hemoglobin and red blood cells, appears to be metabolized more poorly in cases of riboflavin shortage.
The efficiency of iron supplementation for the treatment of iron-insufficiency anemia is increased when riboflavin deficiency is alleviated in individuals who are deficient in both riboflavin and iron.
Synthesis
Biosynthesis
Animals do not engage in biosynthesis; only plants, fungi, and microbes do. Guanosine triphosphate and ribulose 5-phosphate are the metabolic precursors of riboflavin.
L-3,4-dihydroxy-2-butanone-4-phosphate is the result of the former’s conversion, whereas 5-amino-6-(D-tributylamine)uracil is the end product of the latter’s chain of transformations.
Next, in reaction EC 2.5.1.78, these two molecules serve as the substrates for the penultimate step in the route, which is catalyzed by the enzyme lumazine synthase.
The enzyme riboflavin synthase combines two molecules of 6,7-dimethyl-8-ribityllumazine in a dismutation process during the last stage of biosynthesis.
One molecule of 5-amino-6-(D-tributylamine) uracil and one molecule of riboflavin are produced as a result. The latter is recycled back to the sequence’s initial reaction.
The enzymes riboflavin kinase and FAD synthetase, which function consecutively, convert riboflavin to the cofactors FMN and FAD.
Industrial Synthesis
Many microorganisms are used in the large-scale synthesis of riboflavin, including bacteria Corynebacterium ammonia genes and Bacillus subtilis, as well as filamentous fungi including Ashbya gossypii, Candida famata, and Candida flaveri.
Commercial riboflavin for feed and food fortification is produced by B. subtilis which has been genetically engineered to produce more riboflavin and to incorporate a marker of antibiotic (ampicillin) resistance.
By 2012, these fermentation operations were producing more than 4,000 tons annually. Certain bacteria overproduce riboflavin in the presence of high amounts of aromatic chemicals or hydrocarbons, possibly as a defense mechanism.
Micrococcus luteus, strain ATCC 49442 (American Type Culture Collection), is one such organism. It grows on pyridine and becomes yellow when riboflavin is produced, but not on other substrates like succinic acid.
Laboratory Synthesis
Richard Kuhn’s group performed the first complete synthesis of riboflavin. In the last stage, a substituted aniline made by reductive amination with D-ribose was condensed with alloxan:
Uses
Treatment of Corneal Thinning
The most prevalent type of corneal ectasia, or progressive corneal thinning, is called keratoconus. Corneal collagen cross-linking, which stiffens the cornea, is used to treat the disorder. Applying a topical riboflavin solution to the cornea and exposing it to ultraviolet A light causes cross-linking.
Migraine Prevention
High-dose riboflavin (400 mg) is “probably effective and should be considered for migraine prevention,” according to the American Academy of Neurology’s 2012 guidelines. The UK National Migraine Centre likewise supports this advice.
According to a 2017 analysis, adults who take 400 mg of riboflavin daily for at least three months may experience fewer migraine headaches. Supplements are not advised because the evidence of high-dose riboflavin’s effectiveness in treating or preventing migraines in children and adolescents is conflicting.
Food Coloring
In Europe, riboflavin (yellow-orange crystalline powder) is referred to as food additive E101 and is used as a food coloring.
Dietary Recommendations
In 1998, the Recommended Dietary Allowances (RDAs) and Estimated Average Requirements (EARs) for riboflavin were revised by the National Academy of Medicine.
For both men and women over the age of 14, the EARs for riboflavin are 1.1 mg/day and 0.9 mg/day, respectively, whereas the RDAs are 1.3 and 1.1 mg/day.
To offer appropriate intake amounts for people with greater than normal requirements, RDAs are higher than EARs. The recommended daily allowance (RDA) for pregnant women is 1.4 mg, and the RDA for nursing women is 1.6 mg.
The Adequate Intake (AI) for infants under 12 months of age is 0.3–0.4 mg/day, and the recommended daily allowance (RDA) rises from 0.5 to 0.9 mg/day for kids ages 1 to 13 years.
When there is enough data to support a claim, the IOM establishes tolerable upper intake levels (ULs) for vitamins and minerals.
Since there are no human studies on the negative consequences of large dosages of riboflavin, there is no upper limit for this nutrient. Dietary Reference Intakes (DRIs) is the term used to refer to the EARs, RDAs, AIs, and ULs that have been taken together.
The combined collection of data is referred to as Dietary Reference Values by the European Food Safety Authority (EFSA), which uses Population Reference Intake (PRI) rather than RDA and Average Requirement (EAR) in place of EAR.
The definitions of AI and UL are the same as in the US. The PRI is set at 1.6 mg/day for men and women who are 15 years of age and older.
The recommended daily intake (PRI) for pregnant women is 1.9 mg, while for nursing women, it is 2.0 mg. The PRIs rise with age in children (1–14 years old), going from 0.6 to 1.4 mg/day.
The PRIs are more than the RDAs in the US. Like the American National Academy of Medicine, the European Food Safety Agency (EFSA) likewise examined the maximum safe intake and determined that insufficient data existed to establish a UL.
Safety
Riboflavin toxicity caused by high doses has not been observed in humans, and as dosage increases, absorption efficiency decreases.
Any extra riboflavin is eliminated from the body through the kidneys, which causes flavinuria—a vivid yellow tint in the urine.
Subjects in a clinical experiment receiving up to 400 mg of riboflavin orally daily for three to twelve months were treated with the vitamin in an attempt to reduce the incidence and intensity of migraines. Aside from diarrhea, other adverse effects were recorded as well.
Labeling
To comply with U.S. regulations for food and dietary supplement labeling, the quantity in a serving is stated as a percentage of Daily Value (%DV). 100% of the Daily Value for riboflavin labeling was 1.7 mg; however, starting on May 27, 2016, it was changed to 1.3 mg to conform to the RDA. Reference Daily Intake provides a table with the current and old adult daily values.
Sources
One can look for the riboflavin content of hundreds of foods in the food composition database kept by the Agricultural Research Service of the United States Department of Agriculture.
Since 85% of riboflavin is lost during the milling of wheat, some nations enhance their white flour. Additionally, riboflavin is added to infant food, vitamin-enriched meal replacements, pasta, and morning cereals.
Since riboflavin is poorly soluble in water, it is difficult to mix into liquid products. For this reason, riboflavin-5′-phosphate (FMN), a more soluble version of riboflavin, is required when employed as a colorant.
It is also known as E101. A large portion of the vitamin’s dietary intake comes from bread and ready-to-eat morning cereal fortification.
| Source | Amount (mg) (per 100 grams) |
| Beef liver, pan-fried | 3.42 |
| Chicken liver, pan-fried | 2.31 |
| Whey protein powder | 2.02 |
| Salmon, cooked, wild/farmed | 0.49/0.14 |
| Cows’ milk, whole | 0.41 (one cup) |
| Turkey, cooked, dark/breast | 0.38/0.21 |
| Pork, cooked, chop | 0.23 |
| Chicken eggs, fried | 0.23 (one, large) |
| Chicken, cooked, thigh/breast | 0.19/0.11 |
| Beef, ground, cooked | 0.18 |
| Source | Amount (mg) (per 100 grams) |
| Cheese, cheddar | 0.43 |
| Yogurt, whole milk | 0.25 (one cup) |
| Almonds | 1.14 |
| Mushrooms, white, raw | 0.40 |
| Spinach, boiled | 0.24 |
| Bread, baked, fortified | 0.25 |
| Pasta, cooked, fortified | 0.14 |
| Corn grits | 0.06 |
| Rice, cooked, brown/white | 0.05/0.00 |
| Source | Amount (mg) (per 100 grams) |
| Avocado | 0.14 |
| Kale, boiled | 0.14 |
| Sweet potato baked | 0.11 |
| Peanuts, roasted | 0.11 |
| Tofu, firm | 0.10 |
| Beans, green | 0.10 |
| Brussels sprouts, boiled | 0.08 |
| Romaine lettuce | 0.07 |
| Potato, baked, with skin | 0.05 |
| Beans, baked | 0.04 |
| Age group (years) | RDA for riboflavin (mg/d) |
| 0–6 months | 0.3* |
| 6–12 months | 0.4* |
| 1–3 | 0.5 |
| 4–8 | 0.6 |
| 9–13 | 0.9 |
| Females 14–18 | 1.0 |
| Males 14–18 | 1.3 |
| Females 19+ | 1.1 |
| Males 19+ | 1.3 |
| Pregnant females | 1.4 |
| Lactating females | 1.6 |
| Age group (years) | PRI for riboflavin (mg/d) |
| 7–11 months | 0.4 |
| 1–3 | 0.6 |
| 4–6 | 0.7 |
| 7–10 | 1.0 |
| 11–14 | 1.4 |
| 15–adult | 1.6 |
| Pregnant females | 1.9 |
| Lactating females | 2.0 |
Foods derived from animals naturally contain both FAD and FMN that are attached to proteins, as well as free riboflavin. Free riboflavin makes up the majority of the content in cow’s milk, however, FAD and FMN are also present in trace amounts.
Fortification
Grain-based food fortification is mandated or suggested in certain nations. As of 2021, food fortification of wheat flour or maize (corn) flour with riboflavin or riboflavin-5′-phosphate sodium is required in 56 nations.
Primarily in North and South America as well as Southeast Africa. The specified doses are between 1.3 and 5.75 mg/kg. There are volunteer fortification programs in 16 more nations. For instance, the Indian government suggests 4.0 mg/kg of “atta” (whole wheat) and “maida” (white) flour.
Absorption, Metabolism, Excretion
Protein-bound FMN and FAD make up over 90% of the riboflavin found in food. The coenzymes are released by exposure to gastric acid in the stomach and are then enzymatically degraded in the proximal small intestine to liberate free riboflavin.
A quick active transport mechanism is used for absorption, and at high concentrations, some extra passive diffusion takes place.
When the vitamin is taken with a meal, absorption is enhanced because bile salts help in uptake. The most riboflavin that an adult can absorb in a single dose is 27 mg, according to a tiny clinical investigation.
The liver absorbs most of the newly ingested riboflavin on the first pass. suggesting that riboflavin’s postprandial presence in blood plasma may be an underestimate of its absorption.
There are three known riboflavin transporter proteins: RFVT1 is found in the placenta and small intestine; RFVT2 is substantially expressed in the brain and salivary glands; and RFVT3 is primarily expressed in the prostate, testicles, and small intestine.
Riboflavin can be given orally to infants whose genes encoding these transport proteins have mutations. Reversibly, riboflavin is transformed into FMN and subsequently FAD. Zinc-requiring riboflavin kinase performs the conversion from riboflavin to FMN; phosphatase does the opposite.
The role of magnesium-dependent FAD synthase is to convert FMN to FAD; pyrophosphatase does the opposite.
It seems that FAD is an inhibitory end-product that inhibits the synthesis of itself. Urine swiftly removes excess riboflavin from the bloodstream once it is absorbed by the small intestine.
Under normal circumstances, urine color correlates with urine specific gravity and urine osmolality, serving as an indicator of hydration status.
Urine turns yellower than usual when riboflavin is supplemented in great excess of requirements, though.
About two-thirds of the urine produced with a normal dietary intake is made up of riboflavin; the remaining portion is partially converted to hydroxymethylriboflavin by cellular oxidation and other metabolites.
When riboflavin is consumed in excess of its absorption capacity, it enters the large intestine where it is catabolized by bacteria into a variety of metabolites that are excreted.
Unabsorbed riboflavin has been suggested to have an impact on the microbiome of the large intestine.
Deficiency
Prevalence
In the US and other nations with fortification programs for wheat flour or corn meal, riboflavin deficiency is rare.
According to information gathered from biannual polls of Americans over the age of 20, 22% of women and 19% of men said they have taken a riboflavin-containing supplement, usually a multivitamin-mineral combination.
The average daily food consumption for adult women and men who did not use supplements was 1.74 mg and 2.44 mg, respectively.
The RDAs for riboflavin, which are 1.1 and 1.3 mg/day, respectively, are exceeded by these levels.
Average food consumption for all age groups was higher than the recommended daily allowances. Less than 3% of Americans, according to a 2001–2002 survey, ingested less riboflavin than their estimated average requirement.
Signs and Symptoms
Stomatitis, also known as riboflavin deficiency or ariboflavinosis, is characterized by symptoms such as chapped and fissured lips, sore throat, painful red tongue, and inflammation of the mouth’s corners.
Itching, watering, bloodshot, and light sensitivity can occur in the eyes. Anemia and riboflavin deficiency are related.
Long-term riboflavin deficiency can lead to liver and nervous system damage. Pregnant women may be more susceptible to preeclampsia if they are deficient in riboflavin. Pregnancy-related riboflavin deficiency can cause heart and limb abnormalities in the fetus.
Risk Factors
Athletes who follow a vegetarian diet, vegans, and alcoholics are among the groups of people who are susceptible to low riboflavin levels.
If a mother abstains from meat and dairy products, she puts her unborn child and herself at risk. The risk of riboflavin insufficiency is increased in cases of anorexia and lactose intolerance.
Individuals who lead physically demanding lifestyles, such as laborers and athletes, might need to consume more riboflavin. Individuals suffering from riboflavin transporter impairment, adrenal insufficiency, and hypothyroidism have reduced riboflavin conversion into FAD and FMN.
Causes
Usually, riboflavin shortage coexists with other nutritional deficits, especially those of other water-soluble vitamins.
There are two types of riboflavin deficiencies: primary, which are brought on by inadequate vitamin sources in the food, and secondary, which can be brought on by illnesses that interfere with the intestines’ ability to absorb vitamins.
The body’s inability to utilize the vitamin or its increased rate of excretion are the usual causes of secondary deficiencies.
Dietary practices such as low-dairy vegetarianism and veganism raise the risk of deficiency. Riboflavin deficiency can be brought on by or made worse by illnesses like diabetes, cancer, and heart disease.
Rare genetic flaws can impair the transport, metabolism, absorption, or utilization of riboflavin via flavoproteins.
Riboflavin transporter deficit, formerly called Brown–Vialetto–Van Laere disease, is one of these. Defective versions can be found in the genes SLC52A2 and SLC52A3, which encode the transporter proteins RDVT2 and RDVT3, respectively.
Young children and infants can exhibit respiratory distress brought on by a sensorimotor axonal injury, feeding difficulties, sensory symptoms such as sensory ataxia, muscle weakness, and cranial nerve abnormalities including hearing loss.
both cranial nerve pathology and neuropathy. Babies with riboflavin transporter deficiency have difficulty breathing and a ten-year mortality rate if left untreated.
Treatment with high-dose oral riboflavin supplements can save lives. Additional inborn errors of metabolism include the C677T variant of methylenetetrahydrofolate reductase.
Which has been linked to an increased risk of high blood pressure in adults, and riboflavin-responsive multiple acyl-CoA dehydrogenase deficiency, which is also referred to as a subset of glutaric acidemia type 2.
Diagnosis and Assessment
Whenever a deficiency is detected, the evaluation of riboflavin status is crucial for validating patients with non-specific symptoms.
In healthy adults with a normal riboflavin intake, the total amount of riboflavin excreted is approximately 120 micrograms per day; excretion of less than 40 micrograms per day is indicative of a deficiency.
Excretion rates of riboflavin decline with age but rise while under prolonged stress or when taking certain prescription medications.
Erythrocyte glutathione reductase (EGR), erythrocyte flavin concentration, and urine excretion are indicators used in humans.
A measure of tissue saturation and long-term riboflavin status is provided by the erythrocyte glutathione reductase activity coefficient (EGRAC).
Enzyme activity measured both with and without the addition of FAD to the culture medium is used to calculate the activity coefficient ratio, which is used to express the results.
An EGRAC of 1.0 to 1.2 means that riboflavin levels are appropriate; 1.2 to 1.4 is regarded as low, and more than 1.4 means that riboflavin levels are deficient.
Regarding the less perceptive “erythrocyte flavin method,” levels below 270 nmol/L are deemed insufficient while values above 400 nmol/L are deemed appropriate.
The amount of riboflavin excreted in the urine is reported as nmol per gram of creatinine. The range of 50 to 72 nmol/g is considered low.
The deficit is less than 50 nmol/g. Dietary needs have been established through the use of urinary excretion load testing. Urinary riboflavin levels in adult men increased somewhat as oral dosages were raised from 0.5 mg to 1.1 mg.
Reaching 100 micrograms during a second 24-hour urine collection. Urine excretion significantly rose after a load dosage of 1.1 mg, reaching 800 micrograms of urine output during a 24-hour urine sample at a dose of 2.5 mg.
History
The term “riboflavin” is derived from the terms “ribose,” which is the sugar whose reduced form, ribitol, is part of its structure, and “flavin,” which is the ring moiety that gives the oxidized molecule its yellow color (from the Latin flavus, “yellow”).
Together with the oxidized form, the reduced form is produced during metabolism and manifests as orange-yellow needles or crystals.
It was Alexander Wynter Blyth who made the first known identification, predating the idea that vitamins are necessary nutrients.
When exposed to light, a water-soluble substance found in cow’s milk whey that Blyth dubbed “lactochrome” fluoresced yellow-green.
This discovery was made in 1879. Several research labs were looking at feeding ingredients that were necessary to keep rats growing in the early 1900s.
Originally, these components were separated into two categories: water-soluble “vitamin” B and fat-soluble “vitamin” A. (The 1920 version omitted the “e”).
It was also believed that vitamin B consisted of two parts: B1 (a heat-labile chemical) and B2 (a heat-stable material).
It was speculatively determined that vitamin B2 was required. for avoiding pellagra; however, it was subsequently determined that the cause was a deficit in niacin (vitamin B3).
The mistake resulted from the fact that stomatitis symptoms caused by riboflavin (B2) deficiency are similar to those of pellagra, although they do not involve broad lesions on the peripheral skin.
Consequently, when riboflavin deficiency in humans was first identified, the illness was occasionally referred to as “pellagra sine pellagra” (pellagra without pellagra).
Paul Gyorgy, working with chemist Richard Kuhn and physician T. Wagner-Jauregg, discovered in 1935 that rats fed a diet devoid of B2 were incapable of gaining weight.
When rats were fed the brilliant yellow-green fluorescent substance that was isolated from yeast, their growth returned to normal.
The intensity of the fluorescence directly correlated with the growth that was recovered. Because of this insight, the researchers were able to quickly chemical bioassay in 1933, and after that, separate the component out of egg white and refer to it as ovoflavin.
Later, the same team separated a related substance from whey and gave it the name lactoflavin. When Kuhn’s team discovered in 1934 that these flavins had the same chemical structure, they decided to call it “riboflavin” and succeeded in synthesizing the vitamin.
Riboflavin was also known as “Vitamin G” until about 1937. Richard Kuhn won the 1938 Nobel Prize in Chemistry as a result of his research on vitamins, which included B2 and B6.
A 1939 clinical trial led by William H. Sebrell and Roy E. Butler showed that riboflavin is necessary for human health.
When given synthetic riboflavin, women who were fed a diet deficient in riboflavin recovered from stomatitis and other symptoms of insufficiency. When the supplements were stopped, the symptoms came back.
FAQ
What is the deficiency of vitamin B2?
Depression, weariness, swelling throats, and hazy vision can all be symptoms of riboflavin insufficiency. It can lead to dermatitis, skin cracks, and itching in the area around the mouth. In addition to reproductive problems, there may be liver deterioration, hair loss, hyperemia, and edema around the throat.
Which fruit contains vitamin B2?
Fruits: Pears, apples, berries, bananas, figs, and pears are all decent providers of vitamin B2.
What does vitamin B2 do for the skin?
Vitamin B2, also known as riboflavin, is an excellent supplement for dry or acne-prone skin because it can balance natural oils, brighten skin tone, and enhance skin tone. Nicotinic acid, also known as niacinamide, or vitamin B3, is a nutrient that helps your skin’s protection mechanisms.
What produces vitamin B2?
All plants and the majority of microorganisms produce riboflavin, also known as vitamin B2, a water-soluble vitamin that is vital to the growth and reproduction of both humans and animals.
Why is vitamin B2 necessary?
Vitamin B2, or riboflavin, is necessary for the proper growth, development, and operation of your body’s cells. It also facilitates the conversion of meals into the energy your body needs.
Is milk rich in vitamin B2?
A cup of milk, or 240 milliliters (mL), contains 26% of the daily value (DV) for riboflavin. It also contains lower amounts of other B vitamins, such as ( 18 ): The DV for thiamine (B1) is 9%. B2 riboflavin: 32% of the Daily Value. The daily value of pantothenic acid (B5) is 18%.






One Comment