Common Peroneal Nerve Injury: Physiotherapy Treatment
What is a Common Peroneal Nerve Palsy?
- The common peroneal nerve (common fibular nerve, external popliteal nerve, lateral popliteal nerve) is a nerve in the lower leg that provides sensation and motor function to parts of the lower leg. When damaged or compressed, it can cause foot drop.
- The common peroneal nerve, about one-half the size of the tibial nerve, arises from the dorsal branches of the fourth and fifth lumbar and the first and second sacral nerves.
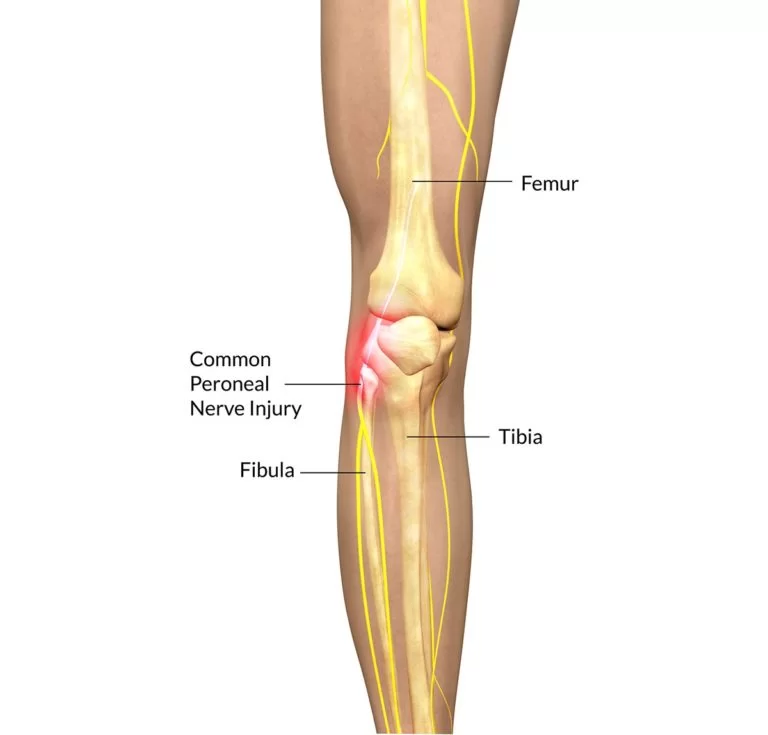
- It descends obliquely along the lateral side of the popliteal fossa to the head of the fibula, close to the medial margin of the biceps femoris muscle. Where the common peroneal nerve winds round the head of the fibula, it is palpable.
- It lies between the tendon of the biceps femoris and lateral head of the gastrocnemius muscle, winds around the neck of the fibula, between the peroneus longus and the bone, and divides beneath the muscle into the superficial peroneal nerve and deep peroneal nerve.
- A peroneal nerve injury (also called foot drop), is a peripheral nerve injury that affects a patient’s ability to lift the foot at the ankle. While foot drop injury is a neuromuscular disorder, it can also be a symptom of a more serious injury, such as a nerve compression or herniated disc.
Anatomy of Common Peroneal Nerve
BRANCHES OF COMMON PERONEAL NERVE
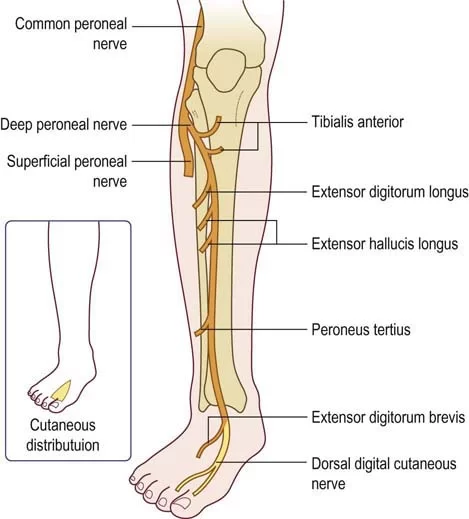
- The common peroneal nerve branches from the sciatica nerve. It includes the deep and superficial peroneal branches.
- (1) Articular branches:
- Two of these accompany the superior and inferior lateral genicular arteries to the knee, the upper one occasionally arises from the trunk of the sciatic nerve.
- The third articular nerve is given off at the point of division of the common peroneal nerve, it ascends with the anterior recurrent tibial artery through the tibialis anterior to the front of the knee.
- (2) Lateral sural cutaneous nerve: It supplies the skin on the lateral and posterior surface of the leg.
- (3) Motor branches:
- As the common peroneal nerve exits the popliteal fossa, it courses around the lateral aspect of the leg just below the head of the fibula.
- Here it is apposed with fibula and gives off two branches, the superficial peroneal branch and deep peroneal branch.
- The superficial peroneal nerve supplies the muscles of the lateral compartment of the leg namely: peroneus longus and peroneus brevis. These two muscles assist with eversion and plantar flexion of the foot.
- The deep peroneal nerve innervates the muscles of the anterior compartment of the leg which are: tibialis anterior, extensor hallucis longus, extensor digitorum longus, and the peroneus tertius. Together these muscles are responsible for dorsiflexion of the foot and extension of the toes.
- The deep peroneal nerve also innervates intrinsic muscles of the foot including the extensor digitorum brevis and the extensor hallucis brevis.
FUNCTIONS OF COMMON PERONEAL NERVE
- The common peroneal nerve innervates the short head of the biceps femoris muscle via a motor branch that exits close to the gluteal cleft. The remainder of the peroneal-innervated muscles are innervated by its branches, the deep peroneal nerve, and the superficial peroneal nerve.
- It provides sensory innervation to the skin over the upper third of the lateral aspect of the leg via the lateral cutaneous nerve of the calf. It gives the peroneal communicating nerve which joins the sural nerve in the midcalf.
Clinical Significance of Common Peroneal Nerve Palsy
- Chronic peroneal neuropathy can result from, among other conditions, bed rest of long duration, hyperflexion of the knee, peripheral neuropathy, pressure in obstetric stirrups, and conditioning in ballet dancers.
- The most common cause is habitual leg crossing which compresses the common peroneal nerve as it crosses around the head of the fibula. Transient trauma to the nerve can result from a peroneal strike.
- Damage to this nerve typically results in foot drop, where dorsiflexion of the foot is compromised and the foot drags (the toe points) during walking, and in sensory loss to the dorsal surface of the foot and portions of the anterior, lower-lateral leg. A common yoga kneeling exercise, the Vajrasana, has been linked to a variant called yoga foot drop.
- Surgical procedures involving the nerve involve:
- Peroneal nerve decompression: To surgically decompress the peroneal nerve, an incision is made over the neck of the fibula. Fascia surrounding the nerves to the lateral side of the leg is released.
- Deep peroneal nerve decompression: In the surgical treatment of deep peroneal nerve entrapment in the foot, a ligament from the extensor digitorum brevis muscle that crosses over the deep peroneal nerve, putting pressure on it and causes pain, is released.
Causes of Common Peroneal Nerve Palsy
- Injury to the spinal cord.
- Other underlying disease such as,
- Amyotrophic lateral sclerosis(ALS).
- Multiple sclerosis (MS).
- Parkinson’s disease.
- Sometimes it is a complication of hip replacement surgery.
- Knee or joint dislocation or fracture.
- Herniated disc.
- Trauma or injury to the knee.
- Fracture of the fibula.
- Use of tight plaster cast (or the long-term constriction) of the lower leg.
- Crossing the leg regularly.
- Regularly wearing high shoes.
- Pressure to the knee from positions during deep sleep or coma.
Symptoms
- Inability to point toes toward the body (dorsi flexion).
- Pain.
- Weakness.
- Numbness (on the shin or top of the foot).
- Loss of function of foot.
- High-stepping walk (called steppage gait or footdrop gait).
- Decreased sensation or tingling in the top of the foot or the outer part of the upper or lower leg.
- Walking problems.
- Loss of muscle mass because the nerves aren’t stimulating the muscles.
Possible Complications
- Decreased ability t walk.
- Permanent decrease in sensation in the legs or feet.
- Permanent weakness or paralysis in the legs or feet.
- Side effects of medicines.
Diagnosis
- A comprehensive clinical exam, including neurological exams.
- Complete medical history.
- Electrical testing.
- Nerve conduction velocity(NCV) test.
- X-rays.
- High resolution 3-T MRI.
- Nerve ultrasound.
- Electromyography.
Prevention
- Warm up and stretch properly before activity.
- Maintain physical fitness.
- Wear properly fitted and padded protective equipments.
- Avoid crossing legs or putting long-term pressure on the back or side of the knee. Treat injuries to the leg or knee right away.
- If a cast, splint, dressing, or other pressure on the lower leg causes a tight feeling or numbness, call your provider.
Prognosis Common Peroneal Nerve Palsy
- Common peroneal nerve injury is often curable with non-surgical treatment. Often symptoms will go away on their own (spontaneously). Sometimes, surgery is needed to relieve pressure from the nerve.
Treatment of Common Peroneal Nerve Palsy
- Treatment first involves resting from any activities that cause the symptoms to get worse.
- The use of ice and medicine may reduce pain and inflammation.
- If ice is used, do not place it directly on the skin. Instead, place a towel in-between.
- If there is weakness of the muscles, causing foot drop, bracing the ankle and foot may be needed.
- It is important to perform strengthening and stretching exercises to maintain muscle strength.
- These exercises may be completed at home or with a physiotherapist.
- If pain continues to get worse, despite treatment, or a cyst is present, surgery may be needed to relieve the pressure on the nerve.
- If the pressure on the nerve is due to compartment syndrome, a fascial (sheet of connective tissue) release may need to be performed.
- The earlier surgery is performed, the better your chances of full recovery.
Medical Treatment
- If pain medicine is needed, non-steroidal anti-inflammatory medicines (aspirin and ibuprofen), or other minor pain relievers (acetaminophen), are often advised.
- Do not take pain medicine for 7 days before surgery.
Physiotherapy Treatment
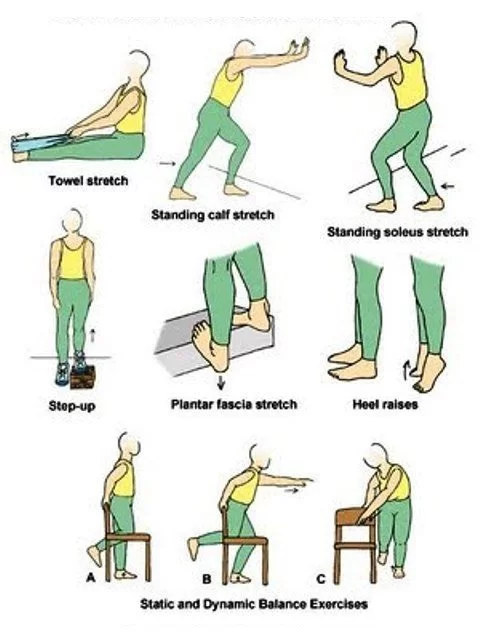
- The goals of physical therapy intervention include minimizing edema, increasing neural mobility, and maintaining or increasing the strength and endurance of unaffected sites.
- Range of motion exercise for ankle eversion.
- Range of motion exercises for ankle inversion.
- Range of motion exercise for ankle dorsiflexion, active assisted.
- Stretching of calf and hamstring muscle.
- Stretching of the gastrocnemius soleus muscle.
- Strengthening exercises for dorsiflexion, ankle eversion, and ankle inversion.
- Modalities:
- Cold therapy.
- Electric stimulation.
- Ultrasound.
- Iontophoresis.
- Ankle-foot orthosis.
Electrical Stimulation :
- Electrical Stimulation is categorized in two parts : Surge Faradic (SF) And Inter-mittant Galvanic(IG) Current.
- Reaction of Degeneration (RD Test) is required according to which IG or SF will be given.
- If RD Test is positive , IG is preferences And as recovery progress SF is given.
- Progress report is checked by SD Curve.
- Selection of Motor point is too much important in Electrical stimulation.
- IG Currunt Maintain Muscle property And Reduce Muscle Wasting
- SF Currunt strengthen Muscle from Helps to Grade 0 to 3 Grades SF is useful.
Related Other Nerve Injury Post :




Pesama iruda konjam…ivan vera !!
Hi- Great article? I am in PT for left side peroneal nerve issue. I pointed out with my finger feeling the nerve only on the left side, centered in the pain site. I have pain during and after tennis and pickleball, then afterward have pain walking. However, I can cycle all day. I have no motor and sensory loss. I hear cases of entrapment where patients experience motor and sensory issues– Do I have entrapment, or something else? Thanks very much!
sorry, that was supposed to be an exclamation point!!!
I am dealing with a left knee trapped perineal nerve entrapment. I can tell you first hand Physical therapy does NOT work. I have also had a left ulnar nerve entrapment where surgery was the only option. I love your information on this site. I would add as an another cause, is standing to long periods of time. I had none of the above causes to my condition. My left knee popped one day walking and in retail as I stand for 7 hours a day it just happened out of nowhere. Thank you for this great site! Just wanted to let you know that I would add to other causes of this condition, long periods of standing. I was even on a stress mat and it didn’t help. I am now in a walking boot awaiting surgery.