Ataxia
Ataxia is a neurological sign characterized by a lack of coordination during voluntary movements. It can affect various body parts, including limbs, hands, fingers, speech, and eye movements.
A person with ataxia experiences difficulties coordinating the movement of their muscles, resulting in sloppy, awkward, or unwieldy movements. This could be a sign of many different ailments or situations, or it could occur on its own. Treatment or reversal of ataxia’s consequences is occasionally achievable, depending on the cause.
A loss of coordination is referred to as ataxia, and it causes irregular, awkward, or even clumsy movements. Usually, it indicates an issue with your hearing, brain, or other nervous system components.
Introduction
“ataxia” refers to a class of neurological illnesses caused by a failure in the nervous system’s movement-controlling components that impair speech, balance, and coordination. Different physical actions, such as walking, reaching, and gripping objects, might be impacted by ataxia. The cerebellum, the area of the brain in charge of coordinating movement, or the nerves that link the cerebellum to the muscles are usually damaged.
A lack of control over muscles leading to awkward motions is called ataxia. It may impact eye movements, speech and swallowing, hand coordination, walking, and balance.
Most often, ataxia is caused by injury to the cerebellum or its connections in the brain. The cerebellum regulates the coordination of muscles.
Atherosclerosis can arise from several conditions, including alcoholism, degenerative diseases, strokes, tumors, multiple sclerosis, and hereditary problems. Some medications can also bring on Ataxia.
Ataxia treatment is based on the underlying reason. To help sustain independence are devices like canes and walkers. Another name for these is adaptable devices. Occupational treatment, speech therapy, physical therapy, and consistent exercise may also be beneficial.
What is ataxia?
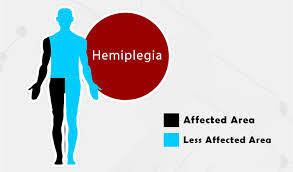
Ataxia is the absence of coordination. Atherosclerosis causes a loss of motor control in the arms and legs. This could result in poor balance, poor coordination, and difficulty walking. The fingers, hands, arms, legs, body, voice, and even eye movements can all be impacted by ataxia.
Ataxia is a symptom that can result from a variety of causes, such as:
- Stroke.
- Multiple sclerosis.
- Tumors.
- Alcoholism.
- Nerve damage.
- Metabolic disorders.
- Vitamin deficiencies.
In certain situations, ataxia may improve with treatment for the underlying cause.
Although ataxia is most commonly used to describe symptoms, it can also refer to a class of distinct central nervous system degenerative illnesses known as hereditary and sporadic ataxias:
- Hereditary ataxias: This kind is brought about by an inherited genetic flaw. Degenerative illnesses such as hereditary ataxias can advance over several years. The type of ataxia, the age at which symptoms first appear, and other variables determine how severe the condition is. Some inherited ataxias begin in childhood, while others manifest in adulthood.
- Sporadic ataxias: This type has no documented family history and typically manifests in maturity.
What are the three main types of ataxia?
There are three primary forms of ataxia, each with its mechanism of occurrence.
Cerebellar
The cerebellum, a brain region that controls how other brain areas interact, is malfunctioning in this kind of ataxia.
When ataxia results from cerebellar dysfunction, it is referred to as cerebellar ataxia. The cerebellum is in charge of combining a large amount of brain data that is required for motor planning and the seamless coordination of ongoing actions. Many disorders affecting the cerebellum can cause ataxia, even though it is not a symptom of all cerebellar lesions. It can be difficult for people with cerebellar ataxia to control the rhythm, force, range, direction, and velocity of their muscle contractions.
Asthenia, asynergy, dyschronometria, delayed reaction time, and other conditions can all be symptoms of this distinctive kind of erratic, uncoordinated movement. In addition to gait instability, eye movement difficulties, dysarthria, dysphagia, hypotonia, dysmetria, and dysdiadochokinesia, individuals with cerebellar ataxia may also exhibit these symptoms. Which cerebellar structures are affected and whether the lesion is unilateral or bilateral can affect these impairments.
An inability to walk in tandem or stand on one leg may be the first sign of impaired balance in people with cerebellar ataxia. As the disease worsens, walking becomes more erratic, with a wider base, high stepping, and lurching from side to side. Additionally difficult and perhaps dangerous is turning. As the severity of cerebellar ataxia increases, standing and walking become quite difficult. Dysarthria is an articulation problem that can also be present and is typified by “scanning” speech, which has a slower tempo, erratic rhythm, and fluctuating volume. Moreover, ataxic breathing, voice trembling, and speech slurring could manifest.
Movement incoordination, especially in the extremities, maybe the outcome of cerebellar ataxia. Dysmetria is obvious because finger-to-nose and heel-to-shin testing result in overshooting, or hypermetria. Dysdiadochokinesia, alternating movement impairments, and dysrhythmia are possible manifestations. People who have cerebellar ataxia may have titubation or tremors of the head and trunk.
A deficiency in the regulation of interaction torques in multijoint motion is considered to be the cause of dysmetria. When the primary joint is moved, interaction torques are produced at an associated joint. For instance, flexion at the shoulder would produce a torque at the elbow, and extension of the elbow would produce a torque at the wrist if the movement involved reaching to contact a target in front of the body. To generate coordinated movement, these torques must be compensated for and corrected as the speed of movement rises. Therefore, at higher movement velocities and accelerations, this could account for poorer coordination.
A vestibulocerebellar (flocculonodular lobe) dysfunction affects balance and eye movement coordination. To gain a larger base and prevent titubation (a physiological oscillation that tends to be forward-backward), this expresses itself as postural instability, in which the person tends to spread his or her feet upon standing. Therefore, whether or not the eyes are open, standing with the feet together exacerbates the instability. Given that the subject feels unsteady even when their eyes are open, this is a negative Romberg test, or more precisely, it indicates that the subject is incapable of performing the test.
A broad “drunken sailor” gait, known as truncal ataxia, is a symptom of spinocerebellar dysfunction (vermis and surrounding areas along the midline). It is characterized by erratic starts and pauses, lateral deviations, and uneven steps. Falling is a worry for patients with ataxia due to this lack of gait. According to studies looking at falls in this demographic, between 74 and 93% of patients report having fallen at least once in the previous year, and up to 60% of them say they are afraid to fall.
“Dysfunction of the cerebrocerebellum” (lateral hemispheres) manifests as abnormalities in the extremities’ ability to move voluntarily and according to plan (appendicular ataxia). Among these are:
- Coarse trembling that is emphasized during the performance of voluntary motions, potentially affecting the head, eyes, limbs, and torso, is known as intention tremor.
- Unusual writing styles (big, uneven letters, erratic underlining).
- A particular type of dysarthria (slurred speech, occasionally accompanied by abrupt changes in voice volume despite regular rhythm).
- Dysdiadochokinesia, or the inability to produce fast alternating movements, can cause rapid forearm pronation and supination. As speed increases, movements become increasingly erratic.
- It is possible to misjudge distances or movement ranges. When dysmetria occurs, the necessary distance or range to reach a goal is frequently regarded as either undershooting, hypometria, overshooting, or hypermetria. When a patient is requested to touch someone’s finger or nose, this can occasionally be observed.
- When individuals with cerebellar ataxia flex their elbows isometrically against resistance, for instance, they may exhibit the rebound phenomenon, often referred to as the loss of the check reflex. The patients’ arms may swing up and possibly hurt themselves if the resistance is abruptly removed without warning. Patients who still have an intact check reflex check and contract their opposing triceps to halt and slow down their movement.
- Patients may present with a range of cognitive symptoms, from subtle to overt, together referred to as Schmahmann’s syndrome.
Sensory
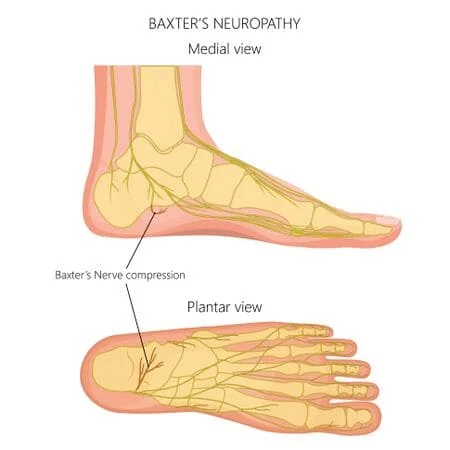
Your body has an innate ability to “self-position,” which allows your brain to keep track of the location of each bodily part. This can be demonstrated by the way you can locate your hands and feet even when you are blind (e.g., in a dark environment or with your eyes closed). Self-positioning sense is disrupted by sensory ataxia.
When ataxia results from a loss of proprioception—that is, from being less sensitive to the locations of body parts and joints—it is referred to as sensory ataxia. Given that the dorsal columns of the spinal cord transmit proprioceptive information to the brain, malfunction in these columns is typically the source of this. In certain instances, the reason behind sensory ataxia could potentially be due to malfunctions in the different brain regions that process positional data, such as the thalamus, parietal lobes, and cerebellum.
In addition to a postural instability that is typically exacerbated when proprioceptive input is lacking and cannot be replaced by visual input, as in dimly illuminated surroundings, sensory ataxia manifests as an unstable “stomping” walk with heavy heel strikes.
During a physical examination, doctors can look for signs of sensory ataxia by having patients stand with their feet together and their eyes closed. This results in a significant worsening of instability in affected people, causing large oscillations and maybe a fall; this is referred to as a positive Romberg test. The addition of difficulty in the finger-pointing test when the eyes are closed is a characteristic of sensory ataxia. Moreover, when patients stand with their hands and arms extended toward the doctor and their eyes closed, their fingers tend to “fall” before abruptly contracting to return to the extended horizontal posture (known as the “ataxic hand”).
Vestibular
This kind entails an issue with your inner ears, which play a role in your equilibrium. Your coordination is affected, making it difficult to maintain your feeling of balance.
When the vestibular system malfunctions, ataxia results. In acute and unilateral cases, strong vertigo, nausea, and vomiting are linked with vestibular ataxia. These distinctive signs and symptoms might not be evident in slow-onset, chronic bilateral cases of vestibular dysfunction, leaving dysequilibrium as the only symptom.
What causes ataxia?
Ataxia results from the degeneration of nerve cells due to aberrant protein production caused by a faulty gene. Muscles lose their ability to respond to brain commands as the disease worsens. Balance and coordination deteriorate as a result.
The brain region known as the cerebellum or its connections can sustain damage that results in ataxia. The brainstem is connected to the cerebellum, which is situated near the base of the brain. Speech, swallowing, eye movements, and balance are all regulated in part by the cerebellum.
The three main categories of causes of ataxia are acquired, degenerative, and inherited.
Acquired causes
- Alcohol: Persistent ataxia may result from long-term excessive alcohol consumption. If alcohol is avoided entirely, ataxia may become better.
- Medicines: One possible adverse effect of some medications is ataxia. Sedatives like benzodiazepines and phenobarbital may be to blame.Moreover, anti-seizure medications, particularly phenytoin, may be to blame. Ataxia is another side effect of several chemotherapy treatments.
- Toxins: Ataxia can also result from solvent intoxication, such as paint thinner, or heavy metal toxicity, such as lead or mercury.
- Too little or too much of certain vitamins: Lack of vitamin E, vitamin B-12, or vitamin B-1, sometimes referred to as thiamine, may be the cause of ataxia. Ataxia can also result from excess or insufficient vitamin B-6. A vitamin deficit is the absence of sufficient amounts of a certain vitamin. Ataxia can frequently be cured when it is caused by a vitamin shortage.
- Thyroid conditions: Atherosclerosis may result from hypothyroidism or hypoparathyroidism.
- Stroke: A stroke can cause abrupt ataxia onset. A blood artery blockage or brain hemorrhage could be the cause of this.
- Multiple sclerosis: Ataxia could result from this illness.
- Autoimmune diseases: Ataxia can be brought on by several autoimmune illnesses, which are conditions where the body assaults healthy cells. Sarcoidosis is one of them; it is a condition that results in the accumulation of inflammatory cells in certain body areas. Alternatively, they can consist of celiac disease, an ailment brought on by an immunological response to gluten consumption. Ataxia may also be brought on by specific forms of encephalomyelitis, a disorder that causes swelling in the brain and spinal cord.
- Infections: Ataxia can infrequently be a sign of viral illnesses including HIV and Lyme disease as well as pediatric chickenpox. It may manifest throughout the infection’s healing phase and linger for several days or weeks. Usually, the symptom improves with time.
- COVID-19: A dangerous infection with the COVID-19 virus can produce ataxia.
- Paraneoplastic syndromes: These are uncommon degenerative illnesses brought on by the immune system’s reaction to a neoplasm, or malignant tumor. The most common causes of paraneoplastic syndromes include lymphoma, lung, ovarian, or breast cancer. Months or even years before the cancer is identified, ataxia may manifest.
- Changes in the brain: Ataxia may result from an abscess, an infected part of the brain. Furthermore, brain growth—whether malignant or not—can harm the cerebellum.
- Head trauma: Atherosclerosis can lead to ataxia.
- Cerebral palsy: This is a catch-all word for a range of disorders brought on by brain injury in children. The harm could occur before, during, or soon after birth. The child’s capacity to coordinate their body motions is impacted.
Degenerative causes
Multiple system atrophy: This uncommon illness has an impact on blood pressure and other bodily systems. Along with additional symptoms like inability to control one’s bladder, fainting after standing up, and a sleep behavior condition when a person plays out dreams, it can produce ataxia.
Hereditary causes
Certain forms of ataxia and certain diseases leading to ataxia are inherited. Another term for these disorders is inherited. It’s possible that you were born with a genetic alteration that results in abnormal protein synthesis if you have any of these illnesses.
Nerve cells, especially those in the cerebellum and spinal cord, are affected by the aberrant proteins. They lead to degeneration, or the disintegration and death of nerve cells. Coordination issues do not get better as the disease advances.
An autosomal dominant inheritance pattern refers to the possibility that an individual with genetic ataxia inherited a dominant gene from one parent. An autosomal recessive inheritance pattern is the possibility that they received a recessive gene from both parents. Recessive conditions do not impact the parents, although they may affect siblings.
There are various forms of ataxia caused by distinct gene mutations. The majority deteriorate with time. In addition to having certain symptoms, each kind also results in impaired coordination.
Autosomal dominant ataxias
- Spinocerebellar ataxias: The number of spinocerebellar ataxia genes that have been found is continually increasing, with over 40 being known. There may be additional symptoms in addition to the common ones of cerebellar degeneration and ataxia.
- Episodic ataxia (EA): Eight distinct forms of episodic ataxia are recognized. There are two most prevalent types: EA1 and EA2. Short episodes of ataxia, lasting a few seconds or minutes, are observed in EA1. The episodes are brought on by stress, abrupt motion, or being startled. They are frequently connected to twitching muscles.
- Longer ataxia episodes—typically lasting between 30 and 6 hours—are a feature of EA2. Stress is another factor that causes these episodes. There could be muscle weakness and dizziness.EA2 patients may experience extreme fatigue. Occasionally, symptoms go away as people age. The duration of episodic ataxia is not shortened, and medication may help with symptoms.
Autosomal recessive ataxias
Friedreich ataxia: The most prevalent type of ataxia that runs in families is this one. It involves injury to the peripheral nerves, spinal cord, and cerebellum. Signals from the arms and legs are sent to the brain and spinal cord via peripheral nerves. Usually, symptoms start well before the age of 25. For this kind of ataxia, a cerebellar scan often reveals no abnormalities.
Walking difficulties are generally the initial sign of Friedreich ataxia. Usually, the disease progresses to involve the trunk and arms. Foot abnormalities like high arches may result from this kind of ataxia. Additionally, it may result in scoliosis, a curvature of the spine.
Slurred speech, exhaustion, erratic eye movements, and hearing loss are further symptoms that could appear. Another possible outcome of Friedreich ataxia is cardiomyopathy or an enlarged heart. Diabetes and heart failure are also possible. Heart problems can be treated early to increase survival and quality of life.
RFC1-associated ataxia: The most frequent cause of ataxia that develops later in life is this. Nerve numbness or tingling in the body is a common sign of ataxia. This kind of ataxia might occasionally result in a cough.
Ataxia-telangiectasia: The brain and immune system deteriorate as a result of this uncommon pediatric illness. This elevates the likelihood of several ailments, such as infections and malignancies.
Little red “spider” veins that resemble spiders may develop in a child’s cheeks, ears, or around their eyes. This condition is known as telangiectasia. The initial signs and symptoms include frequently slurred speech, poor balance, and delayed development of motor skills. Sinus and respiratory infections occur often.
There is an increased risk of malignancy, especially leukemia or lymphoma, in children with ataxia-telangiectasia.
Congenital cerebellar ataxia: This kind of ataxia is caused by birth-related injury to the cerebellum.
Wilson’s disease: Copper accumulates in the liver, brain, and other organs of those who suffer from this illness. Along with other symptoms, this may result in ataxia.
What are the symptoms of ataxia?
Depending on the type of ataxia, symptoms and onset time can change. Usually, the most typical consist of:
- Balance and coordination problems (affected first).
- Poor coordination of hands, arms, and legs.
- Slurring of speech.
- Wide-based gait (manner of walking).
- Difficulty with writing and eating.
- Slow eye movements.
Atherosclerosis symptoms can mimic other illnesses or medical issues. For a diagnosis, always see your medical professional.
How is ataxia diagnosed?
Your healthcare provider searches for a curable cause while making an ataxia diagnosis. Exams for your nervous system and body will probably be performed. Your medical practitioner examines your reflexes, balance, vision, and coordination.
These tests could be performed in addition to a comprehensive neurological and physical examination, family history, and medical history:
- Blood tests: These could aid in identifying ataxia’s curable causes.
- Genetic testing: A genetic test may be suggested by your healthcare provider to determine whether a mutation in a gene is the cause of an ataxia-causing disorder. For many, but not all, hereditary ataxias, gene tests are available. Tests are carried out to find out if a person has specific chromosomal or gene alterations, or mutations, which are known to raise the risk for particular inherited diseases.
- A spinal tap, also known as a lumbar puncture: Test could be beneficial if ataxia is being caused by an infection, swelling (also known as inflammation), or specific disorders. A tiny sample of cerebrospinal fluid is taken using a needle placed between two bones in the lower back. The fluid, which envelops and shields the spinal cord and brain, is transported to a lab for analysis.
- Magnetic resonance imaging (MRI): A test that produces detailed images of the body’s organs and architecture using big magnets, radiofrequency energy, and a computer.
Additionally, these tests can be done to rule out other disorders that could be the cause of ataxia. Ataxia can occur suddenly in several circumstances, including head injuries, strokes, brain hemorrhages, infections, drug exposure, and heart or breathing problems.
Hypothyroidism, alcoholism, certain vitamin deficiencies, long-term medication exposure, multiple sclerosis, and other illnesses can all cause ataxia to develop gradually.
Risk factors
Athexia is associated with multiple risk factors. Individuals who have a family history of ataxia are more likely to develop the condition themselves.
Other risk factors involve:
- long-term excessive alcohol consumption.
- Having a hypoparathyroid or hypothyroid condition.
- Suffering from multiple sclerosis.
- Celiac disease, is an autoimmune disease brought on by consuming gluten.
- Sarcoidosis is a disease that causes inflammatory cells to accumulate in certain areas of the body.
- Having multiple system atrophy, a degenerative illness.
- Having a cancer-related paraneoplastic syndrome.
- Consuming drugs that raise the chance of ataxia, such as sedatives and anti-seizure medications.
- Having been in contact with solvents, like paint thinner, or heavy metals, such as lead or mercury.
lacking in thiamine, also known as vitamin E, vitamin B-6, vitamin B-12, or vitamin B-1. Overconsumption of vitamin B-6 is another risk factor.
What are the complications of ataxia?
The rate at which the various forms of ataxia progress varies depending on the particular syndrome. The worst-case scenario could involve choking, breathing difficulties, or irreversible rigidity, all of which could be fatal. Continuous positive airway pressure (CPAP), tracheostomy, or feeding tubes are necessary to treat some more challenging symptoms.
Aside from pressure sores, infections, and blood clots, falling or being bed- or chair-ridden might result in other potentially fatal consequences. Depression, behavioral issues, and dementia may have an impact on caregiving and compliance. Additional ataxia issues could be:
- Dizziness.
- Spasticity.
- Rigidity.
- Tremor.
- Pain.
- Fatigue.
- Low blood pressure with sitting or standing.
- Bowel or bladder dysfunction.
- Sexual dysfunction.
There are numerous ways to enhance the quality of life for an individual with ataxia.
How is ataxia treated?
An inherited ataxia cannot be cured. Furthermore, there is no medication to address the particular ataxia problem.
Treatment focuses on curing the underlying issues if ataxia results from a stroke, poor vitamin levels, or exposure to hazardous drugs or chemicals.
Using adaptive equipment to help the client retain as much independence as possible is the major treatment for imbalance or loss of coordination. A wheelchair, crutches, walkers, or canes are a few examples of these devices.
Treatments for symptoms like tremors, stiffness, depression, spasticity, and sleep difficulties may also include physical therapy, speech therapy, and medication.
The cause(s) of ataxias and strategies for treating, curing, and eventually preventing them are among the research topics being studied about cerebellar and spinocerebellar degeneration.
The reason determines how to treat ataxia. Treatment of the underlying problem may help alleviate symptoms if ataxia is brought on by a vitamin shortage or celiac disease. Should ataxia stem from chickenpox or other viral diseases, it is probable to resolve spontaneously.
The oral medication omaveloxolone (Skyclarys) is used to treat Friedreich ataxia. For adults and teens 16 years of age and older, the medication has been approved by the U.S. Food and Drug Association. In clinical trials, the medication improved symptoms when taken. Omaveloxolone can alter liver enzyme and cholesterol levels, so people taking this medication need to get regular blood tests. Omaveloxolone may cause headache, nausea, stomach pain, exhaustion, diarrhea, and soreness in the muscles and joints.
Other medications may help with symptoms like tremors, disorientation, and stiffness. Additionally, your healthcare provider may suggest adapted equipment or therapy.
Adaptive devices
Many sclerosis and cerebral palsy are two examples of diseases that may not be curable in ataxia patients. However assistive technology might be useful. They consist of:
- Walkers or hiking sticks for mobility.
- Redesigned eating utensils.
- Speaking instruments for communication.
Therapies
You could gain from some therapies, such as:
- Physical therapy to improve mobility and assist with coordination.
- Occupational therapy assists with activities of everyday life, such as feeding oneself.
- Speech therapy to facilitate swallowing and enhance speech.
Studies have indicated that certain individuals with ataxia may benefit from strength and aerobic training.
Can I treat ataxia myself?
People with ataxia frequently experience fatigue or stress-related symptoms. You just need some relaxation and recuperation in these situations. The same holds for alcohol-induced ataxia (except for cases in which hazardous dosages are consumed).
Ataxia, however, isn’t always a symptom you should disregard, try to self-diagnose or cure it on your own.
How can ataxia be prevented?
Ataxia can be caused by a few avoidable factors. However, since many of the reasons are unpredictable, it is impossible to stop or avoid them. Furthermore, it’s not always possible to lower the likelihood of experiencing this symptom.
The following factors can typically be avoided, albeit not always:
- Alcohol intoxication (being drunk): If you drink in moderation or not at all, you can prevent ataxia from this. It is also possible for certain individuals to have medical disorders such as alcohol intolerance, which makes it more difficult for them to prevent ataxia when they drink.
- Concussions and traumatic brain injuries: The chance of ataxia resulting from brain trauma can be decreased by using safety equipment, such as helmets.
- Drugs (prescription and recreational, especially medications for epilepsy and depression): One method to prevent ataxia from recreational drugs is to abstain from them. It is advisable to consult with your healthcare practitioner before stopping a recommended medicine if you experience ataxia. It’s safer to discuss abrupt medication cessation with your provider to avoid potentially dangerous side effects or consequences.
- Fatigue and stress: One important strategy to prevent ataxia caused by exhaustion is to get adequate sleep. Stress management is also crucial.
- Huffing substances like toluene, gasoline, glue, spray paint, and other inhalants: Huffing has numerous potential side effects, ataxia being only one. This kind of inhalant abuse is risky, therefore it’s advisable to refrain from doing it or to quit using it right away.
- Infections (these can happen because of bacteria, viruses, parasites, and fungi): One of the most important things you can do to prevent ataxia from damaging your ears, nervous system, or brain is to treat infections, particularly ear infections, which can cause balance problems.
- Reaching and maintaining a healthy weight: Your weight and physical health are related to numerous disorders that impact the blood flow to your brain, including stroke. Maintaining your physical well-being can occasionally stop, or at least postpone, the emergence of situations that may lead to these issues.
- Toxic exposure to chemicals, metals, or substances (such as mercury, lead, etc.): One strategy to prevent ataxia from occurring is to stay away from harmful materials. Wearing safety gear and adhering to safety regulations is crucial if you have to operate near hazardous compounds.
- Vitamin deficiencies and nutrition-related problems (such as low vitamin B12 levels): A well-balanced diet will assist you in preventing the nutritional deficiencies that cause ataxia.
When to see a doctor
See your doctor right away if you do any of the following, provided you do not currently have a disease like multiple sclerosis that causes ataxia:
- Lose balance.
- Have a loss of hand, arm, or leg muscular coordination.
- Have trouble walking.
- Slur your speech.
- Have trouble swallowing.
When should I call my healthcare provider?
The kind of ataxia may have different symptoms and start times. Every individual may have distinct symptoms. Any of the following symptoms should prompt you to call your provider:
- Issues with coordination and balance.
- Inability to coordinate hands, arms, or legs.
- Slurring of speech.
- Wide-based gait (manner of walking).
- Trouble eating and writing.
- Slow eye movements.
Atherosclerosis symptoms can mimic other illnesses or medical issues. For a diagnosis, always see your medical professional.
Conclusion
A loss of control and coordination in the muscles is called ataxia. Individuals suffering from ataxia experience difficulties with fine motor skills, mobility, and maintaining their balance.
Ataxia may occur spontaneously, be hereditary, or have no known cause. Depending on the type of ataxia, symptoms, progression, and age of start can change.
Ataxia symptoms may occasionally be relieved by attending to the underlying cause. Other choices that might help control symptoms and enhance the quality of life include medications, assistive technology, and physical therapy.
If symptoms such as speech impediment, difficulty swallowing, or lack of coordination cannot be attributed to another illness, consult your physician.
Your doctor will collaborate with you to diagnose your disease and create a treatment plan.
FAQs
Does ataxia ever go away?
While ataxia has treatable causes, many do not, necessitating medical intervention to control symptoms.
Is ataxia a serious condition?
Depending on the etiology, ataxia can frequently be a dangerous condition. For instance, by the time they are 45 years old, patients with Friedreich ataxia are frequently confined to wheelchairs. The average age of death, which is typically brought on by cardiac issues, is 36.5 years.
Is ataxia a form of dementia?
There are spinocerebellar ataxia forms that can mimic dementia symptoms.
What is ataxia a symptom of?
Most often, ataxia is caused by injury to the cerebellum or its connections in the brain. The cerebellum regulates the coordination of muscles. Several illnesses, including genetic disorders, strokes, tumors, multiple sclerosis,
degenerative diseases, and alcohol abuse, can result in ataxia.
What are the 3 types of ataxia?
It is caused by malfunctions in the brain regions that control movement coordination, most frequently the cerebellum. Based on the site, ataxia can be classified as vestibular, cerebellar, or sensory.
What is another name for ataxia?
An uncommon hereditary condition known as ataxia telangiectasia (A-T) affects numerous bodily systems, including the immune system and brain system. Dilated blood vessels and impaired coordination are characteristic symptoms of the illness, which is also known as Louis-Bar syndrome.
What are the 3 causes of ataxia?
Ataxia can result from a variety of situations or conditions, such as:
Alcohol intoxication, or being wasted.
Brain tumors (or other cancerous conditions).
Celiac disease.
Congenital disorders are illnesses that affect you from birth, like Chiari malformation.
Traumatic brain injury and concussions.
Who suffers from ataxia?
Although ataxia can affect anyone at any age, some forms are more prevalent in particular age ranges. For instance, a diagnosis of Friedreich’s ataxia is typically made during puberty or childhood.
What age does ataxia start?
The onset of symptoms usually happens between the ages of five and fifteen, but they can also happen after twenty-five. One or more of the following are possible signs of FA: shaky, awkward movements and deteriorating muscular coordination (ataxia).
Does ataxia show up on MRI?
The following tests are typically used to identify ataxia: brain imaging scans (MRI); a thorough clinical evaluation that includes a personal medical history, family history, and neurological examination.
What is ataxia in neurology?
Many neurological disorders, such as stroke, brain tumors, multiple sclerosis, traumatic brain injury, toxicity, infection (especially varicella virus), and congenital cerebellar abnormalities, can cause ataxia, or a lack of coordination. It may develop in an acute, subacute, episodic, or chronic manner.
Can you live a long life with ataxia?
For those with genetic ataxia, life expectancy is typically lower than average, while others can live well into their 50s, 60s, or older. In more extreme situations, the illness may be deadly in a child’s early years of maturity. The prognosis for acquired ataxia is dependent on the underlying etiology.
How long does it take to recover from ataxia?
Sudden onset of ataxia with symmetric gait. May also have nystagmus and mild dysarthria. Ataxia is at its worst at first and typically gets better in a few days. In most cases, full recovery happens in 10 to 21 days (>90% resolve in 2 months).
Can ataxia be treated?
Supplemental vitamin E can frequently be used to improve or control ataxia caused by vitamin E deficiency. Acetazolamide is a medicine that is frequently used to treat episodic ataxia, along with avoiding triggers like stress, alcohol, and caffeine.
Is exercise good for ataxia?
Numerous physical activities appear to be helpful in the treatment of cerebellar ataxias, according to the research. A balance trainer can help with ataxia and balance, especially if the workouts are hard. Gait and balance are improved with treadmill exercise.
Can ataxia be stopped?
Depending on the specific type of ataxia you have, there are different treatment options. While treating the underlying cause of the problem can sometimes make it better or prevent it from getting worse, this isn’t always possible, and your symptoms will be treated instead.
References
- Ataxia. (n.d.). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-anddiseases/ataxia
- Imagewww.myupchar.com%2Fen%2Fdisease%2Fataxia&psig=AOvVaw1bLUYlPK5v8TLupeNGpfkh&ust=1714285244336000
- Ataxia – Symptoms and causes – Mayo Clinic. (2024, January 30). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/ataxia/symptoms-causes/syc-20355652.
- Professional, C. C. M. (n.d.). Ataxia. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/17748-ataxia.
- Ataxia. (2024, April 15). Wikipedia. https://en.wikipedia.org/wiki/Ataxia.
- Seladi-Schulman, J. (2023, December 19). Everything to Know About Ataxia. Healthline. https://www.healthline.com/health/ataxia#prevention.
- Ataxia. (n.d.). Physiopedia. https://www.physio-pedia.com/Ataxia.