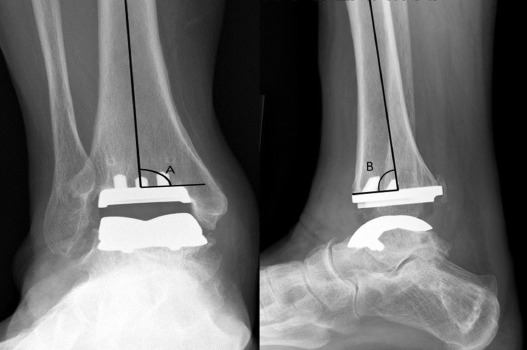
Total Ankle Arthroplasty And Physiotherapy Treatment
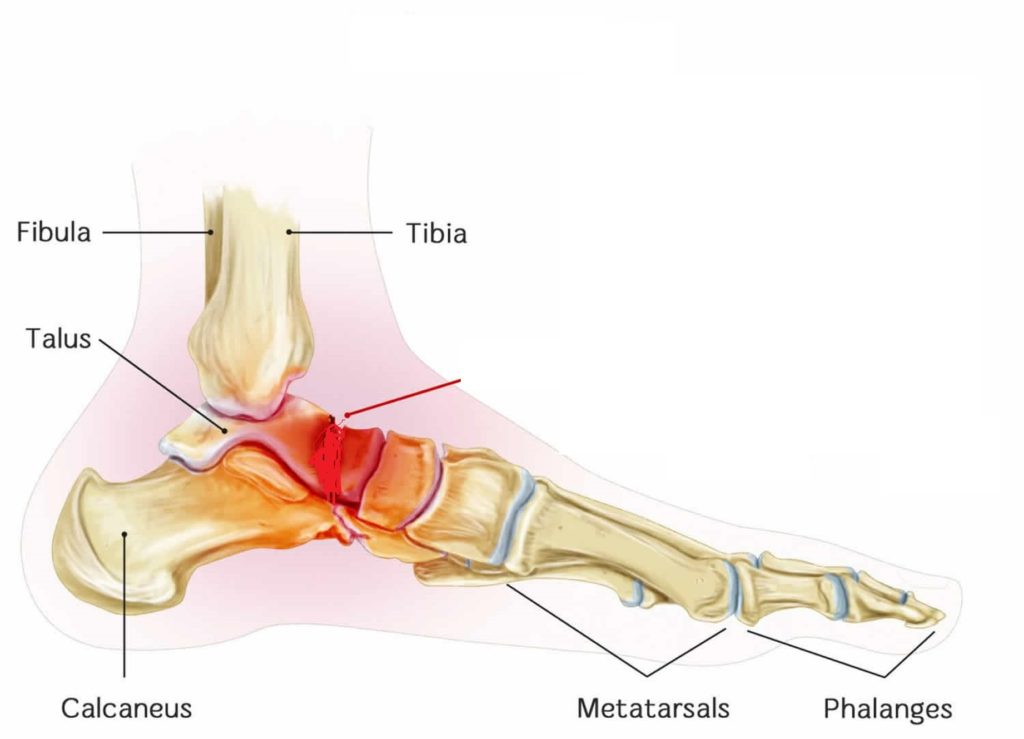
- Ankle arthroplasty is when the ankle joint (Talocrural Joint) is replaced with prosthetic components comprised of polyethylene and metal and is preferred to ankle arthrodesis (fusion) as A range of movement and function a not compromised.
Main objectives of the arthroplasty are to
- Replicate ROM of the talocrural joint
- Function well under weight-bearing
- Be wear-resistant
- Maintain alignment and stability
The Arthroplasty
Indication for Procedure
- There is no well-defined indication for a Total Ankle Arthroplasty. Surgery is considered only when conservative treatment has been attempted with no improvement.
- The operation is mainly being executed in patients who suffer from different types of arthritis. This causes advanced arthritic changes in disabling pain and loss of ankle motion.
- The ankle is most frequently affected by post-traumatic arthritis. Total ankle joint replacement is also indicated following unsuccessful ankle arthrodesis the ‘ideal’ patient for ankle joint replacement is an elderly person with low physical demands who have good bone stock, normal vascular status, no immune-suppression, and excellent hind foot-ankle alignment. Generally here are common indications for arthroplasty:
- Primary or post-traumatic osteoarthritis
- Severe rheumatoid arthritis
- Rejected arthrodesis
Indications of Total Ankle Arthroplasty :
- According to Saltzman, there are no exact indications for receiving a total ankle arthroplasty.
- The “ideal” patient who would typically undergo this intervention is one who is elderly with healthy immunity, normal vascular status, good bone density, and a proper hindfoot-ankle alignment who has not had success with conservative treatment measures.
- Individuals with debilitating ankle arthritis, unresponsive to nonoperative approaches, or have failures with the outcome of their ankle arthroplasty are typically treated with an arthrodesis procedure to fuse the joint.
Contraindications of Total Ankle Arthroplasty :
- Arthroplasty is contraindicated for those with neuroarthropathic degenerative joint disease, infection, avascular necrosis of the talus, osteochondritis dessicans, malalignment of the hindfoot-ankle, severe benign joint hypermobility syndromes or soft tissue problems, or decreased sensation or motion in the lower extremities.
- In individuals with rheumatoid arthritis (RA), inflammatory processes may occur before signs of swelling, tissue reaction, and joint destruction are seen.
- In the first and second year of this disease process, structural damage (ie. joint erosion) can be seen with X-ray imaging. Diabetic patients may develop gouty arthritis in their ankle joints. This is caused by uric acid changing into urate crystals, which is deposited into the joint.
- Thus, RA and diabetic individuals may or may not be candidates for ankle arthroplasty depending on the severity of joint degeneration found with radiographic imaging.
- Common contraindications are:
- Severe talus subluxation, severe valgus or varus deformity
- Substantial osteoporosis
- Neurological disorders or recurrent infection
Physio Therapy Management of Total Ankle Arthroplasty
- As it will be explained in the pre-operation and post-operation phase the multi-disciplinary team involved with the patient have a big role in making the arrangements before and after the surgery, this may involve physiotherapists, occupational therapists, discharge nurses, staff nurses, healthcare assistants as well as doctors.
- Both pre and post-operative phases are integral to the progress of the patient and the pre-op should not be overlooked as important as it can be easy to focus on post-op.
Pre-Operative Phase
- Before the surgery one of the main job for the team is to educate the patient about what will happen before, during and after the surgery as this will give the patient the opportunity to prepare, mentally rehearse, ensure a smooth transition through short-term to long-term goals but also help control and reduce post-operative pain (level of evidence 3B)
- ROM, muscle strength, gait, and deviations will all be recorded as compared before and after arthroplasty and ensure the patient is as optimal strength prior to operation if possible.
- For safety and ease of transition is can be important that the patient learns how to walk with crutches so they can perform ADLs as soon as possible post arthroplasty but also understand that they will be non-weight bearing after the arthroplasty. (Level of evidence 4)
- As will all procedures under general anesthetic there are common pulmonary postoperative complications (PPC’s) that need to be controlled and risk reduced and this can be explained at this stage as well.
Post-Operative Phase
- It is important to ensure the risk of PPC’s is reduced and respiratory physiotherapy may be used at this early stage, cough, deep breathing exercises and early mobility are essential here to reduce atelectasis and reinstate the mucociliary elevator as soon as possible.
- Atelectasis occurs in 90% of anesthetized patients which leads to a 16-20% reduction in functional residual capacity which is why the alveoli tend collapse resulting in increased work of breathing, hypoxia, reduced compliance, V/Q mismatch, and risk of pneumonia.
- (Level of evidence 5)T(Level of evidence 5)here is a 9% chance of developing pneumonia and this is where physiotherapy intervention is crucial at reducing the rate of all of these complications.
Physio Therapy Goals:
- Decrease pain
- Decrease inflammation
- Increase strength
- Increase range of motion
- Improve dynamic and static balance
- Improve proprioception
- Proper independent ambulation
Assessment
- Mechanism of injury or etiology of illness
- Date of surgery and type of implant
- Use of assistive device with weight-bearing status
- Use of controlled ankle motion (CAM) walker/walking boot
- Functional deficits/assistance with ADLs/adaptive equipment
- Pain/ Symptom history: Location, duration, type, intensity (VAS), aggravating and relieving factors, 24-hour symptom behavior
- Relevant Current/Past Medical history: Other lower extremity arthritis or injuries, upper extremity issues that may limit the ability to ambulate with an AD and comorbid diagnoses
- Medications for current/previous diagnoses
- Diagnostic tests
- Sleep disturbance
- Barriers to learning
- Social/occupational history
- Patient’s goals
- Vocation/avocation and associated repetitive behaviors
- Living environment
- Relevant Tests & Measures:
- Observation/inspection/palpation: Skin and incision assessment, edema, muscle atrophy
- Circulation: Dorsal pedal pulse
- Sensory and proprioception testing
- Range of motion and Muscle length: Average postoperative arc of motion (dorsiflexion and plantarflexion) is 23°.
- Muscle strength
- Posture: Increased pronation/supination in standing, ability to maintain the weight-bearing status
- Assess assistive and adaptive devices for need and proper fit
- Balance: Static and dynamic standing balance, the unilateral balance of the unaffected extremity (especially if the patient is still non-weight bearing).The patient may demonstrate dynamic postural imbalance, less reliance on ankle strategy, and de?cit of motor control ability.
- Functional mobility
- American Orthopaedic Foot and Ankle Society ankle-hindfoot score, Outcome measures
- Self-selected normal walking speed
- Assess safety in mobility
- Gait Assessment
- Initial Rehab 0-4 Weeks
- Restrictions:
- Non-weight bearing 2/52 with a back slab
- Below knee POP at 2/52 and begin full weight-bearing in this POP
- POP removed at 4/52 and aircast boot is considered
- Elevation
- If sedentary employment, return to work at 4/52 as long as elevated and protected
- Goals:
- Safe and independent mobility with a walking aid
- Independent with an exercise program
- Know monitoring and protection
Treatment:
- POP
- Pain-relief
- POLICE
- Basic circulatory exercises
- Mobility
- Progress when:
- Out of POP, fully weight-bearing, no complications and then refer to physiotherapy outpatients
Recovery Rehab 4 weeks – 3 months
- Restrictions: No strengthening against resistance until 3 months if any tendon transfers
- No stretching tendons if transferred
- Goals:

- Independent from aircast boot
- Achieve full ROM
Treatment:
- Pain relief, swelling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises –> PROM,AAROM, AROM, light strengthening, core stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy –> SSTM’s, mobilizations
- Progress when:
Full ROM, independently mobile, neutral foot position in standing
Intermediate Rehab 12 weeks – 6 months
- Restrictions: None
- Goals: Independent with no aids
- Normal footwear
- Grade 5 strength
Grade 4 strength in tendons transferred
Treatment:

- Pain relief, swelling management
- Advice, education, postural advice, monitoring complications, pacing
- Gait re-education
- Exercises –> PROM,AAROM, AROM, light strengthening, core stability, balance/proprioception, stretching
- Hydrotherapy
- Orthotics
- Manual therapy –> SSTM’s, mobilizations
- Progress when:
Normal footwear, independent with no aids, pain controlled, strength 5/5 (4/5 if tendon transferred)
Final Rehab 6 months – 1 year
Goals:

- Return to gentle no-impact/low impact sports
- Grade 5 strength in transferred tendons
- Treatment:
- Maximize function
- End-stage exercises, balance and proprioception, and sport-specific
- Manual therapy
- Muscles to Consider
- Here is an unfinished list of some of the major muscles of the lower leg and foot, consider these in your rehabilitation and mechanism of pathology. Some may have had tendons moved or stretched and now need to be specifically rehabilitated as the proprioceptive function may now have changed.
- Posterior Compartment – Superficial
- Gastrocnemius
- Plantaris
- Soleus
- Posterior Compartment – Deep
- Popliteus
- Flexor Hallucis Longus
- Flexor Digitorum Longus
- Tibialis Posterior
- Lateral Compartment
- Peroneus Longus
- Peroneus Brevis
- Anterior Compartment
- Tibialis Anterior
- Extensor Hallucis Longus
- Extensor Digitorum Longus
- Peroneus Tertius