Bertolotti’s Syndrome
What is Bertolotti’s Syndrome?
Bertolotti’s Syndrome is a condition involving a congenital spinal anomaly where there is a lumbosacral transitional vertebra (LSTV) that can cause chronic lower back pain. This anomaly typically involves the fifth lumbar vertebra (L5) and the sacrum, where the transverse process of the L5 vertebrae is enlarged and may fuse with the sacrum or the iliac bone, leading to changed biomechanics and possible nerve compression. Though not always symptomatic, when symptoms occur, they often include persistent lower back pain, sciatica-like symptoms, and reduced mobility.
Up to 8% of people have this illness, which needs to be properly diagnosed in order to be treated.
The most common kind of LSTV is the growth of unilateral or bilateral L5 transverse processes with the fusion of one or more of those transverse processes to the sacrum.
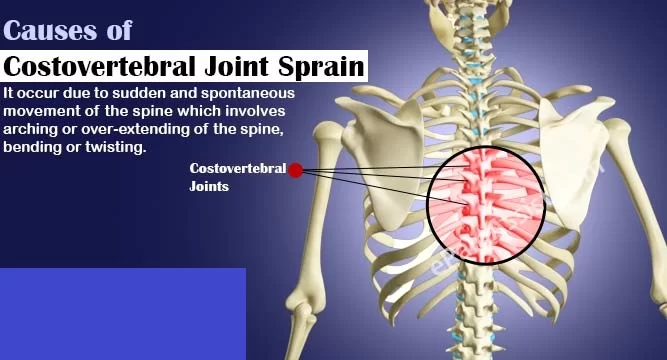
The sacrum, the base of the spinal column, is in the role of distributing the upper torso’s weight over the pelvis. However, when the sacrum is unevenly fused with L5, it affects the sacrum’s capacity to distribute the upper body’s weight effectively. To enable load bearing across the reduced sacral surface area, patients with an LSTV have longer L5 transverse processes than those without one. As a result, there is less motion at the L5-S1 intersection and more motion overall.
Disc herniation and facet arthrosis are more common as a result of this increase in motion at anatomically normal spinal levels. These abnormalities between L5 and S1 cause asymmetry in spinal movement and an increase in stress on the vertebral level preceding it, which is thought to be the source of pain in the majority of the cases.
Imaging scans are usually used to confirm the diagnosis. Depending on the severity of the symptoms, treatment choices vary from conservative management—such as physical therapy and pain relief—to additional interventions—such as injections or surgery.
What are the Causes of Bertolotti’s Syndrome?
Bertolotti syndrome’s cause is yet unclear. Many family members have been reported to have lumbosacral transitional vertebrae, which raises the possibility of an underlying hereditary component. Mutations in the HOX10/HOX11 genes are thought to play a role in the creation of an LSTV. The vertebral column is divided into several levels by HOX genes, also referred to as homeobox genes.
Additionally, biomechanical elements, such as how a person’s body weight is distributed across the SI joints, have an impact on the establishment of the lumbosacral junction. As of right now, the origin of Bertolotti syndrome is thought to be complicated and needs more research.
The specific causes include:
- Congenital Anomaly
- Altered Biomechanics
- Nerve Compression
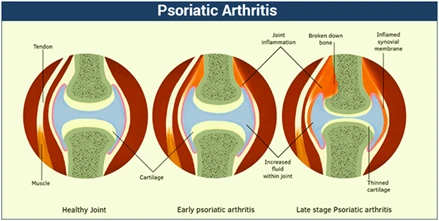
- Degenerative Changes
What are the Symptoms of Bertolotti’s Syndrome?
The degree of related complications and the severity of the lumbosacral transitional vertebra (LSTV) can affect the symptoms of Bertolotti’s Syndrome. Typical signs and symptoms include:
- Lower Back pain: The most typical symptom is chronic, persistent lower back pain. Mostly, the lumbosacral joint junction is the most common site of the pain.
- Symptoms like sciatica: Some people may have sciatica-like radiating pain that goes from the lower back down the legs and buttocks. This happens when the deformity compresses or irritates the nerves in the surrounding area.
- Reduced Flexibility and Mobility: The abnormal structure and mechanics of the spine may result in stiffness and a restricted range of motion in the lower back.
- Pain During Physical Activity: Bending, twisting, or lifting are examples of physical activities that might make pain worse. Extended periods of standing or sitting can exacerbate symptoms as well.
- Asymmetrical Pain: Depending on the unique structure of the transitional vertebra and how it interacts with the surrounding tissues, the pain may be more intense on one side of the lower back or buttocks.
- Muscle spasms: Lower back pain and discomfort may be exacerbated in certain people by lower back muscle spasms.
- Intermittent Pain: This type of pain is not always present and can change in severity, sometimes getting worse in response to particular movements or positions.
Sometimes people with Bertolotti’s Syndrome don’t show any symptoms at all and the disorder is only accidentally discovered during imaging for other purposes. When symptoms occur, though, they can have a major effect on day-to-day functioning and require medical attention.
Classification of Bertolotti’s Syndrome
Jenkins Classification
By using the Jenkins Classification, Bertolotti’s Syndrome is categorized.
- Type 1: A dysplastic transverse process with a gap across the lumbosacral junction of greater than 2 mm but less than 10 mm.
- Type 2: A gap of less than 2 mm between adjacent transverse processes that seem to be pseudo-articulated.
- Type 3: Full fusion of the lumbosacral junction, without spontaneous fusing of the disk or facet joints, lateral to the facet at the ala.
- Type 4: One-sided fused side with contralateral pseudoarticulation (Type 4A, 4B, or 4C).
Subclassifications of Type 1, 2, 3, and 4:
- L (left) or R (right) prominence
- A (unilateral
- B (bilateral)
- C (Type 2 with Type 1 and contralateral 2 anatomy Type 4 with a gap > 10 mm and contralateral Type 3 anatomy), + L (left) or R (right) iliac contact.
Epidemiology
According to reports, the general population has a 4% to 8% incidence of Bertolotti syndrome. An LSTV, on the other hand, occurs significantly more frequently—between 4% and 30%.
Many experts think the diagnosis of Bertolotti syndrome has been significantly underdiagnosed as a result of this disparity. Males are more than twice as likely as females to have an LSTV linked to pain, regardless of this heterogeneity.
Further research has revealed that sacralization of L5 is more common in males, but sacral lumbarization and the existence of an auxiliary articulation between L5 and S1 are more common in females.
Pathophysiology
Pain may accompany an LSTV for a number of reasons, including the abnormal anatomy and mobility of the lumbosacral junction in patients with Bertolotti syndrome.
One iliolumbar ligament anomaly could be the source of Bertolotti syndrome. The iliolumbar ligament helps to stabilize the spinal column in an anatomically normal spine that functions normally. In contrast to its contralateral counterpart, a new study indicates that the iliolumbar ligament, which is situated on the side of the abnormal articulation in patients with Bertolotti syndrome, is significantly underdeveloped.
While discogenic pain and lumbar radiculopathy are two related causes that may confuse the clinical picture, transitional articulation may seem to be the most prominent source of pain. Disc herniations and facet joint degeneration at the spinal level above the LSTV have been found to be associated with the presence of an LSTV.
Compared to the disc between the sacrum and the transitional vertebra, the disc directly above the transitional segment—likely L5-S1—has frequently deteriorated at much faster rates.
Bertolotti syndrome has been consistently shown to have intervertebral foramen stenosis, most likely as a result of degenerative alterations at the facet joints above the long sagittal plane.
Diagnosis
History
A comprehensive medical history can aid in distinguishing between the potential causes of back pain. Back pain is a common complaint among patients with Bertolotti syndrome, although it can be confused with other pain causes. To determine whether the patient may be concurrently experiencing facet pain, sacroiliac pain, radicular pain, or other types of discogenic back pain, a specific examination is necessary.
Physical Examination
Patients who are suspected of having Bertolotti syndrome should have a complete spine exam to rule out other disorders such as neurogenic claudication, lumbar radiculopathy, degenerative disc degeneration, and lumbar spondylosis. During physical examination, there may be painful areas to the touch or nonspecific sensitivity. In the office, they might also exhibit a reduced range of motion. To rule out other neurological causes of pain, provocation movements, reflexes, sensation, and muscular strength should all be thoroughly assessed.
Evaluation
A precise diagnosis of Bertolotti syndrome requires imaging. In most cases, plain radiographs of the pelvis and lumbar spine can reveal the lumbosacral transitional vertebrae with sufficient diagnostic information. These need to be used as primary imaging modalities as they are rapid, reasonably priced, radiation-free, and minimize radiation. Particularly useful could be an AP image of the lumbosacral junction with 30 degrees of cephalad angulation, known as a Ferguson radiograph.
Upon review of these radiographs, one or both of the L5 transverse processes may be enlarged, or there may be an L5 apophysis articulating with the sacrum. On simple radiographs, the sacroiliac joints typically appear normal.
Computed tomography (CT) is a type of advanced imaging that can provide a more detailed picture of the lumbosacral junction than plain radiography, particularly in patients whose body habitus hides the imaging. On CT imaging, osteophyte development and the degree of fusion at the articulation point can be examined more closely. Other lumbar diseases, such as degenerative lumbar intervertebral discs and disc herniations, annular tears, and fissures, can also be seen by magnetic resonance imaging (MRI), as can regions of neural stenosis.
In addition to these extra advantages of sophisticated imaging, vertebral numbering—which is important for treatment planning and may not be visible on ordinary radiographs—can be aided by CT and MRI scans.
No specific laboratory test is needed for the diagnosis. Labs could be used, nevertheless, to rule out further inflammatory or malignant processes. An electromyogram (EMG) of the lower limbs may also be performed if the patient exhibits any degree of radicular symptoms in order to distinguish between peripheral neuropathies and lumbar radiculopathies.
Treatment of Bertolotti’s Syndrome
The first line of treatment for Bertolotti syndrome should be cautious. Nonsteroidal anti-inflammatory medicines (NSAIDs) are inexpensive, usually well tolerated, and may offer considerable relief.
At the time of diagnosis, physical therapy (PT) may also be suggested concurrently. Treatments for PT include strengthening core muscles, increasing spinal mobility, and offering additional pain-relieving techniques.
Injection treatment may be required for the patient if physiotherapy and NSAIDs are unable to offer sufficient pain relief. Pain alleviation from directed corticosteroid injections into the abnormal articulation is very effective and can persist for a short while, if not forever, with fluoroscopic guidance.
In addition to its possible therapeutic benefits, injection therapy can help identify a patient’s source of discomfort and provide guidance for long-term care.
Only those who have not responded to these previously suggested conservative measures should consider surgery. If the false articulation has been identified as the primary cause of pain, then the first surgical option may be the resection of the swollen transverse process involved in the LSTV, either unilaterally or bilaterally.
When there is an instability of the spine at the L5-S1 segment, spinal fusion might be necessary. Fusion could result in long-lasting alleviation, but it might also speed up the degeneration of nearby segments. If there is a central canal or foraminal stenosis that is causing symptoms, a decompressive procedure can also be necessary. Osteophyte production, which may also be a cause of extraforaminal stenosis, may be aided by pseudo articulation.
Each patient should have a distinct surgical treatment tailored to their radiography findings and symptomatology.
Physiotherapy Treatment
For Pain relief:
- Manual Therapy: Techniques for joint mobilization, myofascial release, and soft tissue mobilization are helpful in minimizing stiffness and enhancing stability.
- Electrotherapy: Ultrasound therapy and TENS (Transcutaneous Electrical Nerve Stimulation) techniques are instrumental in relieving pain and inflammation of the body.
Posture Correction and Ergonomics:
- Postural training: It is important to avoid bad posture in order not to worsen the symptoms. In maintaining spinal alignment during everyday activities physical therapists may help.
- Ergonomic tip: Switching work positions while lifting or sitting down; improving body mechanics could help keep one back pain-free.
Strengthening Exercises and Stabilization:
- Core strengthening: In order to alleviate the discomfort, it is important that we build strength in those muscles supporting our back such as those found on the pelvis or abs area.
- Spinal stabilization exercises: They include hip abduction, pelvic tilt, or bridging exercises which align as well as stabilize your spine thereby helping manage symptoms.
Flexibility and Mobility:
- Stretching: Gentle stretches that focus on hips, hip flexors, and lower back muscles can help release tension and improve flexibility
- Mobility exercises: It is important to do exercises to maintain or increase the range of motion of the hips and spine to prevent stiffness.
Lifestyle changes:
- Patient education: Chronicly managing this disease involves instructing individuals with it on their own ailment, the significance of physical activity on a regular basis, and how to handle pains
- Movement modifications – It is important to counsel patients to modify or avoid activities such as sitting for long periods of time or lifting extra weights.
Advanced Treatment for Physiotherapy:
- Dry needling: One technique that can be used to reduce myofascial pain caused by surrounding muscle rigidity is dry needling.
- Athletics Taping techniques will help in lessening the strain on lower backs as well as providing support while performing various exercises.
Differential Diagnosis
Unspecified low back pain is the most common sign of patients with Bertolotti syndrome. Sadly, there are a lot of differential diagnoses for low back pain, and many of them might exist concurrently and result in a multifactorial cause. It is important to take neurological, oncological, and musculoskeletal diseases into account.
Common causes of back pain are lumbar strains, degenerative disc disease, herniations, annular tears/fissures, lumbar facet arthropathy, facet cysts, Tarlov cysts, scoliosis, and sacroiliac joint pain.
A thorough physical examination and history-taking can aid in ruling out a number of these additional diseases.
In addition, to lower back pain, physicians should rule out compressive lumbar diseases such as radiculopathy and lumbar stenosis/claudication when patients present with leg symptoms.
These conditions should be taken into account in addition to Bertolotti syndrome, but not exclusively since lumbar stenosis and radiculopathy can also cause back pain because of separate underlying causes. As a result, having concurrent causes for back pain may be rather common.
Furthermore, neoplastic processes must not be disregarded. Severe weight loss or gain, intractable night pain, and other unexplained lower back pain that is not resolved by conservative therapy should raise suspicions of a primary or malignant tumor of the lower back area.
A malignancy can be diagnosed with the aid of appropriate imaging and laboratory testing, and if one is found, the patient should be referred for appropriate oncologic treatment.
Prognosis
Undiagnosed cases of chronic back pain may be caused by Bertolotti syndrome. Conservative measures like medication, physical therapy, and steroid injections have been demonstrated to have differing effects and to be able to offer either short-term or long-term relief.
After trying all of these non-invasive therapies, patients who have surgery typically report feeling better about their lives, although their symptoms may not completely go away.
In the end, every patient should be treated uniquely, taking into account their demands and lifestyle.
Complications of Bertolotti’s Syndrome
The LSTV in Bertolotti syndrome is a nidus for abnormal spinal mechanics and movement. As a result, more stress is often distributed among the nearby motion segments. Neural stenosis may result from arthrosis, faster disc and facet joint degradation, and higher stresses applied to the neighboring segment.
There are common risks associated with surgical treatment for Bertolotti syndrome. The risks associated with surgery include infection, bleeding at the surgical site, and the need for additional surgeries if the initial one doesn’t work. Because the surgery is so close to the spinal cord and the nerve root canal, there is an additional danger of nerve damage from these treatments.
Even though surgical problems are uncommon, it is crucial to talk to the patient about them.
Education for Patients and Prevention
Bertolotti syndrome is a birth defect. Although it is impossible to prevent chronic pain, patients may be able to avoid its aftereffects by receiving frequent and early patient education. For this reason, it’s essential to diagnose this illness as soon as possible and accurately.
As soon as an abnormal link or structure inside the spine is discovered, patients should be advised of it and given advice on how it can impact their mobility and quality of life. In an effort to lessen any muscle tension caused by the incorrect spinal connection, they should also receive information on preventative stretching and rehabilitation and counseling regarding the significance of maintaining their current level of activity.
Improving the Results of Healthcare Teams
A patient with Bertolotti syndrome may receive care from a variety of healthcare professionals. When completing a workup, the first person a patient talks to about chronic back pain should consider the potential of a lumbosacral transitional vertebra. A chiropractor, physician’s assistant, nurse practitioner, or primary care physician may be responsible for this task. Conservative yet diagnostic procedures like radiographic imaging, pain medication, and the opportunity to be transferred to a pain management specialist if the problem worsens should all be part of their treatment.
If the patient sees a pain management doctor, the doctor has to stay in constant contact with the patient’s primary care physician to ensure a smooth transfer of diagnosis, test results, and available treatments. For therapeutic or diagnostic objectives, the pain management physician may administer fluoroscopic guided injections. With careful monitoring in mind, they may also prescribe a wider range of painkillers.
Instead of seeing a pain management specialist, the patient can see a surgeon to have their abnormal vertebral connection permanently removed. In addition to recommending conservative treatment, the surgeon may advise surgery to ease the patient’s pain and reduce the possibility of LSTV sequelae in the future. For a patient with Bertolotti syndrome, effective communication amongst all members of the interprofessional healthcare team is crucial to a proper diagnosis and course of therapy.
References
- Pandya, D. (2023, October 21). Bertolotti’s Syndrome – Cause, Symptoms, Treatment. Samarpan Physiotherapy Clinic. https://samarpanphysioclinic.com/bertolottis-syndrome/#Physiotherapy_Treatment
- Miller, A. E., & Zhang, A. (2023, July 25). Bertolotti Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK585032/
- Bertolotti’s syndrome. (2024, April 28). In Wikipedia. https://en.wikipedia.org/wiki/Bertolotti%27s_syndrome