Fracture of the Lateral Tibial Plateau
Introduction
- A tibial plateau fracture is a break that occurs into the knee joint itself from the greater lower leg bone below the knee. A bone that is only slightly broken is uncommon. The bone, meniscus, ligaments, muscles, tendons, and skin surrounding the knee may all be affected by this injury.
- it is a type of shinbone break that affects the knee joint and occurs in the upper tibia. Pain, edema, and a reduction in knee mobility are among the symptoms.
- Most people are incapable of walking. Arthritis, compartment syndrome, and damage to the artery or nerve are examples of complications.
Trauma from an accident, such as a fall, is usually the reason. Two risk factors include osteoporosis and participation in specific sports, such as going skiing. X-rays and a CT scan are usually used to confirm the diagnosis, which is usually assumed based on symptoms. Certain fractures might not be visible on standard X-rays. - Opioids, NSAIDs, and bracing are options for treating pain. Surgery is typically used as a kind of treatment for persons who are otherwise healthy. Sometimes patients can receive treatment without surgery if their knee ligaments are unharmed and their bones are in a straight line.
Signs and Symptoms
- Swelling
- Inability to weight bear
- Bruising
- Reduced knee range of movement (ROM)
- History of trauma
- Pain
- A tibial plateau fracture usually manifests as knee effusion, knee swelling, or tibial fragmentation, which results in the loss of the tibia’s natural structural look. Bruising and a doughy sensation in the knee joint can result from hemorthrosis, or blood clots in the soft tissues and knee joint.
- Owing to the proximity of the tibial plateau to significant vascular and neurological structures, including peroneal and tibial nerves, damage to these structures may arise upon fracture. It is essential to thoroughly examine the neurovascular systems.
- Compartment syndrome, a dangerous consequence of tibial plateau fractures, is characterized by swelling that compresses the leg’s blood vessels and nerves, potentially resulting in necrosis or cell death of the leg tissues.
Causes
- High-energy and low-energy tibial plateau fractures are the two forms that exist. Because of alterations in the osteoporotic bone, low-energy fractures, which are usually depressed fractures, are frequently observed in older females.
- High-energy fractures are frequently the consequence of falls, auto accidents, or injuries sustained in sports. The majority of tibial plateau fractures in young people are caused by these factors.
Mechanism
- Tibial plateau fractures are brought on by an axial loading or weight bearing on the knee in combination with a varus (inwardly angling) or valgus (outwardly angling) force. This is typically described as happening when an automobile hits a pedestrian’s fixed knee, or “bumper fracture” for short. Nonetheless, falls or auto accidents account for the majority of these fractures.
- An injury may result from a fall from a height that forces the knee into a varus or valgus position. The opposing, unbroken femoral condyle crushes or splits the tibial condyle. Understanding the anatomy of the knee can help predict why some fracture types occur more frequently than others. Compared to the lateral plateau, the medial plateau is stronger and larger.
- Additionally, there is a valgus or The lateral side will be injured due to the limb’s outward angulation alignment and the frequent valgus or outwardly angulating power during impact. This explains why the lateral plateau accounts for 60% of plateau fractures, the medial plateau for 15%, and the bicondylar lesions for 25%. About 5–37% of all tibial plateau fractures result in meniscal lesions, while 15–45% of fractures involve partial or total ligamentous ruptures.
Classification
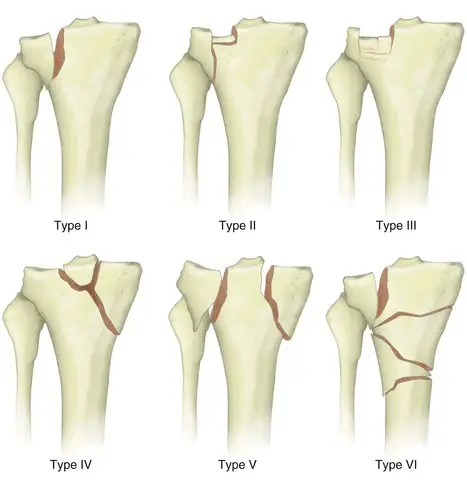
- Classification types are used by doctors to determine the extent of harm, create a treatment plan, and estimate prognosis. There are several different categories for tibial plateau fractures. The most generally recognized and utilized classification scheme at the moment is the Schatzker one.
- It is divided into six categories based on the fragment anatomy and fracture pattern of the condyle fracture. Growing severity is indicated by each increasing numeric fracture type. The degree of energy applied to the bone at the moment of injury and the prognosis are correlated with each other.
- Type I: Fractures of the lateral tibial plateau without depression.
The lateral tibial plateau is vertically split in this wedge-shaped pure cleavage fracture. When it occurs in young people with normal mineralization, it usually results from a low-energy injury. may result from axial loading and a valgus force that pushes the lateral femoral condyle into the tibial plateau’s articular surface. make for 6% of all fractures of the tibial plateau. - Type II: Depression and lateral tibial plateau fracture
This is a combination of cleavage and compression fracture that causes the lateral condyle to split vertically and the surrounding load-bearing portion of the condyle to sink. due to a valgus force acting on the knee; it is a low-energy injury that is usually observed in people with osteoporotic bone abnormalities who are four decades of age or older. most frequent, accounting for 75% of all fractures of the tibial plateau. Distraction injuries to the medial collateral ligament have a 20% chance of occurring. may involve an anterior cruciate ligament or medial collateral ligament distraction injury. - Type III: An articular surface focal depression without a corresponding split.
The articular surface of the tibial plateau is depressed and forced into the lateral tibial metaphysis by axial forces in this instance, which is a pure compression fracture of the lateral or central tibial plateau. These fractures, which are low-energy injuries, are more common in people with osteoporotic bone abnormalities and in their fourth and fifth decades of life. They are really uncommon. able could be separated into two further subtypes: IIIA Contraction lateral tibial plateau fracture and IIIB Condensation fracture of the tibial plateau in the middle could lead to instability in the joints. - Type IV: Medial tibial plateau fracture, possibly including the tibial spines and accompanied by soft tissue damage; may or may not have a depression.
This fracture is a split or depressed medial tibial plateau fracture. It typically results from an accident with significant energy and involves axial stress at the knee combined with a varus force. make for 10% of all fractures of the tibial plateau. The prognosis is poorer since there is a greater chance of harming the popliteal artery and peroneal nerve. include fibular dislocation/fracture, posterolateral corner, and distraction injuries to the lateral collateral ligament. - Type V: Bicondylar tibial plateau fracture
consists of a split tibial plateau fracture, both medially and laterally. Usually, a high-energy injury causing complicated varus and valgus forces to act on the tibial plateau is the cause. may involve collateral ligament and anterior cruciate ligament damage. Constitute 3% of the tibial plateau. - Type VI: Fractures of the tibial plateau with discontinuities in the diaphysis
The primary characteristic of this kind of fracture is a transverse subcondylar fracture in which the metaphysis and diaphysis separate. All kinds of fractures can happen, and the condyles have diverse fracture patterns. Varus and valgus forces are two parts of the intricate mechanism underlying this high-energy injury. There is a chance of compartment syndrome and significant soft tissue damage in up to 33% of these open fractures. accounts for 20% of all fractures of the tibial plateau.
Diagnosis and Examination
- To evaluate these injuries, a physical examination is essential. Breaking this bone might cause injuries to nearby vital blood arteries and nerves. When a blood vessel injury is diagnosed, immediate surgery is necessary. To do surgery, the doctor will check for any open wounds surrounding the injury. The bone frequently tries to protrude from the skin or “tent.” If this isn’t fixed, the skin may eventually break off from the bone or die.
- Individuals who suffer from fractures of the tibia plateau are susceptible to compartment syndrome, a dangerous illness. This happens when blood and oxygen cannot flow freely through the leg due to excessive pressure. If this is left untreated, the muscle will eventually die. This syndrome manifests as excruciating pain when the big toe is stretched, loss of feeling in the foot, or agony that is excessive for the damage. There is an urgent surgical need. Even though you already have a broken bone, these tests may feel like your doctor is torturing you, but they are crucial.
Treatment of Fracture of the Lateral Tibial Plateau
Non-Surgical Treatment
- Surgery is not necessary for the bone to recover in some fracture patterns and types. Often, little fractures or those with good general alignment can be fixed without surgery. Adults with weak or persistently affected skin, those who are less active, and those in poor general health are also advised to pursue nonsurgical treatment. Depending on the type of fracture and the patient’s characteristics, knee immobilizers, hinged knee braces, and casts are all utilized to treat these injuries.
- To make sure that the fracture heals properly and maintains its proper position, regular follow-up care including physical examinations and x-rays is crucial if non-operative care is selected. Reducing or stopping smoking and maintaining strict blood sugar control are crucial for the recovery process if you have diabetes. Failure to follow physician instructions for early walking, bracing, or casting might result in bone movement that necessitates surgery.
- Without surgery, this bone may take three to four months to mend, depending on health and the nature of the lesion. Around six weeks after the bone has sufficiently healed to avoid displacement with motion, physical treatment is initiated to improve the knee’s range of motion.
Surgical Treatment
- If the fractured tibia is unstable owing to the type of fracture, the skin is at risk of dying, the pieces are misaligned, or the surgeon may advise surgery to correct it.
- Usually, a major incision is made and metal plates and screws are inserted to treat the injury. What kinds of incisions are needed, as well as the quantity of plates and screws, depend mostly on the type of fracture. To support the joint surface, bone grafts or certain forms of bone cement may be required. Injured tendons and meniscus are also treated with these procedures.
- Typically, surgery takes one to two hours. Following these kinds of surgeries, the majority of patients are admitted for the night to monitor any development of breathing issues or development of compartment syndrome.
Some patients require external fixation before ultimate surgical treatment in circumstances where there is severe injury to the muscles, nerves, or arteries, or if there is extensive contamination from dirt, rocks, or grass from the injury. - During this procedure, tiny incisions are made in the bone to insert metal pins, which are then attached to bars to provide some stability. The external fixator can be taken out and plates and screws inserted after follow-up procedures to clean the incision or heal skin damage.
- Surgeons like to carry out this procedure as soon as possible after the accident, preferably within a week or two. As a result, if patients would want more information or input from a surgeon, they have time to get a second opinion regarding their course of treatment.
It’s critical to select your surgeon carefully. Having a lot of surgical expertise will help you prevent difficulties and get the best outcome. - Altogether, the orthopedic surgeons at ROC have done more procedures for tibial plateau fractures than any other practice in Northern Nevada, and they are proud of their exceptional surgical outcomes.
- Patients are frequently placed in a hinged brace or knee immobilizer following surgery. They are not able to support weight right away. During the first six weeks, patients will require the use of a walker or crutches. To avoid stiffness, the knee should be moved gently from an early age. If the patient still has stiffness in their knees or ankles six weeks following surgery, physical therapy is started and the range of motion is gradually extended. Following this, your physician can choose to start you on a blood thinner.
Surgical Complications
- No matter how little the procedure, complications can still arise. An infection is always a possibility. Larger and more infected traumatic wounds provide a far higher risk. As little of this danger as feasible can be achieved by administering an antibiotic dose before surgery. There is always a chance of nerve or blood vessel damage. Having a skilled surgeon involved in your care lowers this.
- As previously mentioned, compartment syndrome can develop after an injury and change after surgery. To relieve the pressure on the muscles, more surgery is necessary. Falling, excessive mobility and noncompliance with weight-bearing restrictions can cause the fracture to separate or the metal to pull out of the bone. There’s always a chance that the bone might not mend, necessitating another surgery.
- This is typically linked to diabetes, patient noncompliance, or nicotine use, including smoking and chewing tobacco.
Physical Therapy Treatment
- After a fracture, physical therapy could be required to facilitate a quick recovery to maximum function. To reduce the risk of chronic pain following surgery, it is critical to consider the patient’s goals and mental state
- Managing tibial plateau fractures is a well-known challenge, especially in cases where there is a medial or posteromedial component. The goal of tibial plateau fracture treatment is to achieve stable osteosynthesis and anatomical reduction of the joint surface to allow for early mobilization and avoid general post-operative complications like pulmonary embolism or deep vein thrombosis as well as complications like joint stiffness. The physical treatment program seems to be non-standardized concerning the duration of non-weight bearing (NWB), and it varies according to the surgeon’s discretion.
Non-Weight Bearing STAGE (NWB)
- Depending on the severity of the trauma, this period can last anywhere between four and eight weeks. frequently rendered immobile in a fully extended “Genu-range” brace or cricket pad splint.
- Depending on the surgeon’s advice, static quadriceps and passive knee ROM can now be initiated. A mechanism for continuous passive movement can be employed.
- Give analgesia and decrease swelling priority.
- Exercises for residual joint ROM, such as ankle and hip.
Partial Weight Bearing Stage
- Depending on the degree of pain, gradually increase weight bearing on the operated leg to reach full weight bearing by 12 weeks.
- Exercises for active range of motion in the knee
- Closed kinetic chain Exercises
- Make sure your weight-bearing progression follows appropriate movement patterns.
- fundamental blueprint for strengthening
- Hydrotherapy (where necessary)
Full Weight Bearing Stage
- restoring the normal gait pattern
- Emphasis on functional activities, such as standing and sitting
- Exercises for proprioception
- Go back to your regular everyday routines.
High Level
- Advanced exercises for proprioception
- Sport-specific drills
- Advanced workouts for strengthening the lower limbs
- Given the increased risk of knee osteoarthritis after tibial plateau fracture, strengthening activities have to be promoted in long-term care.
Outcomes
- Fractured tibial plateaus are not common. Although low-energy trauma (such as a slip and fall) can also result in these fractures, high-energy trauma is usually the cause.
Physical therapy is crucial, although it varies depending on the fracture’s origin and the patient. Oedema, pain, loss of range of motion, strength, and function will be the initial presentation.
Early range of motion and mobility following surgery is crucial. Management of ROM, swelling, and discomfort is necessary during the sub-acute phases; however, this will vary according to the surgeon’s instructions. Strength, proprioception, and returning function to normal are critical in the later stages. - The majority of patients who suffer these kinds of fractures recover rather well and resume their previous activities. Patients are very comfortable by week six. It takes approximately four months to fully release them to activities like manual labor, skiing, and motocross. An overly aggressive return to work too soon may cause nonunion, hardware breakage, or refracture. Uneven healing of fractures can result in post-traumatic arthritis and the eventual need for a knee replacement.
FAQ
What is the healing time for a fractured tibia plateau?
Without surgery, non-displaced tibial plateau fractures can heal in as long as three to four months. In circumstances like these, healing takes about four months when surgery is necessary.
How dangerous is a fracture of the tibial plateau?
Fractures of the tibial plateau have an impact on the alignment, stability, and mobility of the knee. Because of the structures on the upper surface of the bone that are essential to the knee’s operation, fractures to the tibial plateau are therefore regarded as quite dangerous.
When you have a tibial plateau fracture, how do you sleep?
When you have a tibial plateau fracture, how do you sleep?
What is the quality of life after a tibial plateau fracture?
Altogether, the tibial plateau fracture of type Moore V represents a serious injury; the patient’s quality of life is considered to be 44% of their original value after an average of 5 years after considering all parameters.
References
- Tibial Plateau Fractures. (n.d.). Physiopedia. https://www.physio-pedia.com/Tibial_Plateau_Fractures
- Tibial Plateau Fracture | Diagnosis & Treatments | Reno Orthopedic Center. (2022, July 6). Reno Orthopedic Center. https://www.renoortho.com/specialties/center-for-fracture-trauma/tibial-plateau-fracture/