Intercostal Neuralgia
What is Intercostal Neuralgia?
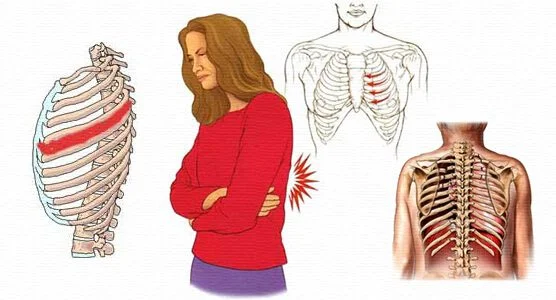
Intercostal neuralgia is a disease in which a person experiences neuropathic pain in the region corresponding to the intercostal nerves. These nerves radiate throughout a patient’s rib cage and abdomen.
Neuropathic pain happens when a person experiences pain because their somatosensory nerves have been upset or become extremely sensitive. The somatosensory nervous system is responsible for sending details about bodily sensations and changes to the brain. Intercostal neuralgia is also called chest wall pain.
Etiology
Thoracic pain is relatively infrequent and is only seen in a calculated 3-22% of persons guided to pain clinics. The majority of thoracic pain in the general residents is approximately 15%.
Chronic post-thoracotomy and post-thoracoscopy pain have a majority of 40%, and half of these patients are neuropathic. Intercostal neuralgia is the most periodic form.
What are the symptoms of Intercostal Neuralgia?
The major symptom of intercostal neuralgia is a sharp, burning, or shooting ache. This ache may be felt:
around the ribs
in the upper chest
in the upper back
Further symptoms in these regions contain:
- a squeezing stress sensation that covers the chest from front to back
- tingling
- numbness
- The pain might feel worse even when doing mild physical exercises, like deep breathing or stretching. It might also intensify when you cough, laugh or sneeze. Some person also notices referred ache in their shoulder edge or lower pelvis. Referred pain is pain that you sense in a location other than the involved one.
Intercostal neuralgia induced by the shingles virus (postherpetic neuralgia) can also cause your skin itchy and too sensitive, even to clothing.
Symptoms of more extreme cases of intercostal neuralgia contain:
- involuntary muscle twitching
- loss of appetite
- paralysis
- muscle atrophy
- ache that feels like a lightning bolt
What are the causes of Intercostal Neuralgia?
Intercostal neuralgia is induced by inflammation, irritation, or compression of your intercostal nerves, which are slightly below your ribs.
Several things can cause this, involving:
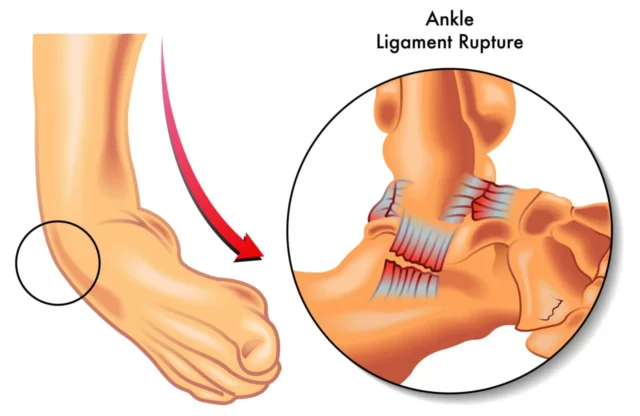
- trauma to your chest
- viral infections, like shingles
- nerve entrapment or pressure
- injury from a surgical process that includes opening your chest to access your lungs, throat, heart, or diaphragm (thoracotomy)
- Periodically, intercostal neuralgia doesn’t have a clear cause. This issue is known as idiopathic intercostal neuralgia.
What are the risk factors for intercostal neuralgia?
Several factors raise your risk of developing intercostal neuralgia. Risk factors contain:
Infection with varicella-zoster virus, the virus that induces chickenpox and shingles
Participation in sports that include high speeds or contact with other athletes, like snowboarding, skiing, football, wrestling, and rugby
Dangerous driving and motor vehicle accidents may cause damage to the ribs and the intercostal nerves
Decreasing your risk of intercostal neuralgia
These fit lifestyle practices may assist to control intercostal neuralgia and the damages that may cause it:
- Driving motor vehicles safely
- Obtaining vaccinated with the chickenpox vaccine
- Obtaining vaccinated with the herpes zoster or shingles vaccine if you are 60 years of age or more aged
- Wearing a seat strap when moving or riding in any type of motor vehicle
- Wearing proper defensive sports kits, like helmets and padding
How is it diagnosed?
Physical Examination
Comprehensive general physical and neurological investigations are always shown in thoracic pain, especially when dorsal column diseases are present. The sharpness of the thorax and stomach should also be studied. Loss of sensitivity means whether or not the ache is neuropathic.
Analysis of the thoracic spine is preferably conducted with the person in a sitting position and includes an assessment at rest and palpation of the vertebra and paravertebral structures, like the costovertebral joints or junctions.
Stimulation of pain by acting passive rotations, backward flexion, forward flexion, and lateral flexions in an individual, can show that the pain has a spinal etiology.
In upper thoracic and median and paramedian unilateral aches, the shoulder role on the same side should also be studied.
Stress pain in the sternum, sternocostal, and costovertebral junctions or joints is generally accompanied by a local ache way (eg, Tietze syndrome), but is periodically associated with segmental pain.
Stress pain of the rib(s) can show which thoracic level(s) is affected. Segmental translation of the thoracic vertebra (Federung test) in the prone position can show the level of the involved segment.
Other examination
Before analyzing your intercostal neuralgia, your doctor or physician will want to rule out any further causes of your ache. During a physical examination, they’ll probably push the site between your ribs or ask you to bring a deep breath. If either of these causes aches, you may have intercostal neuralgia.
Relying on your symptoms, you might also require a neurological examination to study for any issues with your nervous system. Your doctor or physician might also use an X-ray, CT scan, ultrasound, or MRI scan to examine for any signs of damage.
Testing may contain:
Exercise stress testing: Sometimes known as a treadmill test, this test assists your healthcare provider or doctor figure out how much the heart can handle with work. As the body functions more difficult, it requires more oxygen so it must pump more additional blood. The stress test can indicate if the blood supply to the arteries helping the heart is decreased.
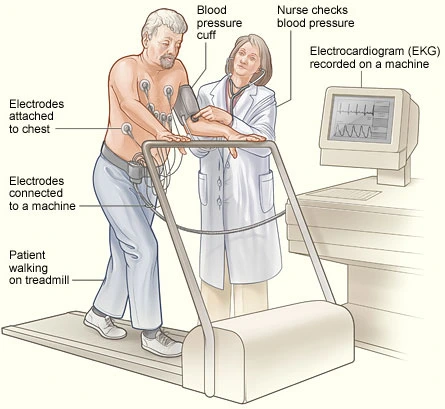
Electrocardiogram: An electrocardiogram is an easy, painless test that calculates the electrical movement of the heart.
Echocardiography: This examination uses sound waves to create live pictures of the heart to permit your healthcare provider or doctor to figure out how your heart and its valves are working.
Bloodwork: Measures levels of specific cardiac enzymes. If cardiac enzymes are raised, this may show an issue with the heart.
How is Intercostal Neuralgia treated?
There are numerous choices for reducing intercostal neuralgia, and many people discover that a variety of therapies functions best.
Over-the-counter pain reliever options
Some over-the-counter topical therapies can supply temporary pain ease. These contain:
capsaicin creams or skin patches
lidocaine gels or skin patches
Medication
Antidepressants are occasionally used to manage nerve-related pain. Common ones contain:
- amitriptyline
- desipramine (Norpramin)
- duloxetine (Cymbalta)
- imipramine (Tofranil)
- nortriptyline (Aventyl, Pamelor)
- venlafaxine
Your doctor or physician might also have you try an anticonvulsant drug, like:
- carbamazepine (Carbatrol, Equetro, Epitol,Tegretol)
- gabapentin (Neurontin, Gralise, Horizant)
- oxcarbazepine (Trileptal,Oxtellar)
- pregabalin (Lyrica)
- In extreme cases, your doctor or physician may specify an opioid-aspirin or opioid-acetaminophen to assist with the ache. These are all powerful drugs with many side impacts, so they’re generally a last-resort choice.
Complementary treatments
Some complementary treatments may benefit some people to nicely deal with intercostal neuralgia. These treatments, periodically guided as alternative treatments, are used in conjunction with conventional medical therapies. Complementary therapies are not told to replace full medical care.
Complementary treatments may contain:
- Acupuncture
- Massage therapy
- Yoga
Physiotherapy treatment
Hot and cold therapy
Cold therapy can assist to reduce your pain and decrease inflammation of the muscle. Use a cold pack to the injured site for 20 minutes at a time, several periods a day for the first two days. You can use a gel cold pack, an ice bag, a plastic bag loaded with ice and covered in a towel, or even a pack of frozen veggies.
After the first 48 hours, you may want to begin using heat on the damaged ribs. Heat can assist to relax and soothe the muscles so you can do your physical treatment. You can use heat for 20 minutes at a time with a heating pad or a warm wet towel.
Epsom salt soaks
As a portion of your heat treatment, you may like to bring a warm bath with magnesium sulfate (Epsom salts) added. You can see Epsom salts at your local drug shop or online at Amazon.com. Just add about 2 cups to your bath, and absorb for 15 or more minutes.
The liquefied minerals soak through your skin and may barely raise your blood levels of magnesium. Magnesium is an essential mineral for muscle role. Although the small quantity of magnesium soaked from your bath is unlikely to do anything to assist your strained muscles, the hot bath can assist you in rest.
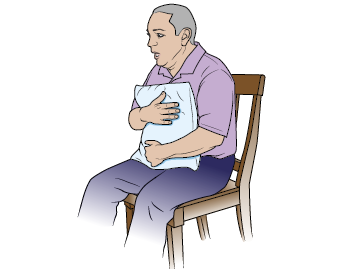
Breathing exercises
Breathing with an intercostal muscle strain is hurting. But assuming only shallow breaths rather than full, deep breaths can conduct to infection and pneumonia. Deep breathing activities can also be a form of meditation to decrease tension.
Attempt to do a few minutes of breathing activities every hour. For instance:
Keep a cushion against your damaged muscles.
You can breathe slowly and as deeply as you can.
Maintain the breath for a few seconds.
Breathe out gradually.
Recount 10 times.
Once you see your doctor or physician, they may send you home with a spirometer, a plastic device that offers you a visible clue to how greatly you should breathe.
Stretches
Several stretches can also decrease intercostal neuralgia aches:
- Stand with arms at the sides and elbows joint flexed at a 90-degree angle. carry arms backward while carrying shoulder edges together. Maintain for 10 seconds. reprise.
- Stand erect with your spine straight, and breathe as intensely as possible. Recount five times.
- Sit or stand with arms directly over the head, and hold hands together. Maintain elbow joints locked. Flex to one side and maintain for 10 seconds. Rest, and then reprise on the further side.
Lifestyle modifications
Specific lifestyle modifications can decrease nerve aches, involving aches caused by intercostal neuralgia:
- Exercising discharges endorphins which naturally decrease aches. Routine exercise also enhances blood flow and grows blood vessels which can assist nourish and recover broken nerves.
- Practicing good sleep hygiene assists to decrease pain. Nerve pain may get intense at night, so good sleep patterns are required to assist the body get as much downtime as possible. Moving to bed and waking up at the exact time per day and restricting caffeine input are useful patterns to enhance sleep and decrease pain.
- Restricting alcohol use is not only useful for overall fitness, but it also is good for ache decrease. Extreme alcohol use can hurt the nerves and worsen the pain. Some professionals recommend no more than four drinks per week.
- Practicing meditation can decrease both tension and ache levels. Suggested imagery and biofeedback may also be useful.
What are the potential complications of intercostal neuralgia?
The difficulties of untreated or inadequately managed intercostal neuralgia vary depending on the underlying condition, disorder, or disease. Any type of rib cage region pain, whether it happens alone or is attended by other symptoms, should be considered by your doctor or healthcare provider, or physician. Once the underlying cause is determined, following the therapy plan you and your healthcare provider or doctor develop especially for you will minimize the risk of difficulties of intercostal neuralgia and its underlying cause. These complications contain:
- Chronic chest pain, rib pain, weakness, or stiffness
- Low oxygen levels
- Permanent immobility and reduced range of movement in the trunk or shoulders
- Pneumonia
- Post-herpetic neuralgia
- Respiratory failure and respiratory arrest
- Spread of cancer
How to Prevent Intercostal Neuralgia?
Because intercostal neuralgia has so many possible causes, prevention can be hard.
When the cause of intercostal neuralgia might be thoracotomy, the most useful preventive approach is to decrease the risk by controlling the infection of the wound. This contains using the proper anesthetics.
When it arrives to intercostal neuralgia due to shingles, the most useful preventive approach is to minimize the risk of acquiring this infection in the first position.
For instance, someone should obtain the shingles vaccine, which a study suggests decreases the chance of shingles by 51%. The shingles vaccine also decreases the risk of aches from shingles by 66%.
FAQ
What do I need to know about intercostal neuralgia?
Intercostal neuralgia contains any painful disease of the intercostal nerves. There is a combination of causes of intercostal neuralgia which cause significant chest, rib, and/or upper abdominal wall aches.
What does intercostal neuralgia feel like?
Symptoms generally contain pain that is dull and constant. The ache also may be defined as stabbing, sharp, tearing, tender, spasmodic, aching, or gnawing. Many persons say feeling as though the pain has covered their upper chest like a strap.
Does intercostal neuralgia come and go?
Most instances of intercostal neuralgia are periodical, meaning the ache arrives and runs. Some persons define it as an aching or gnawing feeling, while others experience sharp aches and spasms, and others yet represent an extreme burning feeling or simply a tender and discolored sensation in the region.
Is intercostal neuralgia life-threatening?
Gentle and short-term intercostal neuralgia In this issue, intercostal neuralgia mostly arrives from trauma, motion weight, or poor posture. Thus, the condition does not pose a threat to the person’s health. Nevertheless, the ache can make it hard for people to work, walk, and live.
Does exercise help intercostal neuralgia?
Several stretches can also decrease intercostal neuralgia aches: Stand with arms at the sides and elbow joints flexed at a 90-degree angle; carry arms backward while carrying shoulder edges together. Maintain for 10 seconds; reprise. Stand erect with your spine straight, and breathe as greatly as possible.