Foot Pain
What is Foot Pain?
Foot pain is a common and often debilitating condition that can affect individuals of all ages and lifestyles. The human foot is a complex structure comprised of numerous bones, joints, muscles, tendons, and ligaments, all working in harmony to support our weight, enable movement, and maintain balance. When any part of this intricate system is compromised or experiences injury, it can result in varying degrees of discomfort, pain, and reduced mobility.
This introduction provides a glimpse into the world of foot pain, a condition that can arise from a multitude of causes, including injuries, medical conditions, or lifestyle factors. Understanding the underlying causes, symptoms, and available treatments for foot pain is essential for those seeking relief and improved quality of life.
Foot pain is the term used to describe any soreness or discomfort in one or more foot areas, including the following.
- Soles
- Heels
- Arches
- Toes
Anatomy of the foot
In order to provide stability, balance, and mobility, each foot’s 26 bones, 30 joints, and more than 100 muscles, tendons, and ligaments collaborate.
Here are the main components of the feet.
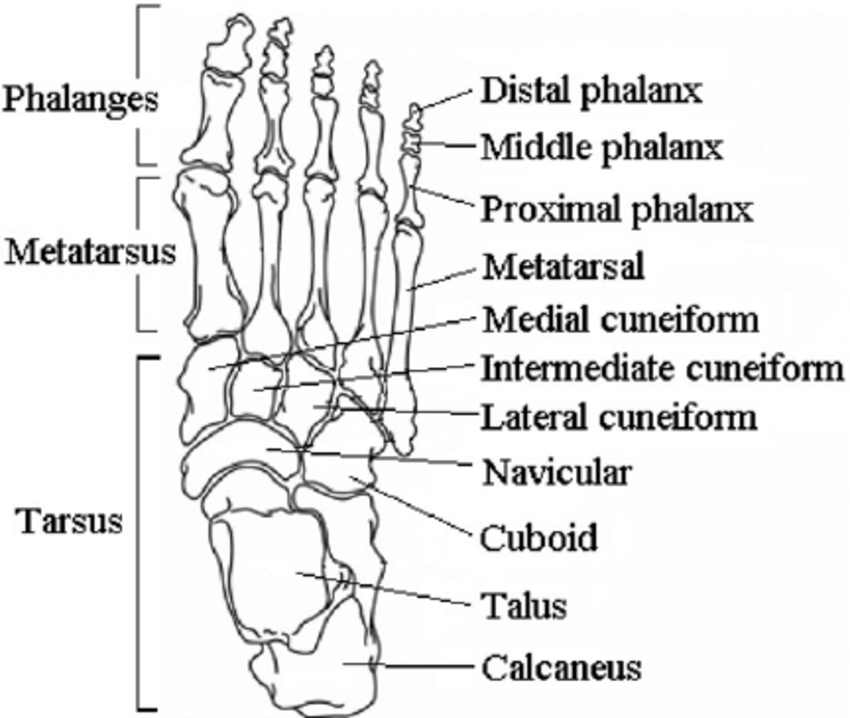
Bones of the foot
The foot is made up of 26 bones, including the tarsal (number 7), the metatarsal (number 5), and the phalanges (14) which are anatomical structures below the ankle joint.
- Talus bone: a junction between the top of the foot and the tibia and fibula, the two lower leg bones.
- Calcaneus: the largest foot bone, which forms the heel bone and is located below the talus.
- Tarsals: The foot’s arch is made up of the tarsals. In order to support weight and maintain foot stability, the arch is crucial.The cuboid, navicular, medial, intermediate, and lateral cuneiform are the tarsal bones.
- Metatarsals: The forefoot is composed of five bones, which are numbered one through five and begin with the big toe. It provides stability to the forefoot.
- Phalanges: the fourteen bones that comprise each toe. The big toe is made up of the proximal and distal phalanges. There are three on the other toes.
- Sesamoids: two tiny, pea-shaped bones that are located in the foot’s ball beneath the first metatarsal head. Its function is to support and lessen the strain on the tendon.
Joints
This two or more of these bones contact, a joint is created in the foot. Each toe has three joints, with the exception of the big toe these include.
- Metatarsophalangeal joint (MCP): The toe’s base joint is called the metatarsophalangeal joint (MCP).
- Proximal interphalangeal joint (PIP): The joint in the middle of the toe is called the proximal interphalangeal joint (PIP).
- Distal phalangeal joint (DP): The joint closest to the tip of the toe is called the distal phalangeal joint (DP).
There are two joints on each big toe:
- Metatarsophalangeal joint: Junction between the metatarsophalangeal
- Interphalangeal joint: Junction between the phalanges
Cartilage
A layer of cartilage covers the surfaces of the bones where they come together to form joints, allowing the bones to move in harmony with one another.
A fibrous capsule surrounds the joints and is lined by a thin membrane known as the synovium, which secretes a lubricant to keep the joints lubricated, is known as the synovium.
Muscles
The foot’s form, stability, and mobility are provided by muscles. The following are the primary foot muscles.
- Tibilias posterior: the foot’s arch-supporting.
- Tibilias anterior: which enables upward movement of the foot.
- Tibilias peroneal: the muscle that regulates ankle lateral movement.
- Extensors: which aid in lifting the toes and enable stepping.
- Flexors: which is stabilizing the toes.
Tendons and ligaments
In order to maintain the foot’s arch, many tendons join these muscles to the bones and ligaments that hold the bones together.
The Achilles tendon, which extends from the calf muscle to the heel, is the primary tendon of the foot. The Achilles tendon enables activities including running, jumping, stair climbing, and toe-standing.
Following are the foot’s primary ligaments:
- Plantar fascia: The foot’s longest ligament that goes from the heel to the toes on the bottom of the foot creates the arch. The plantar fascia gives the foot strength for walking and aids in balance by stretching and contracting.
- Plantar calcaneonavicular ligament: a ligament that supports the head of the talus and joins the calcaneus and navicular bones in the sole of the foot.
- Calcaneocuboid ligament: The ligament that aids in the plantar fascia’s ability to support the foot’s arch by joining the calcaneus and tarsal bones.
Cause of the Foot Pain
Foot pain can be caused due to certain lifestyle preferences or a medical condition.
Lifestyle choices:
- Foot pain is often caused by wearing the wrong-fitting shoes. Because they put plenty of stress on the toes, wearing high heels can often result in foot aches.
- Damages sustained while participating in high-impact sports or workouts, such as jogging or vigorous aerobics, can even result in foot pain.
Common medical causes
Numerous medical conditions are directly connected to foot discomfort.
- Arthritis: Your feet are specifically prone to the pain that arthritis causes.
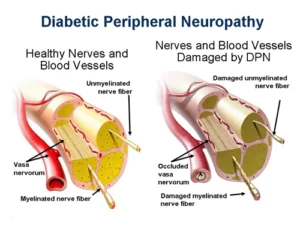
- Diabetes mellitus can lead to issues and a numeral of foot diseases. Foot pain is more typical in those who have diabetes.
- Nerve injury in the foot.
- Foot ulcers/sores
- Clogged/solidified arteries in the legs and feet.
You run a higher risk of developing foot pain if you have:
- Overweight/obesity
- Pregnancy
- A foot injury like a fracture, sprain, or tendinitis.
Foot pain may also result from the following different factors:
- Corns
- Calluses
- Bunions
- Warts
- Ingrown toenails
- Medicines that induce swelling of the feet.
- Morton’s neuroma is thickening around the nerve tissue between the toes near the ball of the foot.
- Hammer toes
- Athlete’s foot
- Haglund’s deformation( which is a growth of the back of the heel bone)
- Peripheral arterial disorder (PAD)
- Fallen arches
- Plantar fasciitis
- Gout (mainly involving the big toe around the ball of the foot)
Common condition of Foot Pain and treatment
Arch pain
Plantar fasciitis
This is the most typical reason for arch pain. Plantar fasciitis can impact the heel, arch, or both.
The heel of the foot encounters severe pain when the patient stands up after lying down, which is a sign of plantar fasciitis. The inflammation of the fascia, a strong, fibrous band of tissue that connects the heel bone to the base of the toes, is caused by overuse damage to the sole (plantar) of the foot.
Women, those who are overweight, those whose jobs demand a lot of walking or standing on hard surfaces, those who have flat feet, and those with high arches are more likely to develop plantar fasciitis. Running or walking, especially when the calf muscles are tight, may also aggravate the disease.
Treatment
- Rest
- Uses of ice packs
- NSAIDs are non-steroidal anti-inflammatory drugs.
- Ultrasound
- Plantar fascia and Achilles tendons stretching exercises
Fallen arches/ Flat feet
Happens when the arches of the feet flatten out (usually when standing or walking), generating foot pain and other problems.
treatment
- shoe inserts or shoe adjustments
- Rest
- Ice
- Walking rod or brace
- Physical therapy
- Surgery
Toe Pain
Pain in the toes might be a symptom of gout, an arthritic condition. Crystals accumulate in toe joints, inducing intense pain and swelling. The big toe is often affected.
treatment
- Rest the foot.
- Ice the area.
- Medication such as a nonsteroidal anti-inflammatory medicine (NSAID), prednisone, colchicine, or allopurinol.
- Avoid foods that can cause gout worse.
Achilles tendon injury
The Achilles tendon is the body’s largest tendon. It ties the heel bone and the calf muscle together. However, this tendon is even the most vulnerable to rupture or tendonitis, an inflammation of the tendon brought on by overuse.
Overusing the calf muscles and Achilles tendon can result in tendonitis. minor swelling, stiffness that goes away as the tendon warms up, and minor post-exercise soreness that becomes worse with time are all potential indications.
Treatment
- NSAIDs are non-steroidal anti-inflammatory drugs
- Bandages and bracing for muscle and tendon stretching
- Massage
- Strengthening training
- Ultrasound
- Surgery
Ankle Sprain
An ankle sprain is damage to the foot’s ligaments in the ankle. Ligaments, which link and stabilize the bones, are elastic, fibrous bands of tissue. A common, painful ailment called an ankle sprain happens when one or more ankle ligaments are strained beyond their usual range of motion. Sudden twisting, turning, or rolling motions can result in sprains. Depending on how badly the ligaments are strained or torn, a sprain can present with different symptoms, but the most common ones are swelling, discomfort, and bruising.
Treatment
Treatment will rely on the severity of the sprain, Which includes:
- Resting the ankle
- Covering the ankle with an elastic bandage or tape
- Ice pack application (to decrease inflammation)
- Elevating the ankle
- Nonsteroidal anti-inflammatory medications, such as ibuprofen to help relieve the ache and inflammation.
- Gradual return to walking and exercise
- A walking cast (for moderate sprains)
- Surgery (for severe sprains)
- Physical therapy
Heel spur
Foot discomfort might also come from heel spurs. On the base of your heel, there are some unusual bone growths. They might be acquired through wearing the incorrect footwear, from having an odd gait or posture, or even from engaging in sports like jogging. While you’re standing or walking, the spurs could pain. Many people have them, yet the majority do not experience pain. Heel spurs are more prone to develop in those who have flat feet or high arches.
Treatment
- Take a footrest.
- Stretch the muscles in your feet’s heels.
- Take painkillers.
- Apply ice or cold packs to the bottom of your foot and the heel.
- Put on shoes with a cushioned sole and strong arch support.
- Put on a heel pad with cutouts.
- Use an orthotic, which is a custom-made shoe insert.
- Give physical therapy a try.
- Ask your doctor about medical procedures if you’re still in discomfort.
Stone bruise
A severe bruise on the fat pad of the heel or ball of the foot is referred to as a stone bruise. It can also occur after stepping on a hard item, however, it frequently results from an impact injury. You experience agony similar to walking on pebbles. Over time, it will naturally disappear.
Treatment
- Relax your foot.
- Ice the site.
- Take over-the-counter ache relievers.
Heel Fracture
A heel fracture is frequently a severe injury brought on by a fall or auto accident. Not only might your heel bone break, but it could also fracture. The major symptoms are heel discomfort, bruising, swelling, or difficulty walking.
Treatment
- Avoid applying pressure on the heel. Crutches are an option.
- Use cushions to shield the heel.
- Put on a cast or splint to protect your heel bone.
- The-counter painkillers.
- Give physical therapy a try.
- Consult with your doctor regarding surgery if you’re still in discomfort.
Metatarsalgia
Your foot’s ball feels painful and swollen. Ill-fitting shoes are the usual cause. However, physically demanding activities like sprinting or jumping could cause it. Additionally, it is sometimes referred to as a stone bruise.
Treatment
- Utilize painkillers.
- Ice and rest your foot.
- Wear comfortable footwear.
- Shoe inserts to relieve stress on the ball of your foot.
Morton’s neuroma
Morton’s neuroma induces a thickening of the tissue near the nerves between the bases of the toes (usually between the third and fourth toes). Over the ball of your foot, you frequently experience discomfort, strange feelings, or numbness. It is more prevalent in women. Wearing high heels or narrow shoes may be the cause.
Treatment
- Wear shoe inserts to relieve stress on the nerve.
- Gain a steroid or other injection into the foot.
- Utilize painkillers.
- Do not wear narrow-toe box shoes or high heels.
- Don’t do anything that would put a strain on the neuroma.
- Consult your physician about surgery.
Sesamoiditis
Two bones close to your big toe are solely joined by tendons. They are known as sesamoids. Sesamoiditis develops when the tendons that surround them are damaged and inflamed. It’s a type of tendinitis that ballet dancers and runners frequently experience.
Treatment
- Put your feet up.
- Ice the painful areas.
- Put on a pair of comfy shoes and a foot pad beneath the toe.
- To immobilize the joint and promote healing, tape the big toe.
- Put on flat shoes.
- Concerning steroid injections, see your doctor.
Bunion
A bony protrusion at the base of the big toe on the outside of the foot is known as a bunion. It is related to the first toe joint being out of place.
Anyone can acquire them, especially if they are sporting uncomfortable or ill-fitting footwear. A lot of people who have bunions also have hammertoes.
Treatment
- Consider using a shoe insert or switching to more comfortable footwear.
- A doctor might recommend surgery if you’re still in agony.
Hammertoes
A hammertoe is when your second, third, or fourth toe bends at the middle joint, creating a hammer-like appearance. It can be brought on by wearing uncomfortable shoes, but it can also result from a muscular imbalance.
Treatment
- Footwear with a broad, deep-toe bed.
- Stretching techniques for toe muscles.
- Surgery if still having problems.
Claw toe
When your toe cannot straighten out and points downward or upward, you have a claw toe. It frequently results from nerve damage brought on by conditions like diabetes or alcoholism, which cause the muscles in your foot to become weak.
Without special footwear to accommodate the claw toe, you may develop irritation and callus.
Treatment
- Change to better-fitting footwear. Avoid high heels and tight shoes.
- Stretching for your toes and toe joints.
- Try shoe inserts.
- Ask your doctor about surgery.
Hallux rigidus
Big toe arthritis, also known as hallux rigidus (stiff big toe), affects the base of the big toe.
Joint stiffness and discomfort are the symptoms, which get worse over time.
Treatment
- Stretching exercises and painkillers are possible treatments.
- Sometimes, surgery is required.
Corns /calluses
Corn is a thick collection of tough skin that forms on the foot or toe when there is irritation or pressure. They occasionally have horn-like appearances.
Calluses are wider areas of tough skin buildup on the toes or feet. They take place as a result of pressure or irritation. Poorly fitting shoes are typically the cause of calluses and corns.
Treatment
- Put on more comfortable shoes.
- To remove the additional skin, soak the foot and rub it with a pumice stone.
Sesamoid fracture
A Sesamoid fracture is a break in the small bones (sesamoids) that are embedded in tendons attached to the big toe. The main indication is pain in the big toe area.
Treatment
- Rest, ice, and elevate your foot.
- To reduce pressure, put on shoes or foot pads with hard soles.
- Take pain relievers.
- If the discomfort persists, speak with your doctor.
Pain on the Foot’s Outer Edge
One of the most often fractured bones in the foot is the fifth metatarsal, which forms the outside of the foot. Following an injury, symptoms include pain, bruising, and swelling along the outside edge of the foot.
Consult a physician and get an X-ray if you believe you may have broken a bone.
Treatment
- Take pain relievers.
- Rest, ice, and elevate your foot.
- Don’t walk on it.
- Ask your doctor if surgery is necessary.
- A cast may be necessary in various conditions.
Heart Disease
Heart disease and high blood pressure can even cause pain and other issues with your feet. When you have heart disease, your heart has a more difficult time moving blood to the rest of your body, particularly the more distant parts such as your feet. Circulation problems can also be caused by high blood pressure.
Heart disease or high blood pressure may induce the following foot-pain symptoms, Sores, Cramping, Pain, or fatigue in your feet, specifically when walking.
Heart disease is usually analyzed based on your symptoms and medical record diagnostic tests such as an EKG, a stress test, or computed tomographic angiography.
Treatment
- Foot pain brought on by heart disease or high blood pressure is typically managed by addressing the underlying cause.
- Lifestyle adjustments like weight loss, exercise, and giving up drinking or smoking can be beneficial.
- To assist in lowering your blood pressure or cholesterol, the doctor may even recommend drugs or dietary changes.
Diabetes
It is typical to experience foot issues when you have diabetes, particularly if your blood sugar isn’t well-managed. Some of the symptoms of diabetic foot problems include a tingling sensation in the foot, Failure of sensation or numbness, A burning or pricking sensation, A sensation of weakness in the foot, and Toes or feet that seem deformed.
Diabetic neuropathy is a type of nerve injury that can be caused by diabetes. This is what causes a lack of sensation in your feet as well as other symptoms.
When you have diabetes, you may also have decreased blood flow to your feet. Decreased blood flow can make it challenging for even small sores, cuts, or other injuries to heal.
Treatment
- Make certain that blood sugar is controlled.
- Make certain that feet are neat and dehydrated.
- Wear moisture-wicking socks and breathable, well-fitting shoes.
- Inform your healthcare provider if you see any cuts, sores, blisters, or further lesions on your feet.
- Don’t walk barefoot.
- Keep your feet elevated when sitting.
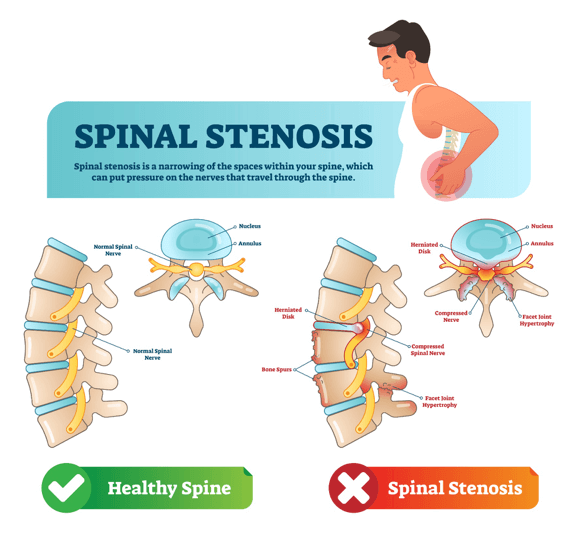
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome refers to the contraction of the posterior tibial nerve. This nerve passes through a space inside your ankle that’s named the tarsal tunnel.
With this syndrome, you may feel foot pain defined as burning, pricking, and numbing. Diabetes can result in diabetic neuropathy, a form of nerve damage. Your feet’s lack of feeling as well as other symptoms are brought on by this. The discomfort might occasionally radiate up to the calf or higher, and it usually gets worse at night.
Anything that puts stress on the posterior tibial nerve can induce tarsal tunnel syndrome. For instance, if you sprain your ankle, the ensuing swelling may aggravate or compress the nerve.
A bone spur, or abnormal bone growth, induced by ankle arthritis can lead to nerve constriction within the tarsal tunnel. This is also actual of other structural concerns with the foot, such as a varicose vein, or a swollen ankle tendon or joint.
Flat feet are also more prone to creating this syndrome.
Treatment
Non-surgical treatments are used to treat tarsal tunnel syndrome. They include:
- R.I.C.E. approach (rest, ice, compression of the nerve, elevation of the foot).
- NSAID such as Ibuprofen or Naproxen
- Steroid injection
- Wearing custom shoe inserts, specifically, if you have flat feet.
- Sporting a brace or cast to immobilize the foot.
- Surgery is considered if the nerve pain is extreme or if it doesn’t react to additional therapies.
Ingrown Toenails
An ingrown toenail happens when the edge of a toenail develops or is pressed into the skin because of pressure from a shoe, it usually is located at the edge of the big toe.
Even the smallest piece of ingrowing can hurt. Excluding pain, other symptoms of an ingrown toenail have red or swollen skin around the nail. The ingrown part of the nail is usually unrecognized because it is buried under the skin.
Some aspects that increase a person’s chance of having an ingrown toenail include Wearing poorly fitted shoes, Trimming the side edge of your toenail too short, and Having some sort of trauma to the toenail.
A physical exam simply examining the concerned toe is all that is required to diagnose an ingrown toenail.
Treatment
- Treatment of an ingrown toenail relies on its severity. For minimal to mild foot pain, redness, and no discharge, warm soaks and a small piece of cotton placed under the nail may be all that is required.
- You could require an antibiotic.
- The ingrown portion of the nail may also need to be removed.
Risk factors for Foot Pain
A risk factor is something that makes developing a medical condition a possibility. In elderly individuals and youngsters, foot discomfort is more common. The danger of wearing high heels may also be increased in women. Following are some typical risk factors linked to increased possibility of developing foot pain:
Certain jobs: Some occupations, such as construction, may increase the risk of harm. In the restaurant business, for example, repetitive work tasks may cause additional problems.
Sports: High-impact exercisers are more likely to develop stress fractures, plantar fasciitis, heel spurs, sesamoiditis, and Achilles tendinopathy.
Smoking: Healing is slowed by smoking. As a result of improper healing, this may result in painful foot issues.
certain health issues, including:
Diabetes: Due to poor circulation, diabetics are at risk for serious foot infections.
Obesity: Individuals who are overweight put additional strain on their feet. Injuries to the foot or ankle are also more likely as a result of obesity.
Medical conditions: Foot discomfort can also be a symptom of other medical conditions such as osteoarthritis, rheumatoid arthritis, gout, and other genetic disorders.
Diagnosis for Foot Pain
- The medical practitioner will physically and visually inspect the feet when they are at rest and while they are bearing weight and not.
In order to find any noticeable abnormalities, swelling, painful places, or variations in the foot and arch’s bones, the foot and arch will be touched, examined, and felt. - The foot’s muscles will be examined by the medical practitioner. patient can be required to hold or move your foot and ankle against resistance during these tests, as well as to stand, walk, or even run.
- The skin will be examined for any indications of bleeding, skin breaks, or infections.
To make sure there hasn’t been any damage to the nerves in the foot, a test will be done on them. - To evaluate the electrical activity of your muscles and nearby nerves, use electromyography.
- To find out whether there are any soft tissue or bone abnormalities, an X-ray, MRI, or bone scan of the foot and arch may be performed.
- To rule out systemic conditions such as diabetes, gout, or rheumatoid arthritis, a blood test may be required.
Treatment of Foot Pain
Your doctor will inquire comprehensively about your symptoms, the intensity and location of your pain, and your medical background in order to identify the cause of your foot pain and recommend a course of action. X-rays should be used in diagnosis.
The origin of your condition will determine the course of treatment.
Non-surgical treatments of Foot Pain
- Rest: Resting your foot is frequently the best course of action for healing if the pain in the foot has been brought on by an overuse injury like plantar fasciitis or Achilles tendonitis. Avoid strenuous activities like jogging or walking that strain your feet.
Ice: Putting ice on your foot might assist in easing pain and inflammation. Use ice multiple times each day for 20 minutes at a time. - Elevation: You can also aid in decreasing inflammation by raising your foot above the level of your heart. When you are seated or lying down, raise your foot on a pillow.
- Over-the-counter pain relievers: Painkillers available over the counter, such as ibuprofen or acetaminophen, can assist to lessen discomfort and inflammation. Make careful you adhere to the directions on the label.
- orthotics: Shoe inserts called orthotics can support your arches and better your foot alignment. This can aid in easing discomfort and minimizing future harm.
- Physiotherapy treatment: Physiotherapy can assist in enhancing the strength of your foot and ankle muscles and tendons. You may be able to move more freely and have less discomfort as a result.
Physiotherapy treatment for Foot Pain
- Strengthening and Stretching exercises
- Exercises to strengthen the ankle may have several advantages, like a reliable source
- By making the muscles around the ankles stronger, injuries can be avoided by putting less strain on the ankle joint.
- Exercises that focus on building strength can assist in enhancing bone density. Degenerative bone disorders like osteoarthritis are less likely to develop in those with higher bone density.
- Balance should be improved by strong ankle muscles. For a lot of sports and workouts, good balance is essential. Additionally, it will decrease the chance of injuries and falls.
- Performing stretches and exercises that may increase the ankles’ flexibility and strength.
- Calf lift
- The muscles in the legs and ankles will also be stretched by the calf raise.
- The steps to a calf lift are as follows
- Step up onto a platform that is just slightly elevated.
- While letting the heels hang off the rear, keep the balls of your feet planted firmly on the platform.
- With a toe lift, the heels will rise above the surface.
- Allow the heels to reappear just below the surface.
- Perform the stretch a few times.
- Towel stretch
- The muscles in the lower legs and ankles will be stretched by the towel stretch.
- The stages of a towel stretch are as follows:
- When you sit, extend your legs straight in front of you.
- Holding the towel at each end, wrap it around the top of the foot.
- Pull the towel gently so that the toes point back in the direction of the upper body.
- After 30 seconds of holding the position, release it for the next 30 seconds.
- Three times while performing the stretch, move to the other side.
- Towel curls
- The muscles in the feet and ankles are strengthened as well with towel curls.
- How to do towel curls
- When you sit, put your feet firmly on the ground.
- Put a cloth beneath one of the feet.
- To lift the towel off the floor, curl the toes inward to grasp it.
- Hold it there for just a short amount of time before releasing it.
- Replicate with the other foot.
- Toe pull
- The muscles in the legs and ankles are loosened by the toe pull.
- How to do a toe pull:
- Place one leg straight up off the floor while seated on a chair.
- Back toward the body, slowly point the toes.
- Hold the position for a little while.
- To return the leg to the ground, let go of the toes.
- One leg at a time, repeat many times.
- Standing heel raise
- Leg and ankle muscles stretch while standing on one’s heels.
- To carry out a heel rise while standing:
- Just wider than your shoulders, stand.
- Knees should be slightly bent and hands should be placed on the thighs.
- While maintaining the toes on the ground, raise one heel, then gradually bring it back down.
- For each heel, carry out this exercise multiple times.
- Roll a golf ball.
- The muscles in the feet and ankles are stretched during the golf ball roll.
- How to do a golf ball roll:
- Put a golf ball beneath one foot while seated in a chair. Any ball that is the same size will do.
- Spend a minute slowly rolling your foot over the ball.
- Use the opposite foot to perform the exercise again.
- Plantar fascia stretch
- Remember that finish this stretch slowly and steadily.
- Sitting in a chair, cross one leg over the other knee so that your ankle is on top of the other leg.
- With one hand holding your ankle and the other with your toes, pull your toes back until you feel a stretch at the bottom of your foot.
- Replace each foot three times after holding it in place for 20 seconds.
- Perform this workout once every day.
- Mobilization and manipulation
- Massage of the plantar fascia.
- Note: This workout shouldn’t cause you any pain. Use just enough force to feel a little stretch but not pain.
- Place one foot on a frozen water bottle while standing or sitting on a chair. A frozen water bottle is useful because the ice reduces inflammation.
- Under your foot move the water bottle slowly forward and backward. You should start just under the ball of your foot and end just before the heel.
- Ten times for each foot, softly roll the bottle back and forth. Make a couple for each foot.
- Perform this activity once every day.
- Foot massage
- To apply this method.
- One hand on either side should be holding the foot.
- your fingers should be on the top of your foot.
- put the thumbs on the toe pads of each foot.
- Using little pressure, run the thumbs down each toe.
- Continue the downward stroke motion with the thumbs as you go to the ball of the foot.
- Massage of the plantar fascia.
- Range of movement exercises
- Ankle Pump Ups and Down, eversion & inversion range of motion exercise helps in mobility and for good blood circulation, especially in heart conditions.
- Ultra Sound
- The use of ultrasound treatment in the management of heel pain has several potential advantages. Most significantly, the hollow needle’s focused sound waves break down painful adhesions and scar tissue on the plantar fascia and heel.
- To improve local circulation, ultrasound works by delivering vibrations to the region that is being treated. The vibrating waves then penetrate through to the deeper tissues and increase blood flow.
- Foot Orthoses
- Foot orthoses, also known as orthotics, are made-to-measure shoe inserts that support the feet and improve foot posture. If a person has ongoing foot or leg problems that influence the health and functionality of their feet, a therapist could advise orthoses.
- The three primary types of orthotics are soft, stiff, and semi-rigid. Soft orthotics are designed to offer additional comfort while the foot is on the ground. Semi-rigid orthotics, which are frequently used on flat feet, are made to offer stability and cushioning.
- Education on footwear and activity
- Proper footwear may provide protection, support, stability, comfort, and cushioning, all of which can help guard against conditions and issues with the feet such as grown toenails, tendonitis, blisters, and foot discomfort.
- For particular sporting activities, wearing the right athletic shoe may increase comfort and performance, and most importantly, avoid injury. Sports may put a lot of strain on the legs, ankles, and feet.
If your foot pain is severe or does not improve with non-surgical treatments, your doctor may recommend surgery.
Surgical treatment for Foot Pain
- Surgical treatment for foot pain is typically considered only after non-surgical treatments, such as rest, ice, compression, elevation, and physical therapy, have failed to provide adequate relief. Surgery may be recommended for a variety of foot conditions, including Plantar fasciitis, Bunion, Hammertoe, and Arthritis.
- The type of surgery that is performed will depend on the specific foot condition and the severity of the pain. Open surgery and endoscopic surgery are both options for doing surgery.
- Open surgery: Open surgery involves making an incision in the foot to access the affected area.
- Endoscopic surgery: Endoscopic surgery involves making a small incision and inserting a camera and surgical instruments to perform the procedure.
- Recovery from foot surgery can vary depending on the type of surgery that is performed. In general, patients can expect to wear a cast or boot for several weeks after surgery.
- Physical therapy may be recommended to help patients regain strength and range of motion in their feet.
- The risks of foot surgery include infection, bleeding, and nerve damage. However, these risks are generally low.
- If you are considering foot surgery, it is important to discuss the risks and benefits of the procedure with your doctor.
How to ease Foot Pain at home?
You may have a variety of at-home therapy options depending on the sort of pain you’re experiencing and its underlying cause. However, the following guidance could make you feel better:
- Apply ice to the damaged area.
- Take into consideration utilizing an over-the-counter (OTC) pain reliever.
- Use foot pads to prevent friction on the afflicted region.
- Elevating the painful foot is advised.
- Give your foot as much time as possible to relax.
When to consult your doctor?
Many persons who have foot pain on a regular basis are knowledgeable about the reasons for their pain and have found effective treatments. However, if any of the following are the case, you should see a doctor right away:
- You feel a sharp, unexpected pain.
- Your foot discomfort is a result of your most recent injury.
- After an injury, you are unable to put pressure on your foot.
- You have foot soreness as a result of a blood flow-related medical condition.
- The part that aches has an open wound.
- Your sore area can seem discolored or develop other inflammation-related symptoms.
- You additionally feel fever and have foot pain.
Prevention of chronic Foot Pain
When standing and walking, the foot is quite essential. It has to compensate for all structural weaknesses in the skeleton above.
A breakdown in the foot structure may occur if the foot is unable to properly adjust to structural defects in the body.
This foot collapse is the root cause of many chronic foot pains, including flat feet, heel spurs, bunions, plantar fasciitis, and many more. The following are typical preventative steps to reduce foot pain:
- Choose comfortable, roomy, and well-cushioned shoes.
- Avoid footwear with high heels and tight toe spaces.
- Maintain a healthy weight.
- Stretch before engaging in vigorous exercise.
- Sit down during breaks.
- Practice good foot hygiene.
- When you’re outside, you should always wear shoes to protect your feet.
- Stay hydrated.
Summary
Foot pain and mobility issues might result from tight or weak ankle muscles. These problems may also raise the possibility of damage to the ankle’s bones, tendons, and ligaments.
Increasing ankle joint mobility and lowering injury risk are both achieved by stretching and strengthening the ankle muscles. Additionally, increasing bone density may help lower the chance of developing degenerative bone illnesses.
People should try to include activities that strengthen the ankles in their normal exercise program. For more specific information and guidance, speak with a physician or physical therapist if you already have ankle issues.
FAQs
What is the main cause of foot pain?
Your feet may ache due to arthritis, a cracked or broken bone, gout, tendonitis, or plantar fasciitis, among other conditions. Foot issues are more prone to develop as you age and your joints deteriorate. Being overweight places additional strain on your feet, which can cause pain
How can foot discomfort be relieved?
Your symptoms may be relieved by rest, ice, or nonsteroidal anti-inflammatory drugs like ibuprofen and naproxen. Your feet’s bones might feel less pressure because of shoe inserts.
How can you tell whether your foot pain is severe?
If you Have extreme pain or swelling, particularly after an injury, get medical help right away.
have a bleeding or open wound.
Have infection-related symptoms, such as redness, warmth, or soreness in the afflicted region, or have a temperature of more than 100 F (37.8 C).
Unable to put weight on the feet or walk.
Can diabetes cause foot pain?
Diabetes patients frequently have foot issues. When the nerves and blood arteries in the foot are damaged by high blood sugar levels, they may eventually take action. Diabetic neuropathy is the term for nerve damage that can result in numbness, tingling, discomfort, or a lack of feeling in your feet.
What medication is most effective for foot pain?
The initial line of treatment for foot pain is frequently an oral painkiller, such as acetaminophen (paracetamol) or aspirin. It is also often suggested to take non-steroidal anti-inflammatory medicines (NSAIDs), which can also assist in decreasing inflammation. Ibuprofen and naproxen are two NSAIDs.
Reference
- O’Connell, K. (2022, February 7). What you need to know about foot pain. Healthline
- Foot pain. (2023, April 5). Mayo Clinic.
- Foot pain and problems. (2022, June 8). Johns Hopkins Medicine.
- Foot pain. (n.d.-b). Mount Sinai Health System.



2 Comments