Ketosis Explained: Benefits, Risks, and How to Achieve It
What is a Ketosis?
Elevated amounts of ketone bodies in the blood or urine are indicative of the metabolic condition known as ketosis. When there is insufficient glucose available, as occurs during fasting or low-carb diets, the body naturally goes into physiological ketosis.
Which gives the brain an extra energy source in the form of ketones. While blood ketones rise over normal ranges in physiological ketosis, the body’s acid–base balance is preserved.
In contrast, ketoacidosis is characterized by the uncontrollable synthesis of ketones in pathogenic conditions and results in a medical emergency known as metabolic acidosis. The most prevalent cause of ketoacidosis in people with type 1 diabetes or late-stage type 2 diabetes is total insulin insufficiency.
Blood, urine, or breath can be used to test ketones. In healthy ketosis, blood concentrations of ketones range from 0.5 to 3.0 millimolar (mM), however, in ketoacidosis, blood concentrations can reach more than 10 mm.
While blood glucose reserves are low and the liver switches from predominantly metabolizing carbs to fatty acids, trace quantities of ketones are always present in the blood and rise throughout these times.
This happens in conditions that cause enhanced fatty acid oxidation, such as famine, prolonged exercise, fasting, or carbohydrate restriction.
When fatty acids are quickly converted by the liver to acetyl-CoA, some Then, molecules can be changed into acetone, beta-hydroxybutyrate, and acetoacetate, which are ketone bodies. These ketone bodies have the ability to act as both signaling molecules and an energy source.
The ketone bodies are released into the bloodstream so that peripheral organs, such as the brain, can use them for energy since the liver is unable to use these molecules for energy.
Nutritional ketosis is the term used to describe ketosis that is brought on by a carbohydrate restriction. A ketogenic diet is a low-carb, moderate-protein plan that can induce ketosis. Type 2 diabetes and epilepsy are two conditions for which ketosis is a well-proven therapy.
Definitions
Less than 0.5 mM of ketone bodies are seen in normal blood levels. The standard definition of hyperketonemia is concentrations of more than 1 mM.
Physiological ketosis
The non-pathological (normal functioning) excess of ketone bodies known as physiological ketosis can be brought on by prolonged exercise, fasting, or extremely low-carb diets like the ketogenic diet.
It can also come from any condition of enhanced fatty acid oxidation. Serum ketone levels in physiological ketosis typically stay below 3 mM.
Ketoacidosis
Serum ketoacidosis is a pathological condition characterized by an uncontrollably high amount of ketones, usually more than 3 mM, and metabolic acidosis.
The most prevalent cause of ketoacidosis is an insulin shortage in people with type 1 diabetes or late-stage type 2 diabetes, although other causes include long-term excessive alcohol consumption, isopropyl alcohol absorption, and salicylate poisoning.
Significant metabolic disturbances are brought on by ketoacidosis, a potentially fatal medical condition. In contrast to physiological ketosis, ketoacidosis necessitates the breakdown of regular control over the synthesis of ketone bodies.
Causes
The most common reason for elevated blood ketone levels is increased ketone generation, however, exogenous ketones or precursors can also be consumed.
A metabolic shift takes place when blood glucose and glycogen levels are low, saving glucose for the brain, which cannot use fatty acids as fuel.
This change entails raising the liver’s fatty acid oxidation and ketone synthesis as a substitute energy source for the brain and the kidney, heart, and skeletal muscles. Always present in low blood levels, reduced glucose availability causes low levels of ketones to rise.
For instance, ketone bodies provide 2–6% of energy following an overnight fast and 30–40% during a 3-day fast.
Although the precise amount of carbohydrate restriction needed to enter a state of ketosis varies depending on a number of factors, including age, heredity, insulin sensitivity, and activity level, ketosis often happens when a person consumes less than 50 grams of carbs per day for at least three days.
Physiological ketosis is particularly quick to develop in newborns, pregnant women, and nursing mothers in response to energy-demanding situations like fasting or sickness. In the context of an illness, this can proceed to ketoacidosis, however, this seldom happens.
Newborns’ abnormally large central nervous systems, high-fat breast milk diet, and little liver glycogen all contribute to their propensity for ketone generation.
Biochemistry
Fatty acids from food or adipose tissue, as well as ketogenic amino acids, are the precursors of ketone bodies. Ketogenesis is the process by which ketone bodies are created in the liver cells’ mitochondrial matrix.
Adipokine signaling with low insulin and high glucagon and adrenaline levels can release fat from adipose tissue. Fasting and other periods, when there is little glucose available, are correlated with high glucagon and low insulin.
Coenzyme A-bound fatty acids enable entry into mitochondria. The attached fatty acids are mostly utilized as fuel by cells by beta-oxidation, which separates two carbons from the fatty acid once it is within the mitochondrion.
Every cycle to create acetyl-CoA from an acyl-CoA molecule. After entering the citric acid cycle, acetyl-CoA combines with oxaloacetate by an aldol condensation to produce citric acid.
This acid then proceeds to the tricarboxylic acid cycle (TCA), which extracts a high energy yield per carbon of the original fatty acid. Any cell may metabolize acetyl-CoA via the TCA cycle, but liver cells’ mitochondria can also use it for ketogenesis.
Oxaloacetate is diverted from the TCA cycle and utilized to create glucose by gluconeogenesis when there is a limited supply of glucose. The use of oxaloacetate in this may make it impossible for it to condense with acetyl-CoA due to gluconeogenesis, blocking entry into the TCA cycle.
In this case, acetyl-CoA may be converted into ketone molecules, which can be used to extract energy. Acetoacetyl-CoA is created during ketogenesis when two acetyl-CoA molecules condense thanks to thiolase.
Through the action of HMG-CoA synthase, acetoacetyl-CoA momentarily joins forces with another acetyl-CoA to generate hydroxy-β-methylglutaryl-CoA. Using HMG-CoA lyase, hydroxy-β-methylglutaryl-CoA forms the ketone molecule acetoacetate.
After that, acetoacetate can reversibly transform via D-β-hydroxybutyrate dehydrogenase into D-β-hydroxybutyrate, another ketone molecule.
Alternatively, acetoacetate can break down spontaneously into carbon dioxide and acetone, a third ketone molecule, producing substantially higher amounts of D-β-hydroxybutyrate and acetoacetate.
The resultant ketone bodies are exported from the liver to provide energy to the brain and other peripheral tissues since the liver is unable to utilize them for energy.
Deaminated ketogenic amino acids can be transformed into ketone bodies and intermediates in the citric acid cycle in addition to fatty acids.
Measurement
Tests for ketones can be performed on breath, blood, or urine. Since these approaches detect distinct ketone bodies, direct comparisons between them are limited.
Urine Testing
The most popular way to test for ketones is by urine. Utilizing a nitroprusside reaction with acetoacetate, urine test strips produce a semi-quantitative measurement based on the strip’s color change.
Urine test strips only measure acetoacetate, even though beta-hydroxybutyrate is the main ketone in circulation.
Because the kidney’s excretion of ketones varies, as well as because renal function and hydration state might have an impact, urine ketones frequently show weak correlations with blood levels.
Serum Testing
Like glucometers, finger-stick ketone meters provide rapid blood testing for beta-hydroxybutyrate levels. Lab tests can also be used to determine blood levels of beta-hydroxybutyrate.
Epilepsy
For refractory epilepsy, a ketogenic diet that induces ketosis is a well-established therapy.
Obesity and Metabolic Syndrome
By lowering blood triglycerides, raising high-density lipoprotein (HDL), and increasing the size and volume of low-density lipoprotein (LDL) particles, ketosis can improve metabolic syndrome indicators. Notwithstanding possible rises in the total cholesterol level, these modifications are consistent with a better lipid profile.
Safety
The safety of ketosis resulting from low-carb diets is frequently questioned by medical professionals, scholars, and the media. Misunderstanding the distinction between pathologic ketoacidosis and physiological ketosis is a typical cause for worry regarding safety.
Whether prolonged ketosis is a good condition or something to be avoided as a stressor is another topic of ongoing discussion. It is believed by some that humans evolved to eschew ketosis and that prolonged ketosis is not desirable.
The counterargument is that if sufficient energy can be produced via other means, there is no physiological need for dietary carbohydrates. Both ketogenesis and gluconeogenesis never stop.
On the other hand, it has been suggested that alternating between a fed and ketotic state is good for neurologic and metabolic health.
Studies of persons on rigorous ketogenic diets for type 2 diabetes or epilepsy have shown the impact of maintaining ketosis for up to two years.
They include short-term negative effects that may lead to long-term ones. There is, however, a dearth of research on the long-term implications of intermittent ketosis.
Medication Considerations
When in a state of ketosis, some drugs need to be taken carefully, particularly several types of diabetic treatments.
Euglycemic ketoacidosis, an uncommon condition characterized by elevated ketones that result in metabolic acidosis with normal blood glucose levels, has been linked to SGLT2 inhibitor drugs.
This typically happens when someone is unwell, forgets to take their insulin, is dehydrated, or follows a low-carb diet while taking the medicine.
Furthermore, hypoglycemia may arise from the use of drugs that directly decrease blood sugar, such as sulfonylureas and insulin, if their dosage is not adjusted before beginning a ketogenic diet.
Adverse Effects
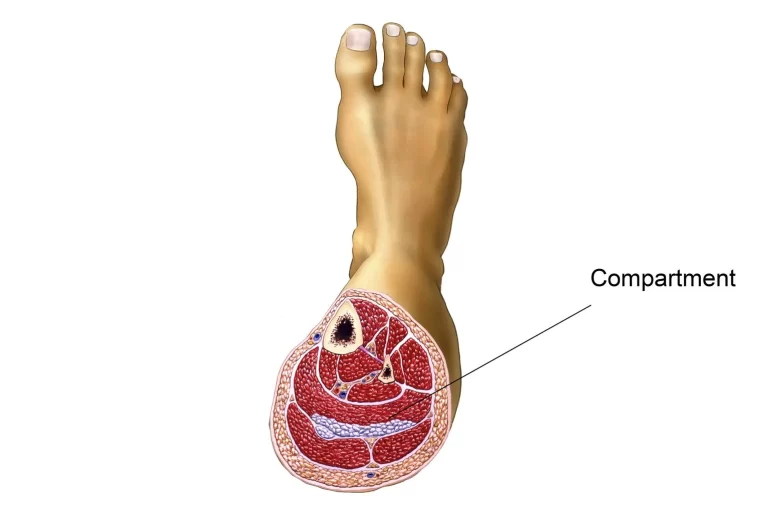
When switching from glucose metabolism to fat metabolism, there can be adverse repercussions. During the initial days and weeks of a ketogenic diet, symptoms including headache, tiredness, dizziness, sleeplessness, trouble tolerating exercise, diarrhea, and nausea may occur.
Because acetone is so volatile, it can produce an exhaled pleasant, fruity flavor in the breath.
Because long-term ketosis has been accepted as a therapy for pediatric epilepsy.
The majority of its side effects have been described in children. These include kidney stones, hyperlipidemia, stunted development, and weakened bones.
Contraindications
People with pancreatitis should avoid pursuing ketosis caused by a ketogenic diet due to the high-fat content of the diet. Furthermore, ketosis is excluded by pyruvate carboxylase deficiency, porphyria, and other rare hereditary illnesses of fat metabolism.
Veterinary Medicine
Ketosis, often known as acetonemia, usually sets up during the first several weeks following calf delivery in dairy cattle. When intake is insufficient to meet the increased metabolic demands of nursing, an energy deficit occurs.
Elevated amounts of β-hydroxybutyrate can suppress the immunological system, feed intake, gluconeogenesis, and milk composition. Screening for ketosis in cattle can be facilitated by point-of-care diagnostic testing.
Pregnancy toxemia is the term for ketosis in sheep, which is characterized by hyperketonemia (beta-hydroxybutyrate in blood over 0.7 mmol/L). This is related to the high metabolic needs of pregnancy and can occur in late pregnancy in ewes carrying multiple babies.
In ruminants, gluconeogenesis is required to provide glucose since rumen microbes consume the majority of the glucose in the digestive tract. Due to the metabolic demands of the fetus’s fast development, pregnancy toxemia is most likely to develop in the latter stages of pregnancy.
It can also be brought on by an inadequate diet. because of the environment, stress, or other factors. With a spontaneous birth, a Caesarean section, or an induced abortion, prompt recovery is possible.
Treatment for advanced stages of pregnancy toxemia is less successful than prevention by optimal nutrition and other management measures.
What are the benefits of ketosis?
There may be a number of health advantages to ketosis, according to research. Weight reduction is one of the main advantages of ketosis. You could consume less food as a result of the procedure if it makes you feel less hungry.
While preserving lean muscle, it can assist you in losing visceral fat, or belly fat. Ketosis may also be useful in the treatment and management of the following conditions:
Epilepsy: By modifying the brain’s “excitability,” medical professionals frequently place children with epilepsy on the ketogenic diet in an effort to lessen or even avoid seizures.
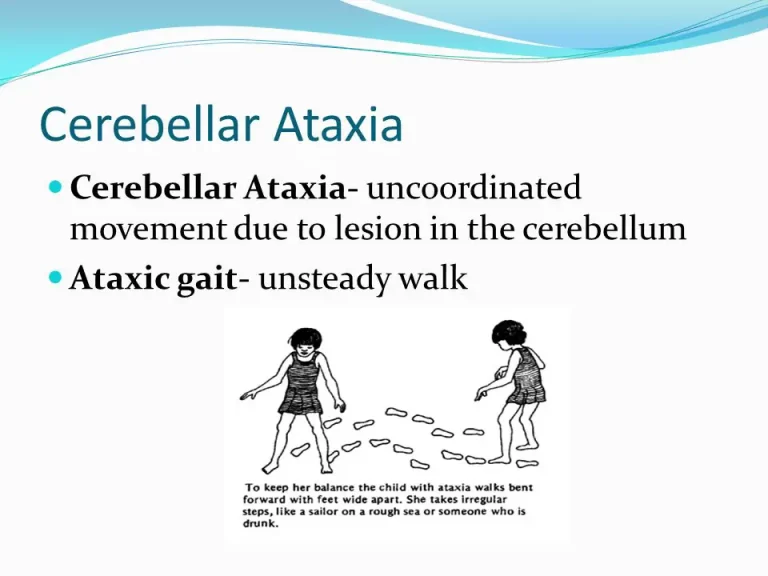
Additional neurological disorders: Studies have indicated that the ketogenic diet may benefit neurological disorders including glioblastoma, autism, and Alzheimer’s disease.
Type 2 diabetes: Those with this condition can control their blood sugar levels and reduce weight by following the ketogenic diet.
Heart disease: By reducing blood pressure, raising HDL (“good”) cholesterol levels, and lowering triglycerides, the keto diet may reduce your chance of acquiring cardiovascular disease.
Metabolic syndrome: The ketogenic diet has been linked to a lower risk of heart disease and may help prevent the development of metabolic syndrome.
It has also been demonstrated that ketosis improves energy and attention. The ketogenic diet lowers inflammation by providing your body with the energy it needs. According to research, your brain processes ketones more quickly than glucose.
What are the side effects of ketosis?
While there are several advantages to the ketogenic diet, there may also be drawbacks. The “keto flu,” which consists of symptoms like headaches, exhaustion, and upset stomach, may be one of the indicators that a person is in ketosis. Additional signs of ketosis might be:
- rotten (“keto”) breath.
- diarrhea.
- sleeplessness.
- dryness of the body.
- Osteopenia, or low bone density, and bone fractures.
- Hyperlipidemia, or high cholesterol.
- kidney-shaped stones.
What is the ketosis Diet?
The way your body utilizes food is altered by the ketogenic (or “keto”) diet. The majority of the fuel your body needs is usually found in carbs. By cutting back on carbohydrates, the keto diet trains your body to use fat for energy instead of carbs.
Low in carbohydrates, moderate in protein, and high in fat is the ketogenic diet. 70% to 80% of the food is fats, 10% to 20% are proteins, and 5% to 10% are carbs in a normal ketogenic diet.
Carbohydrates are present at large levels in many nutrient-rich diets. Fruits, vegetables, and whole grains fall under this category. The ketogenic diet restricts carbohydrates in all forms.
Foods that supply fat for the ketogenic diet include.
- Fish and meats.
- hens.
- Seeds and nuts.
- Cream and butter.
- Cheddar.
- oils like canola and olive oil.
It means you’ll have to drastically reduce your diet of fruits and vegetables and give up all bread, cereal, and other grains.
FAQ
Does my body benefit from being in ketosis?
A well-liked low-carb weight-loss regimen is ketosis. Ketosis can help you feel less hungry in addition to burning fat. It also aids in maintaining muscle. After consuming fewer than 50 grams of carbs per day for three or four days, ketosis often sets in for healthy individuals who are not pregnant or have diabetes.
What is ketosis in fasting?
The term “keto” refers to the metabolic state that occurs when your body begins using stored fat instead of glucose, which is its preferred energy source. When you fast for just 12 hours, as many individuals do before they “breakfast” with a breakfast meal, your body may enter ketosis.
How long is it safe to be in ketosis?
Gulotta advises sticking to a ketogenic diet for no more than six months before reinstating carbohydrates to your diet. Similarly, Scott Keatley, RDN, of Keatley Medical Nutrition Therapy in New York City, argues that the evidence is yet insufficient to advocate any one diet as a permanent solution.
Do you pee more in ketosis?
Increased Urination: Because keto is a natural diuretic, you will need to use the restroom more frequently. A ketone substance called acetoacetate is also expelled through urine, which may cause novices to use the restroom more frequently. Dry Mouth: Decreased thirst and dry mouth are caused by increased urine.
Does urine smell when in ketosis?
These can have a popcorn-like scent to the urine as the body excretes them. When a person experiences ketosis, their blood or urine has a high concentration of ketones. When the body does not have enough glucose or sugar for fuel, it will create ketones. This might occur during a fast or during the night.
Who benefits from ketosis?
Ketogenic diet-following children with epilepsy get fewer seizures. Bodybuilders and endurance athletes also utilize it to burn fat fast.
Does ketosis mean weight loss?
The body enters a state known as ketosis when there are insufficient carbohydrates. The body becomes extremely adept at burning fat and utilizing it as fuel during ketosis, as opposed to glucose. The ketogenic diet is a popular option for those trying to lose weight because of its ability to burn fat.