Mononeuritis Multiplex
What is a Mononeuritis Multiplex?
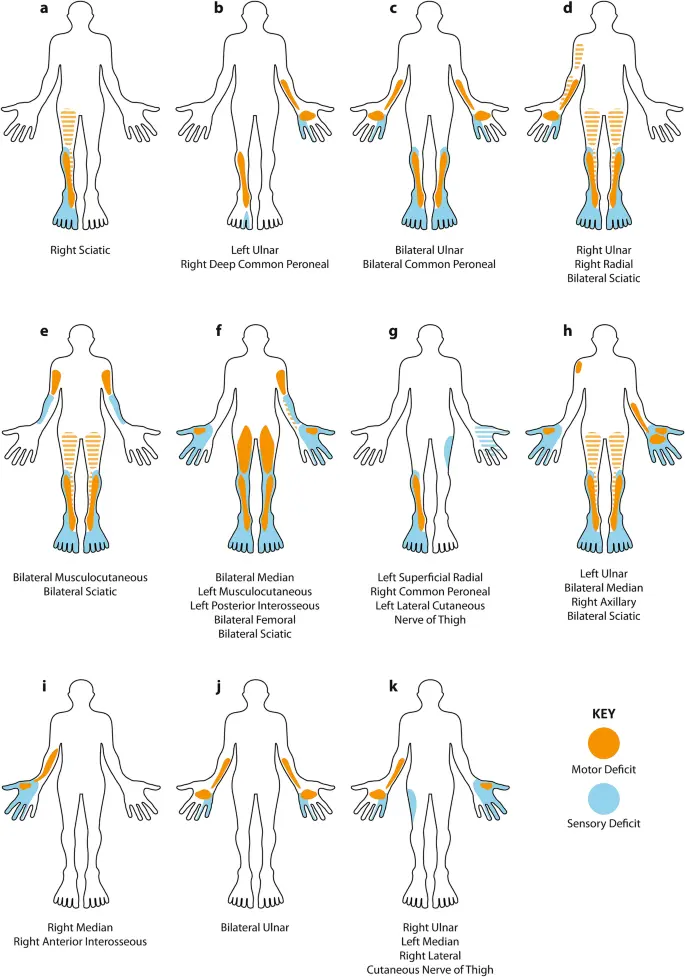
Mononeuritis multiplex (MNM) is a neurological disorder characterised by severe pain, impaired motor function, and diminished sensation in at least two distinct regions of the body. The specific areas affected by mononeuritis multiplex vary based on the underlying cause of the condition.
Introduction
Mononeuropathy multiplex, also referred to as mononeuritis multiplex, involves lesions affecting two or more nerves without a single root or plexus injury explanation. It typically develops subacutely in an asymmetric, non-length-dependent pattern.
If the process advances, it can mimic both clinically and electrophysiologically more common polyneuropathies. An extensive evaluation is crucial, particularly as treatable autoimmune and inflammatory causes are frequently identified.
A. Nerve Conduction Studies and Electromyography (NCS/EMG):
Performed for all suspected cases to confirm the nerve injury pattern and characterise specific nerve pathology (demyelinating vs. axonal).
B. Hereditary Neuropathy Consideration:
In cases with multiple mononeuropathies at common compression sites and a family history of polyneuropathy, hereditary neuropathy with liability to pressure palsies (HNPP) and familial amyloidosis should be considered. HNPP may show moderate diffuse slowing of motor conduction velocities, while familial amyloidosis might present with autonomic dysfunction or systemic disease.
C. Neurolymphomatosis and Graft-Versus-Host Disease:
Direct invasion of nerve roots or peripheral nerves by lymphoma cells (neurolymphomatosis) and graft-versus-host disease in bone marrow transplant patients require a nerve biopsy for diagnosis.
D. Leprosy Consideration:
In endemic areas, leprosy can cause axonal mononeuritis multiplex. Tuberculoid leprosy may lead to nerve injuries around skin lesions, while lepromatous leprosy can result in more diffuse nerve damage.
E. Uncommon Causes:
Lead toxicity, associated with an isolated motor neuropathy, and chemical exposure (n-hexane) causing a motor-predominant axonal multifocal neuropathy are rare but noteworthy.
F. Primary and Secondary Vasculitides:
Primary vasculitides, including polyarteritis nodosa (PAN), granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis, often involve the peripheral nervous system. Secondary vasculitic neuropathy can be caused by cryoglobulinemia and autoimmune diseases, necessitating treatment targeted at the underlying condition.
G. Nonsystemic Vasculitic Neuropathy:
Isolated vasculitis of peripheral nerves without other organ involvement requires monitoring, as up to 10% may eventually develop systemic vasculitis. A biopsy of both muscle and nerve aids in diagnosis, and treatment parallels that of systemic vasculitis.
H. Amyloidosis Consideration:
Suspected in cases with autonomic dysfunction or systemic disease, confirmed by serum protein electrophoresis. A fat pad or nerve and muscle biopsy may reveal amyloid deposition.
I. Multifocal Motor Neuropathy (MMN):
It presents similarly to anterior horn cell disease, causing slowly progressive asymmetric weakness, often in the upper extremities. Anti-GM1 antibodies may be present.
J. Acquired Demyelinating Neuropathies:
Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy, when presenting as mononeuropathy multiplex (MADSAM), may exhibit asymmetric features. Distinguishing features in nerve conduction studies aid in differentiation from vasculitis.
Causes and Risk Factors of Mononeuritis Multiplex
Mononeuritis multiplex can impact anyone but is more prevalent in individuals with specific conditions. Although these conditions might trigger the occurrence of mononeuritis multiplex, they can range from mild to unidentified. Previously, identifying the underlying cause was challenging, but recent decades have seen improvements in this regard.
Conditions contributing to mononeuritis multiplex encompass diabetes mellitus, connective tissue diseases, and vasculitis, with vasculitis being the most common instigator. Diabetes mellitus and oxygen deprivation due to reduced blood flow are common causes, leading to cellular death.
Vasculitis, characterised by inflammation around blood vessels, can affect arteries surrounding peripheral nerves. This inflammation can occur in disorders like rheumatoid arthritis, scleroderma, and systemic lupus erythematosus.
Apart from diabetes and nerve compressions, rheumatoid arthritis stands out as a frequent cause, with studies revealing its presence in up to 56% of non-diabetic, non-compression-related mononeuritis multiplex cases, often undiagnosed until recently.
Other triggers include severe allergic reactions to drugs, violent responses to infections, and, rarely, direct bacterial or viral infections in nerves. HIV and hepatitis B infections, as well as tumours interfering with nerves, are also associated with mononeuritis multiplex.
Risk factors increase the likelihood of developing mononeuritis multiplex. While old age is a general risk factor for diabetes, elderly individuals with mild or undiagnosed diabetes are more prone to mononeuritis multiplex. Notably, only about one-third of those with the condition were diagnosed with the underlying cause before symptom onset.
Various diseases can lead to MNM, including:
- Polyarteritis nodosa
- Diabetes mellitus
- Rheumatoid arthritis
- Systemic lupus
Less common culprits for MNM encompass:
- Sjogren syndrome
- Wegener’s syndrome
- Lyme disease
- Sarcoidosis
- Amyloidosis
- Hansen’s disease (leprosy)
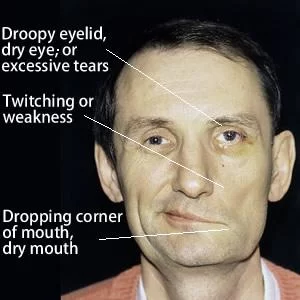
Symptoms of Mononeuritis Multiplex
The manifestation of symptoms depends on the type of nerves affected, and they may encompass:
- Weakness in one or more limbs
- Sensation loss in specific areas of the body
- Incontinence
- Partial paralysis
- Tingling or discomfort in various regions of the body
Diagnosing Mononeuritis Multiplex
To identify the cause of your mononeuritis multiplex, your doctor will gather a comprehensive medical history and conduct examinations, focusing on your neuromuscular system and reflexes. For a definitive mononeuritis multiplex diagnosis, two unrelated nerve areas must exhibit signs of impairment. Your doctor might recommend:
- Nerve biopsy: microscopic examination of a nerve
- Electromyogram: Assessment of the electrical activity in your muscles
- Nerve conduction tests: measurement of nerve impulse speed
Additional diagnostic measures may involve:
- Blood chemistry tests
- Imaging scans
- Rheumatoid factor test
- Thyroid tests
- Sedimentation rate
- X-rays
Treatments for Mononeuritis Multiplex
The approach to treating mononeuritis multiplex hinges on identifying the underlying disorder. A neuromuscular neurologist will tailor your treatment plan, possibly involving a consultation with a rheumatologist for connective tissue-related diseases like arthritis.
Treatment objectives encompass:
- Addressing the root cause
- Symptom control through medication or nutritional supplementation
- Providing support for increased independence
- Occupational Therapy: Your doctor may recommend occupational therapy (OT) to enhance mobility and independence. OT focuses on regaining daily activity skills, with therapists offering home or work environment assessments, exercise plans, and suggestions for adaptive equipment.
- Orthopaedic Aids: If mobility is challenging, orthopaedic aids like wheelchairs, braces, supports, and corrective shoes may prove beneficial.
- Physical Therapy: Incorporating stretching, strengthening exercises, and low-impact aerobics, physical therapy aims to enhance muscle strength, flexibility, and balance.
- Vocational Therapy: Vocational therapy (VT) assists in resuming employment, addressing changes in physical and mental function while aligning with your abilities.
- Medication: To manage pain, your doctor might prescribe anticonvulsants or antidepressants, especially for relief from stabbing pains.
Long-Term Outlook for Mononeuritis Multiplex
Achieving a full recovery from mononeuritis multiplex is plausible if the underlying cause is accurately diagnosed and effectively treated, with damage kept to a minimum.
The spectrum of disability varies, ranging from none to complete loss of movement or sensation.
Persistent nerve pain, requiring attention from a pain specialist, can be a notable challenge.
Decreased sensation in areas like your feet may lead to unnoticed injuries as nerves fail to transmit pain signals. Regular inspections for cuts or bruises are crucial to preventing potential severe infections in these areas.
Long-Term Complications Associated with Mononeuritis Multiplex
Several complications are linked to mononeuritis multiplex, encompassing:
- Muscle mass or tissue loss
- Kidney disease
- Gastrointestinal issues
- Pulmonary complications
- Corticosteroid-induced diabetes
- Impotence
FAQ
What is the difference between polyneuropathy and mononeuritis multiplex?
Signs and symptoms of polyneuropathies are typically length-dependent and indicate a widespread disease that affects all nerves in a roughly symmetrical manner. One nerve at a time is initially affected by the disease process in mononeuropathy multiplex, but gradually numerous nerves are affected, typically with significant asymmetry.
What is mononeuritis multiplex summation?
The most common types are polyneuritis (MM summation), mononeuritis, and mononeuritis multiplex (MM). The pure neuritic leprosy-presenting variant lacks the frequently occurring anaesthetic skin lesions. Peripheral nerve involvement, including cranial nerves, is frequently isolated.
What is mononeuritis multiplex, which is vasculitis?
Peripheral neuropathy may occasionally be among the initial signs of systemic vasculitis. Traditionally, individuals experience excruciating asymmetrical sensory-motor neuropathy, also known as mononeuritis multiplex. It is possible for several nerves in various body parts to be impacted in a sequential, stepwise manner.
Why is it called mononeuritis multiplex?
A painful, asymmetrical, asynchronous peripheral neuropathy affecting the motor and sensory systems, mononeuritis multiplex involves independent injury to at least two different nerve regions. It is possible for several nerves in various body parts to be impacted. The illness gets more symmetrical and less multifocal as it gets worse.
How do you diagnose mononeuritis multiplex?
Laboratory testing, electrodiagnostic testing, and nerve biopsy are the main methods used in the diagnosis of MNM. Studies on the conduction of sensory and motor nerves aid in distinguishing primary axonal neuropathies from primary demyelinating neuropathies and also show the location of the neuropathy.
What nerves are involved in mononeuritis multiplex?
When mononeuritis multiplex affects two or more peripheral nerves, nerve roots, or cranial nerves, it usually manifests as a progressive, asymmetrical progression of sensory and motor symptoms.
What medication is used for mononeuritis multiplex?
Corticosteroids, immunosuppressants, anticonvulsants, prokinetic agents, tricyclic antidepressants, and cholinergic antagonists are among the medications used for mononeuritis multiplex.
What is the differential diagnosis of mononeuritis multiplex?
The following conditions should be taken into account when making a differential diagnosis of mononeuritis multiplex: monomelic ischemic neuropathy. Paresthetic fatigue. Brachial plexopathy is caused by neoplasms.
Is mononeuritis multiplex an autoimmune disease?
A rare autoimmune peripheral neuropathy, mononeuritis multiplex usually manifests as a paraneoplastic disease, vasculitis, diabetes, or infection.
What is mononeuritis multiplex in DM?
The unusual diabetic neuropathy known as mononeuritis multiplex is characterised by the acute or subacute asymmetric sensory paralysis of two or more peripheral nerves. Vasculitis is the most frequent cause.
Is mononeuritis multiplex the same as amyotrophy?
In contrast to diabetic amyotrophy, which progresses more quickly and primarily involves proximal, almost purely motor involvement, mononeuritis multiplex includes slower stepwise progression, distal extremity involvement, and sensory-motor multifocal abnormalities.
Can mononeuritis multiplex be cured?
If the nerve injury is minimised and the underlying cause is identified and addressed, a full recovery is achievable. There are those who are not disabled. Some people lose their ability to move, function, or sense entirely.
Reference
- “What Is Mononeuritis Multiplex?” News-Medical.net, 11 Mar. 2021, www.news-medical.net/health/What-is-Mononeuritis-Multiplex.aspx.
- Underwood, Corinna. “Mononeuritis.” Healthline, 10 Feb. 2022, www.healthline.com/health/mononeuritis.