Neuro Developmental Treatment (NDT) Techniques
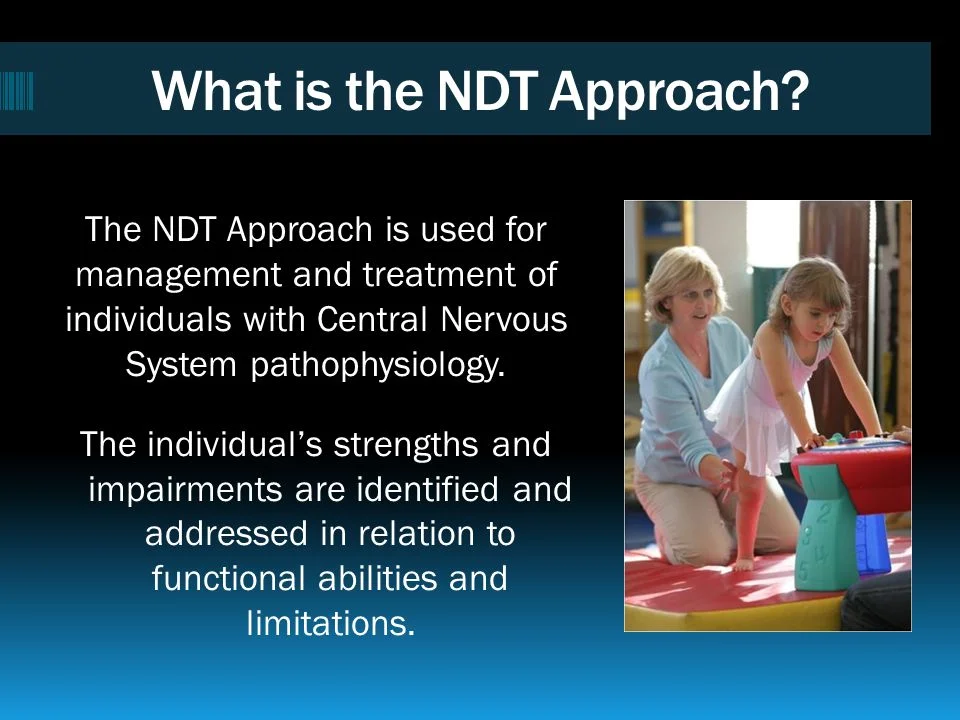
What is a Neuro-Developmental Treatment (NDT) Technique?
Neurodevelopmental treatment (NDT) is a clinical practice model used by physical therapists, occupational therapists, and speech-language therapists who work with people with stroke, traumatic brain injury, cerebral palsy, or other related disorders.
This therapy uses facilitated movements as a treatment strategy to ensure the correlation of input from tactile, vestibular, and somatosensory receptors within the body.
Theoretical approach
-NDT, first known as ” The Bobath approach” was initially developed by the bobaths in the mid-1900s and is now practiced worldwide.
-NDT is identified as a problem-solving approach but simultaneously is known for being a hands-on process.
-the therapist uses an international classification of functioning disability and health model in a problem-solving approach to assessing activity and participation thereby identifying and prioritizing relevant integrities and impairments as a basis for establishing achievable results with patient and caregivers.
-In the 1990s Cerebral Palsy patients were managed only by surgery and orthotics. The bobaths put together the philosophy of the bobath approach that increased the scope of physiotherapy in cp.
-Based on the hierarchical reflex theory of motor control. NDT intervention aimed to inhibit abnormal postures and tone by holding the child in reflex-inhibiting postures. but it was not found to be very effective.
NDT evolution
- The decreased tone of muscle through the use of reflex-inhibiting postures.
- Incorporation of hierarchical motor sequences into therapy, which one activity following another during facilitation (head control, rolling, sitting, quadruped, kneeling).
- Facilitation of involuntary movement sequences which is opposed to isolated developmental skills.
- It is recognized the need to direct the treatment toward particular functional movements.
Living concept
1. Bobath began
-Problem-solving approach based on reflex/hierarchical models.
-Hierarchical model of CNS structure and function.
-CNS is viewed as the “controller”.Automatic postural control mechanism simplified the responsibility of the CNS in control of movement.
-Sensory feedback is key for the correction of movement errors.
-“Positive signs” including spasticity and abnormal coordination of movement are the most important aspect of sensorimotor impairments.
-Muscle and postural tone determine the quality of the patterns of posture and movement used in functional activities.
2. NDT is now
-Problem-solving approach based on a system model.
-Distribution model of CNS structure and function.
-The CNS determines the pattern of neural activity based on input from multiple intrinsic systems and extrinsic variables that establish the context for movement initiation and execution.
-Sensory feed-forward and feedback both are important for different aspects of movement control.
-The “Negative signs” including weakness, impaired postural control, and paucity of movement are recognized as equally important as “Positive signs” in limitation of function.
-Task goals, experience, patients learning strategies, movement synergies, energy, and interests all affect the quality of the final movement.
NDT assumption
- The impaired pattern of postural control and movement coordination are the primary problems in clients with CP.
- These system impairments are changeable and overall function improves when the problem of motor coordination is treated by directly addressing neuromotor and postural control abnormalities in a task-specific context.
- Sensorimotor impairment affects the whole individual the person’s function, place in the family and community, independence, and overall quality of life.
- Working knowledge of typical adaptive motor development and how it changes across the lifespan provides the framework for assessing function and planning intervention.
- NDT clinicians focus on changing movement strategies as a means to achieve the best energy-efficient performance for the individual within the context of age-appropriate tasks and in anticipation of future functional tasks.
- Movement is linked to sensory processing.
- Intervention strategies involve the individual’s active initiation and participation. Often combined with the therapist’s manual guidance and direct handling.
- NDT intervention utilizes movement analysis to identify missing or atypical elements that link functional limitations to system impairments.
- Ongoing evaluation occurs throughout every treatment session.
- The aim of NDT is to optimize function.
-The remainder of the theories are currently known as ” Traditional ” theories of motor control, including
- Rood’s Approach
- The bobath
- Brunnstrom
- PNF
- Carr and Shepherd
Key concepts
1. Normal development
-cephalocaudal ,proximal-distal ,gross to fine.
2.sensory-motor
-sensory feedback system.
3. components of normal development
-the interplay between stability and mobility.
-effect of postural reflex mechanism of movement.
- postural tone
- muscle tone
4. reciprocal innervation -an interplay between agonist and antagonist muscles during coordinated muscle movement
5. righting and equilibrium reactions
- righting reaction -restore and maintain the vertical position of the head in space, the alignment of the head and trunk, trunk and limbs.
- equilibrium reaction serves to maintain or regain balance during a shift in the center of gravity.
- the ability to disassociate movement.
- development of posture control in three planes of space.
6. sequences of motor development
7. Abnormal development
8. Sensory input as a means of bringing about changes
Current principle
-Patients with CNS dysfunction have problems with control of stability and mobility because of impaired feedback and feed-forward systems. Abnormal tone and abnormal movement should be inhibited, whereas normal tone and normal movement should be facilitated. Once the patient learns the typical movement patterns. He will be able to make functional gains as he moves more efficiently.
-For assessment, the therapist should have knowledge of the typical development and typical movement patterns. The therapist should observe and analyze and find the missing components of the movement.
-The therapy starts with preparatory work, stretching spastic muscles, ROM exercise, and weight bearing.NDT is a hands-on approach in which key points of control are used to facilitate normal alignment of posture and movement when the patient actively performs a task-based movement.
-The normal alignment should be maintained using adaptive devices when the therapist is not maintaining the alignment.
-All principles of motor learning
- Repetition
- Feedback
- Variability of task
-The therapist should maintain a working hypothesis and perform continuous re-examinations.
How it might work
-NDT uses sensory input through the key points to re-educate the patient’s internal reference systems so that he has more movement choices and greater efficiency of movement.
-The main is to give a sensorimotor experience because the learning comes from movement perception. Feedforward is developed as the child practices the task with the therapist’s guidance.
-The therapist provides less guidance and assistance as the infant takes over and anticipates postural and motor requirements.
The assessment of the process
-NDT focus to identify the client’s abilities and limitation in order to tailor an individualized treatment plan and provide a basis for comparing the patient’s abilities at a later point in time.
-Assessment consists of data collection, examination, and evaluation.
-The examination and evaluation are done at the beginning of treatment, before and after each session, at the end of each block of intervention, and at the end of the entire treatment.
- Initial contact
- Data collection
- Evaluation analysis
- plan of care(goals,objectives)
- Intervention plan
- Re-examination and evaluation.
Examination
-NDT focus to identify constraints that limit the client’s ability to perform functional activities.
Components
- Present and anticipated functional skills or limitation of skills.
- Posture and movement components and compensatory strategies.
- Anatomical and physiological status of all those systems that participate in functional limitations.
Functional skill
-Gross motor and fine motor control, communication skill, control of behavior and emotions.
-Functional abilities and limitations.
-Potential to change function.
-clusters of function and activity limitations.
-Relationship between participation and activity level.
-Assistive devices, splinting, and orthotics.
Observation of posture, movement, and compensatory strategies
-Spontaneous posture and movement.
-Typical and atypical posture and movement.
-compensatory movement strategies.
-Alignment,weight-bearing, balance, coordination, muscle and postural tone, and movement components.
Individual systems related to the function
-Neuromuscular system
-Musculoskeletal system
-Sensory, perceptual, and cognitive systems
-Regulatory system(arousal, attention, emotional and behavioral responses)
-Limbic system(emotions,fear,pain)
-Respiratory, cardiovascular system
-integumentary system(skin)
Measurement tools
-Norm-referenced tests(WeeFIM,AIMS,The school functional assessment)
-Criterion-referenced tests(COPM)
-Non-standardized tests(compare the performance of the patient at the beginning and at the end of the session)
Evaluation
-The therapist observes, describes, and formulates hypotheses, linking treatment planning with outcomes.
-Client’s internal and external resources.
-functional limitations and participation restrictions.
-The relationship between posture and movement components.
-Hypotheses regarding the impact of impairments on daily life activities.
-Potential to change.
-Intervention plan developed.
NDT intervention
-NDT focus differentiates NDT intervention from other approaches is the precise therapeutic handling, including facilitation and inhibition which are used to provide sensorimotor cues that facilitate change in ADL.
Principle of intervention
- Established a treatment plan with anticipated outcomes that include specific, observable functions within a specific time frame under specific environmental conditions.
- The therapy utilizes the client’s strengths and recognizes that each individual has competencies and disabilities.
- Set anticipated outcomes and impairment goals in partnership with the family, the client, and the interdisciplinary team.
- Treatment strategies often include preparation and stimulation of critical foundational elements.
- It includes planning and solving motor problems.
- Repetition is an important component of motor learning.
- Create an environment that is conducive to cooperative participation and support of the client’s efforts.
- knowledge of the development of posture and movement components is used in designing treatment strategies.
- A single treatment session progresses from activities in which the client is most capable to activities in which the client is capable to activities that are more challenging.
- NDT intervention methods include modifying the task, or the environment, and taking into account the current level of the client’s performance and capacity for function.
- Individual treatment sessions are designed to evaluate the effectiveness of treatment with the session.
- Families receive information regarding the client’s problems and management of those problems, as they are able to understand and assimilate the information.
- In an NDT approach, suggestions to the family are as practical as possible.
- NDT recommends an interdisciplinary model of service.
Sequence of intervention
-Preparatory activities for body alignment.
-Selection of the main points for therapeutic treatment according to the child’s postural tone.
-Facilitation of active movement patterns by applying graded and various therapeutic inputs.
-The key points are the places of physical contact between the therapist’s parts of body or therapy equipment and the patient’s body.
Proximal key points
-Located closer to the source of the problem, at the head, trunk, or large joints.
-used to influence posture and movement in all three planes (sagittal, frontal, and transverse), especially during difficult moments.
Distal key points
-Located away from the source of the problem, usually at the upper and lower extremities level.
-Used to allow the patient to engage in activities with minimal control of the therapist.
Facilitation
-Facilitation is the process of intervention that uses the improved muscle tone in goal-directed activity. facilitation techniques involve stimulation of the muscle activity to produce the desired motor response. It is related to the functional activities that need to be achieved.
-modifies postural control.
-Guides the child’s posture or movement during the activity.
-Techniques: Tapping and intermittent compression to provide proprioceptive and tactile stimulation.
Inhibition
- Inhibition is the most common method of intervention that reduces dysfunctional muscle tone and muscle activity.
- Reduces the intensity of spasticity.
- Reduces the effect of fluctuating muscle tone.
- Improve the range and variety of movements.
- Not used with hypotonicity.
- Techniques: traction and light joint compression. It is used in combination with facilitation.
Weight-bearing and weight-sifting promote
-postural alignment
-child’s movement
-proximal stability
Adaptive equipment and orthotic devices
-Allows more independent movement.
-Decreases the possibility of deformities and contractures.
-can be used by parents and other professionals to reinforce the therapy.
Role of play in NDT Intervention with children
-Motivates and engages the child.
-Provides proper stimuli for the development of normal movement patterns.
-Fulfills therapeutic goals.
-Facilitates the handling techniques.
-Facilitates the use of the gained movement in other activities.
-Allows observation of the child’s spontaneous and active posture and movement.
Bobath Therapy
-Bobath therapy is a problem-solving approach to physiotherapy treatment that aims to improve movement and postural control in individuals with damage to their central nervous system (brain and spinal cord). Many physiotherapists use the Bobath technique in the rehabilitation of patients with neurological conditions to improve the sensory and motor pathways and facilitate normal motion and motor control.
-Bobath therapy aims to regulate muscle tone, provide posture correction with special grip techniques and improve functions with the active participation of the individual. The facilitation of normal movement portion and their special performance according to the task, which includes strategies preserving muscles and joint uniformity, are critical elements of the Bobath Concept.
Principles Of Bobath Therapy
-Bobath depends on the brain’s ability to accept change, reorganize and recover after neurological damage.
The Bobath approach depends on a number of principles that include
-Encouragement of normal movement patterns.
-Focusing on the quality of movement.
-The normalization of muscle tone to facilitate active movement.
-All movement and posture in lying, sitting, and standing positions.
-Discouragement of compensatory movements.
-Discouragement of muscle strength training.
-Improvement of maximum functional recovery to promote the quality of life.
Children with cerebral palsy
-Treat the child as a whole.
-Basis for intervention is normal movement and their interrelationships.
-Treatment includes facilitation and inhibition using key points of body control.
- the abnormal tone is always inhibited.
- normal responses, once elicited, are always repeated.
Stages of hemiplegia and the bobath approach
1) Initial flaccid stage
-Treatment focuses on positioning and movement in bed to avoid the typical postural patterns of hemiplegia.
2)Stage of spasticity
-Treatment is a continuation of the previous stage with the goal of breaking down the total patterns by developing control of the intermediate joints.
3)Stage of relative recovery
-Treatment aims at improving the quality of gait and the use of the affected hand.
Treatment Techniques Of Bobath Therapy
Motor relearning programme
Sitting up at the side of the bed
1) From a supine position in bed: patient Flexing the affected leg while the therapist stabilizes the foot and leg that turn to the intact side. Therapist assists by lowering the legs from the bed and Flexing the head sideways while the therapist assists in sitting.
2) Mobility exercises perform in bed: Trunk Rolling and bridging
Balanced sitting
-Sitting on a firm surface(chair), hands in lap. feet and knees are resting on the floor approximately 15 cm apart.
-Head and trunk movements – patient Turning head and trunk to look over The right shoulder, returning to the mid position, and repeating it to The other side. Looking up at the ceiling, returning to mid-position, and looking down at the floor.
-Reaching actions – Therapists assist the patient in shoulder flexion over the affected side, they place one hand on the elbow and another hand on the wrist. Doing reach out with the affected arm forwarding, sideways, backward, returning to normal position.
Balanced standing
-Standing on a firm surface(floor), hands over the side of the body, feet apart, while the therapist stabilizes affected the side of the knee.
-Head and trunk movements: Patient Standing with feet apart, looking up at the ceiling, returning to upright, and looking down. patient Standing with feet apart on the floor, turn head and body and look behind, return to the normal position, and repeat on the other side.
-Reaching actions –Therapists assist the patient in shoulder flexion over the affected side, they place one hand on the elbow and another hand on the wrist. Doing reach out with the affected arm in forwarding, sideways, backward, and returning to normal position.
Standing up and sitting down
-Sitting on a chair, no armrests over arm supporter, feet rest on the floor, no flexion within the upper body throughout the action.
-Standing up – Start with upper body erect, feet placed backward. Patients swing their upper body forward at the hips and stand up. Therapists stabilize the affected foot and knee by placing one hand over the trunk and another hand over the knee, to prevent buckling.
-Sitting down – therapists assist with the movement while the Patient flexes the hip, knee, and ankles to lower body mass toward the seat.
Upper limb function
-Reaching: Forward (flexion at the shoulder), sideways (abduction at the shoulder), and backward (extension at the shoulder). The opening of the hand aperture between the thumb and fingers, an extension of the wrist, pronation, and supination.
-Grasping: Extension of the wrist and fingers. Abduction and conjunct rotation of the carpometacarpal joints of the thumb and fifth finger. Closure of fingers and thumb around the cylindrical object (tumbler).
-Holding: Flexion and extension of wrist holding object (rolled towel).
-Manipulation and finger dexterity: Flexion and extension of fingers. Multidirectional movement of the carpometacarpal joints of the thumb and fifth finger. active finger flexion and extension.
Bobath technique
In sitting
-Sitting on a firm surface, hands rest over a bed, feet flat on the floor, while therapist place one hand over the elbow and the other over the wrist Weight shifting to both sides done.
-Clasping both hands forward, turning to the sound side, While lifting the affected leg and crossing it over the sound side.
-Clasping both hands forward, turning to the affected side, While lifting the sound leg and crossing it over the affected side.
-Sitting with crossed legs. The affected leg is over the unaffected one, While both hands clasps and are placed over the knee.
-Flexion and extension of the knee. The therapist places one hand over the foot and the other hand over the knee.
From sitting to standing
-Clasping both hands forward by placing the affected foot parallel with the normal one on the floor. The therapist places one hand over the sacrum and another hand over the knee and helps them to stand up.
In standing
-both hands forward. Turning to both sides.
-Sitting and standing up.
-For movements of the arm.
-Elevation of arms with clasped hands.
-Moving clasped hands to face, while the therapist’s hand prevents retraction of the shoulder.
-overhead movement with clasped hand, while the therapist’s hand prevents retraction of the shoulder.
Handling
-Manner of controlling the patient through tone-influencing patterns
Tone influencing patterns
-Normal patterns of activity used to modify abnormal patterns of posture and movement.
a.Total TIPs: Whole body is controlled in a reversal of the abnormal pattern.
b.Partial TIPs: Some body parts remain free to move.
Positioning
Problems
-confused & disoriented
-Divided into two half
-No balance or arm supported on the affected side
-Fear of fall
-Abnormal attitude on the affected side
-No midline orientation
Treatment
-Self-orientation on the affected side.
-Carry weight on the affected side.
-Bilateral functioning – interplay.
-Explain the fact of the affected side.
-Passive movement.
-Proprioceptive feedback.
Nursing preparation
-Positioning & handling to avoid spasticity, contracture, shoulder pain, SHS, retraction of the affected side, and rejection.
Cooperation bet nurse & therapy
-Turning patient bed pans uses.
-Weight-bearing exercise.
-Trunk balance in sitting.
-Mobilization of the shoulder girdle.
Indications Of Bobath Therapy
-In Bobath, physiotherapists encourage a patient to move in a normal and energy-efficient way and prevent abnormal movement patterns in order to
-Normalize tone
-Regain motor control
-Make movements easier to achieve that are precise and goal-directed
-Improve posture
-Lengthen tight muscles to help reduce spasticity and contractures
-Improve ability with everyday activities
-Increase independence
-Achieve maximum potential
Facilitation-Inhibition
Facilitation
-It is a means by which movement is made easy, made possible, and made necessary.
Inhibition
-Involves decreasing the use of pathological movements and the effects of tonal dysfunction on movement.
-Facilitation and inhibition may be used simultaneously and may be applied throughout the session.
In current NDT practice it refers to the reduction of any underlying impairment that interferes with functional performance It can be used to:
-Prevent or redirect those components of a movement that is unnecessary and interfere with intentional, coordinated movement, Constrain the degrees of freedom, to decrease the amount of force the client uses to stabilize posture.
-Balance antagonistic muscle groups.
-Reduce spasticity that interferes with moving specific parts of the body.
Bobath trained Physiotherapist Analyses posture and movement within functional activities Sets meaningful goals with family Decides on treatment plan accordingly Aims to
-Change the atypical tone
-Mobilize tight structures
-Activate appropriate muscle groups
-Strengthen weak muscles
-Hands-on which improves the quality of posture and movement
-Take hands off to improve the child’s own activity
-Motivate a child’s problem-solving skills to improve independence
-Work within a suitable context to improve functional activities
-Some overlapping skills with occupational therapy, speech, and language therapy
Bobath-trained Occupational Therapist
-Analyses posture and movement within functional activities
-Sets meaningful goals with family
-Decides on treatment plan accordingly
Aims to
-Hands-on which improves the quality of posture and movement.
-Take hands off to improve the child’s own activity.
-Optimize perceptual skills.
-Optimize sensory processing.
-Work within a suitable context to improve functional skills.
-increase the child’s potential for independence within routine activities such as dressing, cutlery skills, and writing.
-Some overlaying skills with physiotherapy, speech, and language therapy.
-Frequently uses play and exploration to develop and learn many skills.
-CP can sometimes affect a child’s perceptual and sensory ability and their judgment of spaces and distances.
-Occupational therapy seeks to help overcome this by using carefully graded activities so that the child can move and use their eyes and hands more effectively to dress, eat, read, write and play with friends.
Bobath trained Speech & Language Therapist
-Analyses general posture and specific oral motor ability Set meaningful goals with family.
-Decides on treatment plan accordingly improving the quality of posture and movement in order to communicate and in relation to oral motor ability and speech breathing.
-Take hands off to increase the child’s own activity.
-Work within suitable conditions to increase functional skills with regard to eating, drinking, and communication including access to AAC.
-Improve the child’s potential for independence with functional activities.
-Some overlaying skills with physiotherapy and occupational therapy.
-Speech and Language Therapy deals not only with communication and speech but with all aspects of oral movement.
-Difficulties in coordinating the muscles necessary for speaking mean that children may also experience problems eating and drinking.
FAQS
What are NDT principles?
An advanced ‘hands-on’ therapeutic approach that helps to guide the presence of normal postural reflex mechanisms is fundamental to motor skill performance. The normal postural reflex mechanisms consist of righting and equilibrium reactions, reciprocal innervation, and coordination patterns that improve motor development, motor control, motor learning, and other supporting scientific principles to improve basic body functions.
Why is NDT important?
Assist CP child who has difficulties with postural control and movement performed against gravity and Enhance functional cortical reorganization for improving the child’s function, social participation, and quality of life. The Bobath approach also assists in early rehabilitation, consistency of practice, and a stimulating environment in order to promote recovery.
Is Bobath Therapy Effective?
The Bobath concept is used in conjunction with other treatments to provide the best possible outcome for the patient. There is moderate evidence for the superiority of bobath approaches such as it helps to improve movement and mobility by using a combination of techniques involving passive and active movements in a functional way in order to obtain functional independence.
What is the difference between Bobath and Brunnstrom?
Brunnstrom supports the view that treatment should emulate”evolution in reverse”, by developing motor behavior on primitive behavior, whereas Bobath urges therapists to bypass this intermediate stage by suppressing the pathological spastic patterns and training normal patterns immediately after the disorder.






7 Comments