Pelvic Floor Dysfunction
The pelvic floor is a collection of muscles and ligaments in the pelvic area. The pelvic floor works as a sling to support the pelvic organs, which include the bladder, rectum, and uterus or prostate. Controlling your bowel motions, urine, and, especially for women, sexual intercourse is possible by contracting and releasing these muscles.
Pelvic floor dysfunction causes your muscles to contract rather than relax. because of this, having a bowel movement may be challenging. Pelvic floor dysfunction, if left untreated, can cause pain, long-term colon damage, or infection. Initial treatments include biofeedback, pelvic floor physical therapy, and medicines.
What is the Pelvic Floor Dysfunction?
Pelvic floor dysfunction is the inability to relax and coordinate your pelvic floor muscles to make a bowel movement.
Your pelvic floor is a collection of muscles attached to the floor (base) of your pelvis (the bottom of your torso). These muscles serve as the support system that holds your body together. By wrapping around your pelvic bone, your pelvic floor muscles supply protection to numerous of your organs. Some of these muscles provide additional support by wrapping a sling around your rectum.
Pelvic floor dysfunction is a common disorder in which you are unable to effectively relax and coordinate your pelvic floor muscles when you have to pee or have a bowel movement.
If you are a woman or were assigned female at birth (AFAB), you may have discomfort during sex, and if you are a man or were assigned male at birth (AMAB), you may experience difficulty achieving or maintaining an erection (erectile dysfunction or ED).
The function of the pelvic floor is to keep the organs in the pelvis, which can contain the:
- Bladder
- Rectum
- Urethra
- Uterus
- Vagina
- Prostate
Individuals with pelvic floor dysfunction may contain weak or especially stretched pelvic floor muscles.
When the muscles stretch, or spasm, individuals may have problems in urinating and passing stool. When they strain, the organs within the pelvis may fall and push down on the rectum and bladder.
Generally, you’re able to go to the bathroom with no trouble because your body tenses and relaxes its pelvic floor muscles. This is just like muscular action, like tightening your biceps when you raise a weighty box or grasping your fist.
But if you have pelvic floor dysfunction, your body tightens these muscles instead of relaxing them as it should. This pressure means you may have:
- Problem evacuating (removing) a bowel movement.
- An insufficient bowel movement.
- Urine or stool that leaks.
Causes of The Pelvic Floor Dysfunction
Multiple problems can induce the structures of the pelvic floor to weaken, including:
- Age
- Systemic diseases
- Continuing health issues that drive improved pressure in the abdomen and pelvis, like a chronic cough
- Pregnancy
- Trauma during delivery
- Multiple deliveries
- large babies
- Operative delivery childbirth
- Traumatic damage to the pelvic area
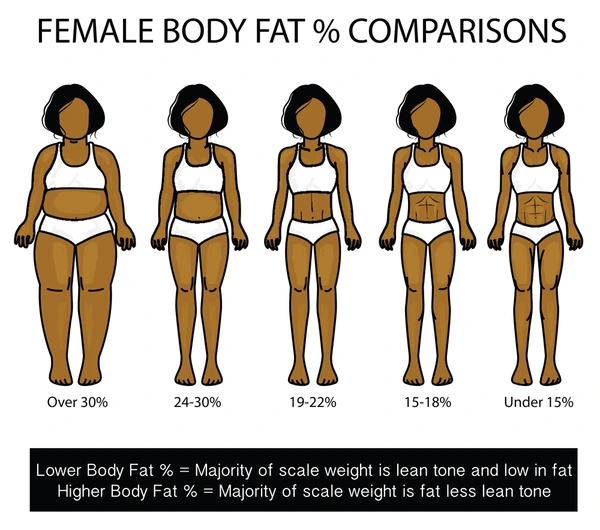
- Obesity
- pelvic surgery
- Nerve damage
- Around fifty percent of all women who have given birth experience stress urine incontinence, pelvic organ prolapse, or both.
- These problems are closely associated with birth-related damage to the pelvic floor muscles. There are multiple kinds of urinary incontinence.
- The pelvic floor muscles can also stretch inherently with age. Stress urinary incontinence and pelvic organ prolapse evolve more familiar with increasing age in females, for example. Collagen diseases can also involve the muscle’s ability to keep the pelvic organs.
- coccygodynia generally arises from trauma to the tailbone, likely to fall. In one-third of individuals with this disease, the cause of coccygodynia is unspecified. The ache can cause bowel movement challenging.
Sings and symptoms of The Pelvic Floor Dysfunction
Pelvic floor dysfunction can generate a mixture of signs and symptoms, and some can interrupt daily living activities. Depending on the kind of pelvic floor dysfunction, an individual may encounter.
- urinary problems, like the desire to urinate or hurting (urination incomplete urination)
- constipation or bowel anxieties (involuntary leakage of stool)
- bowel movement dysfunction
- lower back pain
- ache in the pelvic region, genitals, and rectum
- hurt during sexual intercourse for women
- stress in the pelvic area or rectum
- muscle cramps in the pelvis
- bulge somewhere in the lower pelvic region
- Stress urinary incontinence occurs when a small quantity of urination leaks from the body as a result of an action such as coughing.
Diagnosis for The Pelvic Floor Dysfunction
Normally, a healthcare practitioner will begin by inquiring about your symptoms and taking a complete medical history. The following questions may be asked by your provider:
- Have you ever had a urinary tract infection?
- Have you given birth, if you’re a woman?
- Do you experience pain when having sex as a woman?
- Do you have interstitial cystitis (a long-term bladder wall inflammation) or irritable bowel syndrome (a lower intestine disorder)?
- Do you have to strain to get a bowel movement?
Your clinician may also perform a physical exam to assess your ability to manage your pelvic floor muscles. Your clinician will examine these muscles with their hands for spasms, knots, or weakness. They may also need to do an intrarectal (inside the rectum) or vaginal exam.
Diagnostic test for Pelvic Floor Dysfunction
- surface electrodes (self-adhesive pads applied to your skin) can be used to assess your pelvic muscle control. If you do not wish to take an internal test, this may be an option. The electrodes are put on the perineum (the region between the vagina and the rectum in women and the testicles and the rectum in men) or the sacrum (the triangular bone at the base of your spine). This examination is not painful.
- Anorectal manometry (a test that determines how effectively your anal sphincters operate) can assess pressure, muscular strength, and coordination. This examination is not painful.
- A defecating proctogram is a test in which you are given an X-ray-visible enema of a viscous liquid. A unique video X-ray will be used by your provider to film the action of your muscles while you try to push the liquid out of your rectum. This will demonstrate how effectively you can pass a bowel movement as well as any other reasons for pelvic floor dysfunction. This examination is not painful.
- A uroflow test can determine how well you empty your bladder. If you have a weak urine flow or have to stop and start when urinating, this might indicate pelvic floor dysfunction. If you have urination difficulties, your doctor may request this test. This examination is not painful.
Treatment for The Pelvic Floor Dysfunction
In many circumstances, pelvic floor dysfunction is treatable. If you require physical therapy, you will most likely feel better after a few months of sessions. Pelvic floor dysfunction is treated non-surgically.
Nonsurgical treatments:
- Modifications to a Lifestyle
- Diet: to treat urine frequency and incontinence, avoid alcohol, caffeine (found in cola, tea, and coffee), acidic meals and beverages (like citrus and tomatoes), concentrated sugar, artificial sweeteners (like aspartame), spicy foods, and cigarettes.
- Weight loss: A 3% to 5% weight loss can result in a 50% reduction in episodes of urine incontinence.
- Medications: A key component of treating pelvic floor dysfunction is taking daily medication that promotes smooth, regular bowel movements. Stool softeners are among the over-the-counter pharmaceuticals that may be purchased at the pharmacy. A gastroenterologist or your primary care physician might advise which drugs are best for maintaining soft stools.
- Pelvic floor physical therapy: Pelvic floor physical therapy: Biofeedback treatment is frequently used with physical therapy at the same time. Your therapist will identify the tight muscles in your pelvis, lower back, and pelvic floor and will provide you with stretches to enhance the coordination of these muscles.
- biofeedback: This method uses devices to measure how well your pelvic floor muscles contract. Most likely, your PT will employ biofeedback to monitor your progress and assess how well your workouts are working. Electrodes could be positioned externally, for example, in the space between your vagina and anus. Alternatively, they may evaluate the tension and relaxation of your pelvic floor muscles using an inside probe. On a computer screen, the results are shown, and your PT will go over them with you.
- Relaxation techniques: You may also be advised to try relaxing methods like yoga, acupuncture, meditation, warm baths, or physical therapy by your healthcare physician or physical therapist.
Surgical treatments
When non-operative treatments fail to provide enough relief from symptoms related to anatomic prolapse, surgical procedures become necessary.
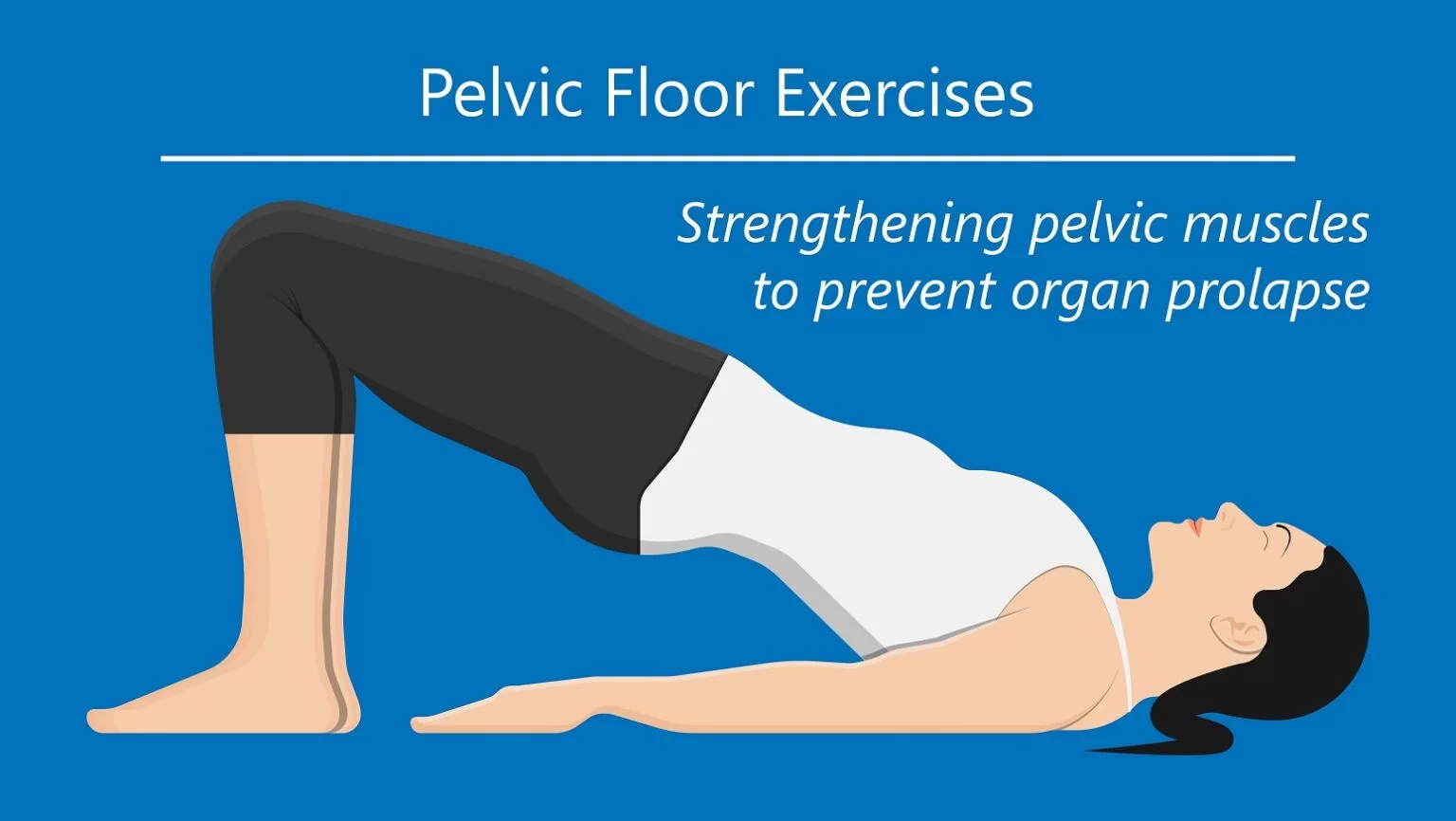
Physical therapy for The Pelvic Floor Dysfunction
Physical therapy includes:
- Electrical stimulation therapy
- Exercises therapy
Electrical stimulation therapy
- This method aids in decreasing pelvic discomfort and muscle spasms. Muscle electrostimulation is a useful tool for improving awareness, helping to strengthen weak pelvic floor muscles, and reminding them of how to function.
- Other electrotherapy modalities, such as TENS (transcutaneous electrical stimulation) and us(ultrasound), are used to treat overactive bladder and relieve discomfort.
Exercises therapy
- Creating a program that divides the exercises into two categories for those with hypotonic and hypertonic pelvic floor muscles is one approach to creating it.
- If your pelvic floor is low-toned, you are hypotonic, which suggests you need to build and enhance your power and endurance.
- If your pelvic floor muscles are hypertonic, they need to be stretched and relaxed because they are either excessively tight or hyperactive.
Exercises for hypotonic pelvic floor muscles
Kegels exercise

For those with pelvic floor dysfunction, kegel exercises are one kind of exercise for the pelvic floor muscles that may be effective. The muscles that support your rectum, bladder, uterus, and small intestine can all be strengthened by them. This can lessen urine incontinence, enhance sexual function, and aid with bladder control.
To Perform a Kegel exercise.
- Consider that you try to stop the urine’s flow in the middle.
- Put as much force as you can into your pelvic floor muscles, hold them for a little while, and then release them.
- repeat this ten to fifteen times. Three times a day,
Heel slides

Heel slides stimulate pelvic floor contractions while targeting the deep abdominal muscles.
To perform heel slides
- Start by laying on the floor with your pelvis in a neutral posture and your knees bent.
- Breathe in through your lips and into your rib cage, allowing your ribs to naturally collapse.
- Slide your right heel away from you, engage in your core, and raise your pelvic floor. Go only as far as it is safe to go without losing your connection to your deep core.
- Take a deep breath and return your leg to the beginning position when you’ve found the lowest position. and repeat.
- Perform ten backward and forward slides, then switch to the other leg.
Marches(Toe Taps)
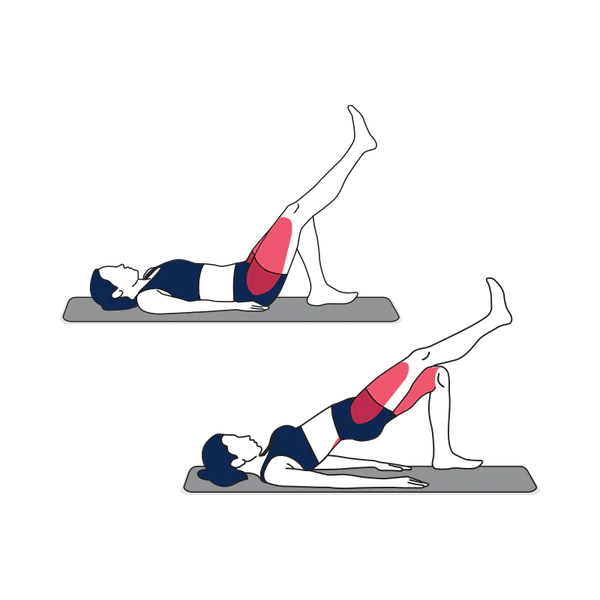
Like heel slides, the marching exercise improves core stability and boosts pelvic floor contractions.
To perform marches:
- Start by laying on the floor with your pelvis in a neutral posture and your knees bent.
- Breathe in through your lips and into your rib cage, allowing your ribs to naturally collapse.
- Tighten your abdominal muscles and raise your pelvic floor.
- Raise one leg slowly to a tabletop posture.
- Lower this leg gradually to the beginning position.
- Repeat with different legs each time. There shouldn’t be any lower back discomfort. You must maintain engagement of your deep core throughout the whole workout.
- Repeat steps 8 to 10 times in total.
Exercises for hypertonic pelvic floor muscles
Individuals with tight or short pelvic floor muscles may find some relaxation and lengthening with hypertonic exercises.
Happy Baby Pose

When the intention is to release and stretch the pelvic floor, the Happy Baby Pose is an excellent exercise.
To perform Happy Baby Pose
- Start with bending your knees while lying on the floor.
- With the soles of your feet facing up, bend your knees 90 degrees towards your belly.
- Either grab and grasp your feet inside or outside.
- Your knees should be somewhat broader than your torso when you open them. Next, raise your feet until they are in your armpits. Verify that your ankles are longer than your knees.
- Place your feet firmly in your palms and flex your heels. You can gently rock back and forth or hold this posture for a few breaths.
Diaphragmatic breathing

Breathing diaphragmatically promotes the pelvic floor and diaphragm’s functioning interaction. Stress reduction may also be aided by it.
To perform Diaphragmatic breathing
- On a yoga or fitness mat, start by laying flat on the floor. The exercise may also be done while sitting down.
- Practice gradual relaxation for a few seconds.
- Put one hand on your tummy and the other on your chest when you’re comfortable.
- To make your stomach grow, inhale through your nose while keeping your chest mostly steady. After two to three seconds, inhale gently and exhale. repeat a few times.
When to see a doctor
- Consult a physician if you suffer from unpleasant constipation, trouble urinating or passing stool, pelvic discomfort, or pain during sex.
- A lower pelvic bulge that is not normal may also be a reason to visit a doctor, however, a bulge by itself may not be significant.
- Treatment options for pelvic floor dysfunction are numerous. It could be awkward to discuss this subject with a doctor, but it’s crucial to get expert guidance on these symptoms.
- Pelvic floor dysfunction is a condition that some family physicians may not be aware of, but experts like gynecologists, urologists, and colorectal doctors may assist in identifying the problem and suggest a treatment plan.
Summary
Although anybody can have pelvic floor dysfunction, pregnant women are more susceptible. Different factors can lead to different forms of pelvic floor dysfunction, therefore before creating a treatment plan, a physician must determine the underlying problem.
Some patients with pelvic floor dysfunction may benefit from exercise. A doctor may also suggest medication, surgery, pessaries, diet modifications, or biofeedback, depending on the underlying reason.
FAQs
How can you tell if you have a pelvic floor problem?
When coughing, sneezing, laughing, or running, urine leaks. unable to reach the toilet in time. When leaning over or lifting, wind can escape from either the anus or the vagina. The vaginal feeling is diminished.
How can I check the strength of my pelvic floor?
Technique for female-Lie down and insert one of your fingers inside your vagina. Try to squeeze your vaginal muscles around your finger. You should be able to feel the feeling in your vagina, as well as the pressure on your finger. You are working the correct muscles if you can feel this.
How can I strengthen my pelvic floor quickly?
Squeeze your pelvic floor muscles up to 10 times while standing, sitting, or lying down to strengthen them. Hold your breath and do not tense your stomach, bottom, or thigh muscles at the same moment. When you’re comfortable with pelvic floor exercises, consider holding each squeeze for one second
Which exercises should you avoid if you have a weak pelvic floor?
Avoid high-impact physical activity that includes jumping heavy heavy objects or sustained increases in intra-abdominal pressure, such as double leg lifts.
References
- Professional, C. C. M. (n.d.-b). Pelvic floor dysfunction. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/14459-pelvic-floor-dysfunction
- What is pelvic floor therapy? (2021, May 21). WebMD. https://www.webmd.com/women/what-is-pelvic-floor-physical-therapy
- Physio for All Ltd. (2017, June 16). Pelvic floor therapy – PHYSIO FOR ALL. PHYSIO FOR ALL. https://www.physio4all.com/therapies/pelvic-floor-therapy/
- Pelvic floor dysfunction. (n.d.). Physiopedia. https://www.physio-pedia.com/Pelvic_Floor_Dysfunction