Pericardial Vein
What is the Pericardial Vein?
Although the period “pericardial vein” is not always used in conventional anatomical terminology, it’s far considered barely much less traditional. Still, upon closer examination, the most apparent word refers to the muscular tissues related to the pericardium the fibrous sac that surrounds the coronary heart. You in most likelihood speak that some muscles move the pericardium or have something to do with it in discussing anatomy. These are often referred to as cardiovascular or cardiovascular connections:
- Pericardial veins: These are tiny veins that return deoxygenated blood from the heart to the systemic venous circulation after draining the pericardial sac, which is the fibrous lining of the heart, and typically larger veins that are close by.
- Pericardial venous plexus: This refers to the vasculature on the pericardium that draws blood from the pericardial portion of the heart. These muscles may be important in regulating fluid balance and pressure in the heart.
Can you describe the location and function of the pericardial vein?
Certainly! Capillaries transport fluid out of the double-walled pericardial sac, which is where the coronary heart beats. This is an example of their surroundings as well as the setting for artistic endeavours.
- Installation: Located within the pericardial sac, a fibrous serous tissue that surrounds the coronary heart.
- Infiltrating arteries: These arteries are usually slightly opaque but surround the pericardial cavity between two layers of the pericardium: the ventral layer (which connects directly to the coronary heart) and the lateral layer (K stretch). Fibers near the rear of the heart, beneath the nose
- Communication: Pericardial arteries usually drain into larger arteries. Popular includes the following:
- Azygos vein: This main vein runs just beside the thoracic vertebral column and enters the superior veins Left superior intercostal vein: This vein draws blood from the pericardium, which is located on the left side of the chest wall and feeds the extra blood into the left brachiocephalic vein.
Function:
- Pericardial drainage: The primary function of the pericardial hollow space is to empty venous blood from the pericardial hollow space. The pericardial sac can store small amounts of fluid, those vessels help adjust that fluid and make certain it returns to the systemic movement.
- Cardiac pressure regulation: These capillaries help regulate pressure and fluid stability in the pericardial sac which is necessary to keep the heart functioning properly to stop conditions including atrial fibrillation, which can increase pressure around the heart and potentially affect its ability to pump properly
- Supportive function of the heart: Adequate pericardial drainage The heart pump works best to prevent excessive fluid accumulation that can impair the ability of the pericardial cavity to support the heart pump.
In conclusion, despite being as well known as other vital vessels such as the jugular or thoracic veins, the pericardial vessels are important for the health of the pericardial sac because they contain universal cardiovascular inputs required for strength and the water balance has been preserved.
How does the pericardial vein differ from other veins in the body?
Extracardiac vasculature differs from other vasculature in several important ways, often related to location, purpose, and physiological state. Examination of the peripheral nerves is shown below, and there are many nerves in the frame.
- where: the vein around the heart
- Location: Within or next to the pericardial sac of the heart. They are smaller and less conspicuous than the bigger veins.
- Communication: usually drains straight into a major vein, like the azygos or the left advanced intercostal vein.
Other muscles:
Major vessels: Some vessels include the upper and lower veins and thoracic and pelvic veins. These vessels are large, effortlessly visible, and demonstrate another important role in regulating blood flow between the heart and various organs.
- Systemic and pulmonary circuit: Major vessels are related to systemic current (e.g. Shirakawa) or pulmonary flow (e.g. pulmonary veins).
Function:
- Pericardial Veins:
- Basic Function: Deoxygenated blood ought to be again from the outer portion of the heart, which is a hole at the heart, to the circulatory machine of the human body. It is critical to manipulate the fluid and pressure tiers in the cardiac sac.
- Main Function: It is involved with the preservation of cardiovascular fitness and the prevention of immoderate fluid accumulation.
- Additional muscle tissues:
- Primary arteries: Their massive-ranging responsibilities embody bringing oxygenated blood from the lungs (pulmonary arteries) or the frame (systemic veins) once more to the coronary heart.
- Uses: Nerves are important in high-quality sections of the trunk, no longer simply in emptying the liver or the top and neck.
Anatomical Characteristics:
- Pericardial Veins:
- Size and form: They are normally smaller and less outstanding in comparison to larger veins.
- Complications: additionally it is a band across the sac of the heart and isn’t without difficulty detected through conventional anatomy.
- Other muscles:
- Size and form: Larger veins are large and more outstanding, making them less difficult to identify and study.
- Direct routes: Their routes are more direct and join immediately to the essential verbal exchange channels.
Clinical advantages:
Extracardiac veins:
- Clinical Concern: Issues associated with this artery are pericardial effusion (accumulation of fluid) or other coronary heart ailment. Compared to huge veins, their popularity is typically much less discussed.
Other muscle mass:
- Clinical importance: Large vessels are often concerned in medical analysis and remedy, collectively with venous thrombosis, atherosclerosis, and primary worried device involvement and their health is critical for cardiovascular disorder the overall characteristic.
In precis, even though the pericardial vessels ought to deliver fluid to the pericardial sac and keep its fluid stability, the alternative endovascular vessels play a unique direct position in blood motion as they’re regularly huge and substantially distinguished.
What are pericardial veins’ unique features or roles?
Pericardial vessels have precise residences and functions that distinguish them from different vessels within the body. Let’s examine their differences in extra detail.
Unique Features:
- Smaller and much less apparent:
- Size: The heart muscle is commonly small compared to large muscle tissues such as the superior vessels or pulmonary arteries. They are not so prominent in conventional physiological mechanisms.
- Visibility: Due to their size and location, they are generally not very visible unless physical examination or detailed photographs are specifically required.
Location of pericardial sac:
- These vessels are found in or close to the pericardial sac, which is made up of the muscles that encircle the heart. Because of this, their physiological setting is considerably different from that of tissues in other parts of the body.
- Pericardial plexus: A community or plexus is usually fashioned across the pericardial hollow space, which contributes to the drainage of this precise region.
Drainage works:
- Fluid control: The number one feature of the pericardial cavity is to cast off blood from the pericardial sac and go back to the circulatory gadget This helps to keep the fluid stability within the coronary heart.
- Pressure law: By pumping fluid outside the coronary heart, those muscle masses help adjust the pressure and extent of fluid across the heart, which is essential for preserving proper cardiac characteristic
Unique Roles:
Maintaining Pericardial Health:
- Preventing Effusion: They play a role in stopping immoderate accumulation of fluid (pericardial effusion) in the pericardial sac. Furthermore, an excessive amount of fluid increases the coronary coronary coronary coronary heart’s strain, which hinders the coronary coronary coronary heart’s potential to pump blood successfully.
- Ensuring normal traits: By effectively enjoying the pericardial region, one’s muscle organizations make a contribution to everyday coronary heart functions saving you troubles together with constrictive peripheral contamination.
- Supporting Cardiac Function: Equilibrium Pressure: Maintaining choicest pressure across the coronary coronary heart is made viable by way of proper pericardial sac drainage, which is essential for inexperienced cardiac filling and pumping.
- Fluid Homeostasis: They make contributions to the homeostasis of the pericardial fluid, making sure that the amount and pressure within the pericardial hole space are balanced.
Interconnection with Larger Veins:
- Drainage Pathways: Pericardial veins drain into extensive venous systems in conjunction with the azygos vein and the left advanced intercostal vein. This association assures that blood from the posterior cardiac sac receives an additional time of effective endothelialization.
Role in extracardiac conditions:
- Importance of diagnosis and treatment: Diagnosis and treatment of extracardiac problems may be important, in cases of pericardial effusion, pericardial disease, or problems affecting the pericardial cavity
Finally, pericardial vessels are unique because of their specific location in the pericardial sac, their significantly smaller size, and their important role in stabilizing and regulating the pericardial space because of the heart.
What anatomical structures are associated with the pericardial vein?
The pericardial arteries are associated with many anatomic structures in and around the pericardial sac, the coronary is a double-walled artery surrounding the heart The major anatomical structures associated with pericardial vessels are in detail: The posterior sac of the heart.
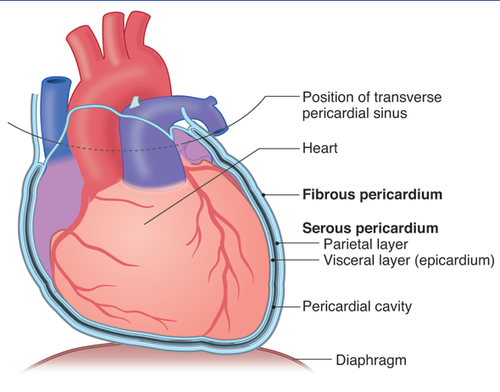
- Description: The pericardium sac is made from two layers: the interior serous pericardium and the outer fibrous pericardium. The inner layer, additionally known as the epicardium, connects at once to the coronary coronary heart, at the same time as the outer layer covers the fibrous pericardium.
- Relationship: Pericardial vessels drain blood from the pericardial cavity, that hollow space between the inner and outer serous membranes of the heart
Pericardial plexus:
- Description: These are muscles surrounding the heart sac. The pericardial plexus consists of small vessels that connect to shape the larger vessels.
- Relationship: This artery receives blood from veins outside the heart and pumps it to the great arteries.
Azygos muscles.
- Description: The azygos vein is a large artery that passes through the common part of the spinal cord and enters the superior vena cava
- Relationship: The azygos artery, which is the main part of the artery returning from the chest, receives the volume of blood flowing from the heart.
Superior intercostal muscles:
- This artery collects blood from the heart, causing damage to the chest wall before entering the left brachiocephalic artery.
- Relation: The left advanced intercostal vein is an extra-vital recipient of blood from the pericardial veins.
Phrenic Nerves:
- Description: The phrenic nerves, which might be vital for diaphragm feature and sensation of the pericardial sac, run along the pericardial sac.
- Relationship: Being close to the pericardial sac is critical to comprehending its shape, no matter the truth that they now not talk with the coronary heart muscle mass immediately.
Blood vessels:
- Description: Blood is transported to the myocardium by the use of pulmonary veins and arteries. The capillaries empty into the right ventricle after draining into the diaphragm.
- Relationship: The pulmonary artery is anatomically near the pericardium but has a unique permeability.
After the heart:
- Description: The coronary heart muscle, together with the phrenicopericardial ligaments, connects the pericardium with the diaphragm and system.
- Relationship: These muscle tissues make contributions to the outer sac of the heart, which influences the orientation of the cardiac outflow.
Heart Chambers and Great Vessels:
- Description: The cardiac sac consists of both the chambers of the coronary heart (atria and ventricles) and the outstanding vessels (aorta, pulmonary arteries, and arteries).
- Relationship: Pericardial vessels are components of the vascular device that adjust blood flow around those structures, contributing to the go-back of all vessels from the pericardial hollow space.
In precis, pericardial vessels and lots of large vessels consisting of pericardial sac, pericardial plexus, azygos vein, left superior ventricle, and many others. Are involved. Their area and characteristics are key to retaining fluid stability and stress in the pericardial hollow space, helping universal cardiac characteristics.
How does it interact with the pericardium and other nearby structures?
The pericardial veins engage with the pericardium and different nearby structures in several important methods:
Interaction with the Pericardium:
Drainage of Pericardial Space:
- Function: The primary role of the pericardial veins is to drain blood from the pericardial area, that is the cavity between the visceral layer (epicardium) and the parietal layer of the serous pericardium. This helps in overseeing the fluid equilibrium within the pericardial sac.
- Mechanism: Blood from the pericardial area enters the pericardial veins, which then channels it into big venous systems. This drainage prevents immoderate accumulation of fluid within the pericardial hole area, which could in any other case cause conditions like pericardial effusion.
Pressure Regulation:
- Function: The pericardial veins help in maintaining the pressure and fluid quantity in the pericardial area by means of putting off blood from the pericardial sac. For the coronary coronary heart to persist in functioning well, this is important.
- Mechanism: The coronary heart can also agree and make bigger generally without being too squeezed with the aid of the encompassing fluid whilst the pericardial hollow space’s pressure is saved and balanced via proper drainage.
Interaction with Nearby Structures:
Azygos veins:
- Communication: Some extracardiac arteries drain into the azygos artery. The azygos vein runs along the right side of the thoracic vertebral column and eventually drains into the superior vena cava.
- Function: This connection allows deoxygenated blood to flow back to the heart by pooling fluid from the pericardial cavity into the larger return vessels
Left superior intercostal vein:
- Communication: Blood is drawn from the left pericardium and chest wall by the left superior intercostal vein, which then empties into the left brachiocephalic vein.
- Function: This channel facilitates efficient revascularisation by offering an alternate pathway for extracardiac venous blood flow back into the system.
Nerves of the Phrenic:
- Location: The phrenic nerves run parallel to the pericardial sac and may be involved in diaphragm innervation and sensory innervation to the pericardium.
- Role: While no longer at once concerned with venous drainage, the proximity of the phrenic nerves to the pericardium is important for expertise in the general anatomy and capacity effect on pericardial sensations and infection.
Coronary Vessels:
- Location: Blood is drained and extracted from the heart muscle by pulmonary arteries and veins. The coronary arteries collect blood from the coronary arteries to the right ventricle.
- Function: Although the myocardium has a distinct drainage system, its proximity to the myocardium underscores the close anatomical relationship between these systems Disturbances in one system can affect another.
External heart muscle:
- Location: The diaphragm and the pericardium are joined to structures by the phrenicopericardial ligament and other myocardial ligaments.
- Function: These muscle tissues help to position the pericardial sac, affecting the spatial connectivity and stress inside the pericardial place, which circuitously affects the function of the pericardial vessels
Clinical benefits:
- Pericardial effusion: Abnormal pericardial venous outflow can cause fluid to accumulate in pericardial effusion, resulting in pericardial effusion, that may compress the coronary heart and impair its characteristic
- Pericarditis: Pericardial infection can affect the pericardial vessels and their capacity to drain blood properly, inflicting symptoms including chest pain.
In the end, the pericardial veins interact intently with the pericardium via draining fluid from the pericardial space and maintaining strain stability. They moreover merge with greater enormous venous systems which include the azygos vein and left advanced intercostal vein, integrating their drainage into the systemic venous return machine. Comprehending those interactions is critical for diagnosing and managing situations affecting the pericardium and adjacent networks.
What is the embryological source of the pericardial vein?
The pericardial vein in most cases originates from the embryological improvement of the cardinal veins, mainly the anterior cardinal veins. Here’s a detailed evaluation of this system:
Embryological Development
Formation of Cardinal Veins:
- During early embryogenesis, the frame establishes a fundamental venous system constituted of paired cardinal veins. These include the northeast cardinal veins.
- The anterior glands drain the pinnacle, neck, and higher limbs, while the posterior glands drain the decreased frame.
Heart development:
- As the coronary heart matures, it starts offevolved as a simple tube that expands and modifications dramatically consisting of looping and septation.
- The heart is surrounded by a developing pericardial cavity, which paperwork from the lateral mesoderm.
Connection to the Pericardium:
- The pericardial veins are associated with the drainage of the pericardial cavity, which includes fluid that reduces friction among the heart and surrounding systems throughout motion.
- As the anterior cardinal veins develop, they also contribute to the venous system around the heart, consisting of veins with the purpose of draining into the pericardial cavity.
Formation of Specific Veins:
- Over time, particular branches from the anterior cardinal veins deliver an upward push to the pericardial veins, which help in draining the pericardial fluid again into the systemic venous circulation.
Summary
In summary, the embryological supply of the pericardial vein is usually the anterior cardinal veins, which can be part of the initial venous system fashioned all through embryonic improvement. These veins play a critical function in setting up the vascular connections across the growing coronary heart and the pericardial hollow space.
How does its development occur during fetal life?
The growth of cardiac muscle during embryonic life is part of the wider development of the nervous system and the heart. Here is a detailed account of the way this evolution occurs.
Formation of the principle muscle tissue:- Premature root development
Cardinal administrators: The number one tense device of the early testis has massive vessels, consisting of the anterior (head and top body drains) and the peripheral nerves (reduced body drains). Finally, these muscle groups make contributions to the regeneration process.
Vitelline and uterine muscles:
- Vitelline arteries: These arteries provide blood circulation between the uterus and the scrotum.
- Uterine veins: These veins carry oxygenated blood from the placenta to the baby. The growth of cardiac muscle during fetal life is part of the broader development of the nervous system and the heart. Here is a detailed account of how this evolution occurs.
Formation of the main muscles:- Premature root development
Cardinal officials: The primary fearful system of the early testes has huge vessels, along with the anterior (head and upper frame drainage machine) and the peripheral frightened system (lower frame drainage machine. Finally, these muscles contribute to the regeneration process.
Vitelline and uterine muscles:
- Vitelline arteries: These arteries provide blood circulation between the uterus and the scrotum.
- Umbilical vessels: The foetus receives oxygenated blood from the placenta through the umbilical vessels.
Development of the Pericardial Sac and Veins:
Formation of the Pericardial Sac:
- Pericardial Cavity Development:
- The inner and outer pericardium consist of the inner serous layer and outer fibrous layer of the sac, respectively.
- It is a water-filled chamber between the inside and the outside.
- Development of the myocardium
- The first artery around the heart:
- At the beginning of the embryo, small vessels begin to protrude through the heart sac into the empty space.
- These veins get up from the developing venous device, in particular from the cardinal veins and their derivatives.
- Connection with Major Venous Structures:
- Azygos Vein System: Some pericardial veins connect to the azygos vein machine, which is formed from embryonic cardinal veins.
- Other pericardial veins flow into the left advanced intercostal vein, which is a continuation of the embryonic intercostal veins.
- Integration into the Mature Venous System:
Maturation and Reorganization:
- Venous System Integration:
- As fetal growth continues, the fetal tissues undergo extensive reorganization and incorporate the mature vascular system.
- The pericardial vasculature evolves in response to developing physiology, interacting with the bigger vascular regenerative structures.
- Final Configuration:
- The pericardial veins begin as little veins towards the quit of fetal development and grow into huge venous structures with the left advanced intercostal vein and the azygos vein.
- They help to maintain the fluid percentage of the human heart’s coronary heart and drain the pericardial area.
Clinical Significance:
Pericardial Diffusion and Additional Disorders: To detect and treat disorders that impact the pericardial area and its associated venous drainage, such as pericardial effusion or pericarditis, it is vital to understand how the pericardial veins are improving.
Summary: The development of the pericardial veins takes place as part of the formation and maturation of the fetal venous device. Initially arising from the embryonic cardinal veins and their derivatives, those veins establish a community across the pericardial sac. They finally drain into larger venous systems like the azygos vein and the left superior intercostal vein, contributing to the preservation of fluid stability and pressure within the pericardial space because the fetal circulatory machine develops.
What is the blood supply and drainage pattern of the pericardial vein?
The pericardial veins are small veins that drain the pericardial sac, which is the hollow space surrounding the coronary heart. Their blood delivery and drainage pattern are part of a broader community of veins that manage venous return from the pericardial vicinity. Here’s a detailed look at their blood supply and drainage pattern:
Blood Supply:
- Pericardial Veins’ Blood Supply:
- The pericardial veins do not have a distinct or separate blood supply as they are small veins involved in the venous drainage of the pericardial sac.
- The blood delivered to the pericardial sac more often than not comes from the coronary arteries, which provide the coronary heart muscle and the visceral layer of the pericardium. The visceral layer of the serous pericardium (epicardium) gets its blood delivered from branches of the coronary arteries.
Drainage Pattern:
- Pericardial Veins Drainage:
- Blood from the pericardial hollow space should drain through the pericardial veins. Usually, that is a tiny amount of fluid or blood that is lower back to the systemic venous stream.
- Primary Venous Drainage Pathways:
- Azygos Vein:
- Some cardiac arteries enter the azygos artery, which runs along the right side of the thoracic spine.
- The azygos vein then controls the upward circulation, returning oxygen-poor blood to the right atrium of the heart.
- Left Superior Intercostal Vein: Other pericardial veins drain into the left advanced intercostal vein. This vein collects blood from the left aspect of the thoracic wall and the pericardium and then drains into the left brachiocephalic vein, which ultimately returns blood to the superior vena cava.
Summary of Blood Supply and Drainage Pattern:
Blood Supply: The sac of the coronary heart no longer incorporates the stream of blood from the precise arteries of the heart. Instead, the blood comes from the coronary arteries, which supply the arteries of the coronary heart muscle and the internal lining of the heart.
Drainage Pattern:
- Pericardial Veins drain the pericardial sac and empty into:
- Azygos vein: The longitudinal Shirakawa is drained by using the azygos vein.
- Left advanced intercostal vein: drains into the left brachiocephalic vein and into the superior vena cava.
By effectively draining blood from the pericardial place, the veins help preserve the fluid balance and stress within the pericardial hollow area, which is critical for normal cardiac traits.
Which veins or arteries are involved?
The peripheral nerves of the heart are connected to a number of tissues and are connected to many major arteries and veins. Here is a description of the most important muscles and vessels associated with the peripheral arteries of the heart.
The muscles involved:- Extracardiac veins:
- Procedure: Remove the pericardial sac, that fluid-filled cavity that surrounds the heart of the heart.
- Drainage: These small veins drain into large venous structures.
Azygos Vein:
- Connection: Some pericardial veins drain into the azygos vein.
- Pathway: The azygos vein runs alongside the right aspect of the thoracic vertebral column and drains into the advanced vena cava.
- Role: The azygos vein collects deoxygenated blood from the thorax, together with the pericardial veins, and returns it to the proper atrium of the heart.
Left Superior Intercostal Vein:
- Communication: Other postcardiac arteries drain into the left ascending intervertebral artery.
- Pathway: This vein collects blood from the left side of the chest wall and the posterior part of the heart, and drains into the left brachiocephalic vein.
- Function: The left advanced intercostal vein contributes to the blood going back from the chest to the superior vena cava.
Arteries Involved:- Coronary Arteries:
- Branches: The proper and left atrial branches branch into arteries that deliver the heart muscle and the internal outer part of the coronary heart (epicardium).
- Function: Blood is supplied to the heart and the inner pericardial cavity. Although not administered directly to the heart muscle, it is important for the health of the heart sac and surrounding tissues.
Pericardial Branches of the Internal Thoracic Artery:
- Communication: A branch of the subclavian artery arises from the pericardial branch which supplies the internal pericardium of the thoracic artery.
- Function: These branches help circulate blood outside the heart and surrounding tissues.
Summary:
Veins:
- Pericardial Veins: These veins join with larger veins after emptying the pericardial sac.
- Azygos Vein: Returns blood to the superior vena cava after receiving drainage from a few pericardial veins.
- Left ventricle: The left brachiocephalic ventricle receives blood, which then delivers it to the end of the human body’s upper heart muscle
The nervous system:
- Coronary Arteries: Coronary blood vessels that arise from coronary arteries and supply the coronary and pericardial arteries of the body.
- Pericardial Branches of the Internal Thoracic Artery: The blood is supplied to the parietal layer of the pericardium and nearby systems.
These arteries and veins work together to maintain the right features and fluid stability of the pericardial sac and assist universal cardiac fitness.
How does the pericardial vein contribute to the overall circulatory system?
By helping in the pericardial sac’s drainage and keeping the fluid stability surrounding the coronary heart, the pericardial veins aid the circulatory device as a whole. They paintings with and supplement the bigger circulatory machine in the following techniques:
Fluid Drainage and Pressure Regulation:
Drainage of the pericardial sac:
- Function: Responsible for the diversion of extra blood and fluid from the pericardial hole vicinity of the various pericardial and distal portions of the coronary heart
- Important: This drainage device is crucial to save you from fluid buildup (pericardial effusion) that would compress the heart and impair its characteristics.
Pressure Regulation:
- Function: By draining fluid from the pericardial sac, the pericardial veins help hold the ideal stress and extent in the pericardial area.
- Importance: Proper stress regulation is vital for ordinary coronary heart expansion and contraction, which supports powerful cardiac pumping.
Integration with Larger Venous Structures:
Connection of the azygos muscles:
- Pathway: A pericardial nerve enters the azygos nerve, which runs on the right side of the thoracic spine.
- Integration: The azygos artery then guards the superior vena cava, returning oxygen-deprived blood from the upper body to the right side of the heart This integration helps the entire artery return to the heart.
Communication of the left superior intercostal vein:
- Route: Other extracardiac arteries drain into the left ventricle.
- Communication: The left superior interventricular vein regulates the left brachiocephalic vein, which then contributes to the return of arteries through the superior vena cava This contributes to the return of arteries from the left ventricular side of the heart.
Contribution to Cardiac Function:
Support for Cardiac Efficiency:
- Function: By ensuring proper drainage and fluid balance in the pericardial sac, the pericardial veins assist premier coronary heart function.
- Importance: Effective cardiac feature is based on maintaining the best environment across the heart, which incorporates controlling pericardial fluid ranges and stopping constriction of the heart by using extra fluid.
Clinical Relevance:
Pericardial Effusion and Constrictive Pericarditis:
- Pericardial Effusion: Fluid buildup within the pericardial sac can also result from anomalies within the pericardial venous drainage. An excessive fluid accumulation that would jeopardize coronary coronary heart feature is prevented with right drainage.
- Constrictive Pericarditis: This infection is characterized by utilizing pericardial thickness and fibrosis, which may avert pericardial vein traits, coronary heart traits, and drainage.
- Diagnostic and Therapeutic Interventions:
Imaging and Procedures: Understanding the function of the heart muscles can help diagnose and treat conditions associated with pericardial fluid and stress Other techniques, such as echocardiography or pericardiocentesis, can follow pericardial arteries and pathways the process of drainage.
Summary: The cardiac muscle is fundamental for circulation by helping to cope with the contractions of the heart sac and maintaining fluid balance around the heart along with large vessels such as the azygos muscle and the left superior intercostal vein connects, allowing deoxygenated blood to flow through the right atrium Helps to regulate rudimentary communication.
How are pericardial vein disorders diagnosed?
Diagnosing issues related to the pericardial veins generally involves evaluating conditions that affect the pericardial area and its surrounding structures. Since the pericardial veins themselves are small and not normally the primary target of diagnostic exams, the point of interest is commonly on figuring out abnormalities in the pericardial vicinity that could impact those veins. Here’s a detailed overview of diagnostic procedures for conditions connected to the pericardial veins:
Clinical Evaluation
- Patient History:
- Symptoms: Patients may complain of dyspnoea (shortness of breath), chest pain, or coronary heart failure symptoms. A history of recent infections, injuries, autoimmune illnesses, or cancers is also relevant.
- Physical exam findings consisting of pericardial friction rub, jugular venous distension, or signs and symptoms of heart failure can provide clues.
Imaging Studies
Echocardiography:
- Description: An ultrasound is used to image the coronary heart and extracardiac space.
- Function: Critical for assessing intracardiac edema, the quantity and extent of fluid accumulation, and the effect of leakage on cardiac characteristics.
- Types: It Comprises transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE).
X-ray of the chest:
- Description: Provides visual inspection of the chest cavity and heart.
- Function: The heart may appear enlarged, indicating pericardial effusion or other problems. It is useful for measuring the size of the heart and the amount of fluid that can accumulate.
Computed Tomography (CT):
- Description: Creates a close-up of the detection part.
- Uses: Useful for detailed examinations of the pericardial, thoracic, or soft tissues, as well as for assessing the degree of intracardiac ischemia.
Magnetic resonance imaging (MRI):
- Description: Uses radio waves and magnetic fields to create highly detailed images.
- Function: Provides excellent soft tissue contrast for examination of the pericardium, detection of abscesses, cysts, or pericardium thickening, and assessment of their effects on the surrounding environment
Laboratory Tests
- Blood testing: Described as together with checking out for cardiac biomarkers (like troponins) and different pertinent markers, as well as checks for inflammatory markers (like C-reactive protein).
- Function: Aids inside the prognosis of underlying illnesses that may cause pericardial anomalies, inclusive of infections, autoimmune sicknesses, or cardiac injuries.
Pericardiocentesis
- Description: This is a manner that entails extracting fluid for research with the useful resource of placing a needle into the pericardial hollow area.
- Function: Provides diagnostic facts through lifestyle-monitoring urine tests as to whether cancer, infection, or unique drift-causing issues are most prevalent. In addition, it helps build stress for those with heart disease.
Advanced methodologies
Endomuscular biopsy:
- Commentary: In addition to tolerable myocardial biopsy.
- Application: Can be used in specific cases to diagnose conditions affecting the extracardium, including systemic or inflammatory diseases.
Electrocardiography (ECG)
- Description: Records the electrical hobby of the coronary heart.
- Role: Can assist in finding adjustments in coronary heart rhythm or symptoms and signs and symptoms of pericarditis. It is regularly used as a complementary take a look at in place of a primary diagnostic device for pericardial vein troubles.
Summary of Diagnostic Approaches:
Clinical diagnosis: Initial diagnosis is mainly based on signs and symptoms and physical examination.
Photography courses:
- Echocardiography: the primary tool for assessing cardiac output and output.
- Chest x-ray: cardiac imaging and initial assessment of fluid collections.
- CT and MRI: Deep pericardial effusions, looking for strokes, tumors, or vasoconstriction.
- Laboratory evaluation: Analysis of inflammatory markers and underlying conditions.
- Pericardioscencesis: diagnosis and treatment, urine donation for research purposes.
- Advanced methods: Primary diagnostic biopsy.
- ECG: Another device used to measure and adjust heart rhythms.
These diagnostic tools and techniques help identify and manage issues in the extracardiac space that affect the circulation of the coronary arteries.
What role does it play in maintaining cardiac function?
Through their assistance in the management of the pericardial location and promoting standard heart health, the pericardial veins play a modest however important position in maintaining cardiac characteristics. How they impact coronary heart characteristics is as follows:
Pressure Control and Fluid Balance
Endocardial Drainage:
- Function: The pericardial veins drain the pericardial sac, the area between the inner and outer heart muscular tissues.
- Important: This inflow helps to maintain the correct amount of fluid in the heart. Excessive accumulation of fluid (pericardial effusion) can increase the pressure around the heart and impair its function.
Pressure Regulation:
- Function: By maintaining the fluid balance in the pericardial sac, the pericardial cavity helps to maintain a constant pressure in the heart.
- Importance: Ensuring the heart can expand and settle properly depends on proper strain regulation. Reduced cardiac output and restricted coronary heart action can result from increased strain brought on by fluid buildup.
Support for Cardiac Filling and Contraction
- Facilitating Heart Movement:
- Function: Effective drainage by way of the pericardial veins facilitates saving excessive pressure from fluid accumulation, allowing the coronary heart to move freely in the pericardial sac.
- Importance: This freedom of motion is vital for the heart’s diastolic filling (while the heart relaxes and fills with blood) and systolic contraction (while the heart pumps blood out). Restricted movement can reduce the performance of those strategies.
Integration with Venous Return System
- Connection to Major Venous Structures:
- Function: The pericardial veins drain into larger venous structures along with the azygos vein and the left superior intercostal vein.
- Importance: These connections combine pericardial drainage with the systemic venous return device, making sure that blood from the pericardial location is lowered back to the coronary heart efficaciously. Proper venous return is critical for maintaining cardiac preload (the extent of blood inside the ventricles earlier than contraction) and universal cardiac output.
Impact on Cardiac Conditions
Pericardial Effusion:
- Role: Fluid may acquire in the pericardial sac (pericardial effusion) in times wherein the pericardial veins aren’t running at their quality.
- Effect: Breathlessness, chest ache, and a discount in cardiac output are some of the signs and symptoms that could stand up from this expanded strain on the coronary coronary coronary heart. Headaches are less common when the heart muscle is in a good state.
Pericarditis with:
- Function: In conditions such as constrictive pericarditis where the pericardium is thick and fibrous, the pericardial vasculature may fight for proper drainage
- Consequences: This can lead to worsened cardiac filling and decreased cardiac output. Understanding how the cardiovascular system works under these circumstances can help to diagnose and manage such problems.
Summary
The pericardial veins play a vital role in retaining cardiac function by way of: We are ensuring powerful drainage of pericardial fluid to save you immoderate pressure around the coronary heart. Supporting the coronary heart’s potential to extend and contract freely, is critical for proper filling and pumping. We are integrating with the bigger venous go-back device to keep green blood flowing to and from the coronary heart. Proper functioning of the pericardial veins is vital for keeping the fluid stable in the pericardial sac and supporting typical coronary heart health and efficiency.
What are common pathologies or disorders associated with the pericardial vein?
The pericardial veins themselves are not generally the direct recognition of many pathologies, nevertheless, problems regarding the pericardial space or adjoining systems can affect their characteristic and bring about numerous complications. Here are a few commonplace pathologies or problems related to the pericardial area and the veins involved in its drainage:
Pericardial Effusion
- Excess fluid buildup inside the pericardial sac is described.
- Cause: Irritation (pericarditis), infection, trauma, cancer, or cardiac failure are possible outcomes.
- Impact on Pericardial Veins: Excess fluid can increase pressure in the pericardial space, probably impairing the drainage function of the pericardial veins and inflicting discomfort or problems in coronary heart growth and contraction.
Constrictive Pericarditis
- Description: Thickening and fibrosis of the pericardial sac, can restrict the heart’s ability to fill properly.
- Cause: Often results from persistent irritation because of tuberculosis, radiation therapy, or other infections.
- Impact on Pericardial Veins: Fibrosis of the pericardium can affect the drainage of the pericardial veins and contribute to bad fluid management and impaired cardiac filling.
Cardiac Tamponade
- Description: An intense form of pericardial effusion in which fluid accumulates rapidly and exerts considerable pressure on the heart.
- Cause: This can be because of trauma, malignancy, or severe infection.
- Impact on Pericardial Veins: Increased strain from fluid accumulation can crush the pericardial veins’ ability to drain the pericardial space, leading to decreased cardiac output and symptoms of heart failure.
Pericarditis
- A buildup of fluid or thickening of the pericardial layers can be the final effects of pericardial infection.
- Cause: Frequently delivered on with the aid of autoimmune diseases, viral infections, or cardiac infarction.
- Impact on Pericardial Veins: By converting the pericardial fluid dynamics and possibly causing pericardial effusion or fibrosis, inflammation might also affect the pericardial veins
Heart Pericardiac Cysts
- Description: Fluid-crammed sacs that may expand inside the pericardial space.
- Cause: Congenital or acquired; regularly asymptomatic.
- Impact on Pericardial Veins: Large cysts can exert strain on surrounding systems, in all likelihood affecting the function of pericardial veins and normal pericardial fluid stability.
Tumors or Masses in the Pericardial Space
- Description: Primary or metastatic tumors can grow inside the pericardial space.
- Cause: Cancers, which encompass mesothelioma, or the spread of severe malignancies metastatically might be the purpose of this.
- Effect on Pericardial Veins: Tumours can hinder the pericardial veins, which ends up in awful drainage and fluid retention. This also can enhance the strain on the coronary heart valves.
Summary of Impacts on Pericardial Veins:
- Impaired Drainage: Disorders like pericardial effusion or cardiac tamponade can crush the pericardial veins’ potential to drain excess fluid, leading to improved pressure across the coronary heart.
- Pressure Effects: Conditions like constrictive pericarditis or large pericardial cysts can physically affect the function of the pericardial veins by altering the space and fluid dynamics.
- Inflammation and Fibrosis: Pericarditis and other inflammatory conditions can change the nature of the pericardial space and potentially impact the pericardial veins’ ability to function properly.
These conditions regularly necessitate clinical evaluation and intervention to control fluid stability and stress within the pericardial space, ensuring superior cardiac features and ordinary cardiovascular health.
Are there conditions that specifically affect it?
While the pericardial veins themselves are not often the number one recognition of specific conditions, certain pathological situations and issues can mainly impact the pericardial area and not directly affect the pericardial veins. There are cases where there will be a specific injury to the heart muscle or part of the heart where the muscle is placed.
Pericardial effusion: formation of fluid in the pericardial cavity.
Effects on the cardiovascular system: Excess fluid causes pressure in the heart sac, which in turn can exacerbate symptoms of myocardial infarction, leading to symptoms such as shortness of breath, chest pain, or stress signs and symptoms that have occurred.
Cardiac Tamponade
- Description: An immoderate form of pericardial effusion wherein fluid accumulates unexpectedly and exerts great pressure on the coronary heart.
- Impact on Pericardial Veins: Rapid accumulation of fluid can compress the pericardial veins and prevent them from correctly draining the pericardial vicinity. This can motivate intense cardiovascular compromise and calls for urgent medical intervention.
Constrictive Pericarditis
- Description: Thickening and fibrosis of the pericardial sac restrict coronary heart filling.
- Impact on the Pericardial Veins: The fibrotic pericardium can disrupt the venous system, causing it to return from the pericardial cavity, resulting in decreased drainage via the pericardial veins. The illness is typically characterized by heart failure and reduced cardiac output.
pericardial cyst
Description: Expanded fluid-filled sacs in the heart.
- Effects on pericardial arteries: Large pericardial arteries can put stress on pericardial arteries and affect permeability, certainly if they cause pain or objective issues it occurs depending on tumor length and location of tumors outside the heart
- Description: Primary metastatic or tumor in the cardiac region.
- Effects on pericardial muscles: Tumors can obstruct or compress pericardial arteries, especially disruption of secretion and power fluid accumulation. Symptoms can also vary depending on tumor size and location.
Pericarditis
- Description: Inflammation of the pericardium, which can be because of infections, autoimmune illnesses, or publish-cardiac harm.
- Impact on Pericardial Veins: Inflammation may additionally result in fluid accumulation (pericardial effusion) or fibrotic adjustments, that could affect the pericardial veins’ potential to drain successfully.
Pericardial Adhesions
- Description: Fibrous adhesions among the pericardial layers could arise after surgical operation or irritation.
- Impact on Pericardial Veins: Adhesions may adjust the anatomy of the pericardial area and probably affect the drainage characteristic of the pericardial veins.
Hemorrhagic Pericardial Effusion
- Description: Accumulation of blood in the pericardial sac, usually due to trauma or malignancy.
- Effects on pericardial arteries: Blood accumulation can increase pressure in the pericardial cavity, and certainly with symptoms damaging pericardial arteries and with excessive signs and symptoms due if treated early results
An overview of the effects on the peripheral myocardium:
- Perfusion is intact: Conditions that encourage fluid accumulation or stress alterations in the extracardiac region can influence the effectiveness of myocardial vasculature in the well-awakened heart.
- Increased pressure: Excess fluid or abscesses can raise the pressure in the pericardial sac, unfavorable to the heart muscle.
- Physical obstruction: Large tumors or tumors can bodily clog the veins because of negative drainage and related signs.
Even if non-pericardial veins are now not the number one choice, troubles with the pericardium may additionally have a particular effect on their residents, needing cautious control to cope with various underlying symptoms and signs to be able to maintain adequate cardiac output.
What diagnostic tools or techniques are used?
Diagnosis of extracardiac events usually requires examination of conditions affecting the heart and its surroundings because the myocardium itself is small, currently generally not central to the goals of research investigations, so they often focus on the wrong things rather than on the hearts that can be made of clay. Here is a detailed explanation of the diagnosis of conditions associated with cardiovascular disease.
Clinical Evaluation
- Patient History:
- Symptoms: Patients may present with chest pain, shortness of breath (shortness of breath), or signs and symptoms of congestive heart failure History of recent infection, depression, illness immune system, or malignancy is also appropriate.
- Physical Examination: Findings including pericardial friction abrasions, jugular venous dilatation, or signs of heart failure may be clues.
Imaging Studies
- Echocardiography: An ultrasound is used to image the heart and extracardiac space. Important for the evaluation of intracardiac edema, the dimensions and quantity of fluid accumulation, and the evaluation of the impact of leakage on cardiac function. There are many types: Includes transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE).
- X-ray of the chest: Chest X-rays offer a visual examination of the chest cavity and heart. It may show an enlarged picture of the heart showing abnormalities such as pericardial effusion. It is helpful to check the size of the heart as well as any fluid that may accumulate.
- Computed Tomography (CT): Computed Tomography (CT) is a close-up image of a part of the body. Useful for detailed evaluation of pericardial, thoracic, and soft tissues, as well as for assessing the degree of intracardiac hemorrhage.
- Magnetic resonance imaging (MRI): Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to create incredibly detailed images. It also provides excellent soft tissue contrast for examination of the pericardium, detection of abscesses, cysts, or pericardium thickening, and assessment of their effects on the surrounding environment
Laboratory Tests
- Blood testing: Described as together with checking out for cardiac biomarkers (like troponins) and different pertinent markers, as well as checks for inflammatory markers (like C-reactive protein).
- Function: Aids inside the prognosis of underlying illnesses that may cause pericardial anomalies, inclusive of infections, autoimmune sicknesses, or cardiac injuries.
Pericardiocentesis- Description: This is a manner that entails extracting fluid for research with the useful resource of placing a needle into the pericardial hollow area. Function: Offers diagnostic facts through using analyzing the fluid to check for the lifestyles of maximum cancers, infections, or unique effusion-causing info. Additionally, it aids in strain consolation for cardiac tamponade sufferers.
Advanced Procedures
- Endomyocardial Biopsy: Description: Involves taking a biopsy of the heart tissue. Use: At times it can be used to track conditions affecting the heart, including inflammatory or invasive diseases.
- Electrocardiography (ECG): Description: Coronary The electrical pulses of the heart are recorded with the help of an electrocardiogram (ECG). Role: May assist in choosing out pericarditis signs and symptoms and signs and symptoms, further modifications in coronary heart rhythm.
It is regularly used as a complementary take a look at in place of a primary diagnostic device for pericardial vein troubles.
Summary of Diagnostic Approaches:
Clinical diagnosis: Initial diagnosis is mainly based on signs and symptoms and physical examination.
- Echocardiography: The main method for tracking cardiac output and results is echocardiography.
- Chest x-ray Initial assessment of fluid collections and cardiac imaging.
- CT and MRI: Evaluate for deep myocardial infarction, depression, stroke, or atherosclerosis.
- Laboratory diagnosis: Evaluation of underlying diseases and markers of inflammation.
- Pericardioscencesis: diagnosis and treatment, urine donation for research purposes.
- Advanced methods: Primary diagnostic biopsy.
- ECG: Another device used to measure and adjust heart rhythms.
These diagnostic tools and techniques help identify and manage issues in the extracardiac space that affect the circulation of the coronary arteries.
What are the treatment choices for pericardial vein-related conditions?
Since those conditions cannot directly impact the inclinations of the pericardial veins, treatment choices for pericardial vein-related conditions typically involve coping with issues affecting the pericardial area. Here is a radical examination of the remedies that are available for various pericardial vein-associated situations:
Pericardial Effusion
Management:
- Observation: For small, asymptomatic effusions, ordinary tracking with echocardiography can be enough.
Medication:
- Diuretics: These can be used to manipulate excessive fluid intake, specifically while coronary coronary heart failure is present.
- Antibiotics: For fever brought on by pericarditis or other inflammatory diseases.
Pericardiocentesis:
- Procedure: To remove extra fluid, a needle is inserted behind the heart.
- Goal: Enables diagnostic urine testing and relieves pressure in the event that flow results in symptoms or heart failure.
Surgical Options:
Pericardial Window: A drainage channel is established by making a tiny incision, which permits fluid to continuously enter the lungs.
Pericardiectomy: Surgical elimination of things or all of the pericardium can be taken into consideration in chronic or recurrent times
Cardiac Tamponade
Management:
Emergency Pericardiocentesis: Procedure: Rapid elimination of fluid from the pericardial area to relieve strain on the coronary heart and restore regular cardiac characteristics.
Treatment of Underlying Cause:
- Infections: Antibiotics or antivirals for infectious causes.
- Malignancy: Chemotherapy, radiation, or surgical interventions for cancer-associated tamponade
- Trauma: Surgical intervention to repair the supply of bleeding.
Constrictive Pericarditis
Management and Medication: Anti-inflammatory pills: To control underlying inflammation or infection. Diuretics: To alleviate signs and symptoms of fluid overload and decrease venous strain.
Surgical Treatment: Pericardiectomy: Removal of the thickened pericardial layer to alleviate constriction and improve heart filling.
Pericardial Cysts
Management:
- Observation: Small, asymptomatic cysts regularly need no remedy and are scrutinized with everyday imaging.
- Surgical Removal: Considered if the cyst is huge, symptomatic, or causing headaches.
Pericardial Tumors
Management:
- Surgical excision is the primary treatment for pericardial tumors, regardless of whether they may be malignant or benign. The intention of surgical procedure is to put off the tumor and any impacted tissue.
- Chemotherapy and radiation therapy can be used as the primary remedy for malignant tumors or in aggregate with surgical procedures if surgical operation isn’t an alternative.
Pericarditis
Management:
- Anti-inflammatory Medications:
- NSAIDs, or non-steroidal anti-inflammatory drugs, are frequently used to lessen pain and inflammation.
- Colchicine: You can upload colchicine to assist in lessening contamination and boost up your restoration.
- When therapy on my own is in vain, corticosteroids may be used for the duration of acute or present-day episodes.
- Purpose-Based Therapy:
- Infections: capsules or the proper drugs for infections.
- Autoimmune illnesses: Autoimmune sicknesses: Particular remedies for ailments like rheumatoid arthritis or lupus.
Pericardial Adhesions
Management:
- Medication: Antibiotics are used to lessen irritation and its associated signs.
- Surgical intervention: Surgery may be required to get rid of or decrease adhesions in extreme instances if they may be impairing coronary heart features.
An overview of to-be-had remedies:
- Pericardial Effusion: Observation, medications, pericardiocentesis, and surgical alternatives.
- Cardiac Tamponade: Emergency pericardiocentesis and restorative of the underlying cause.
- Constrictive Pericarditis: Anti-inflammatory medications and pericardiectomy.
- Pericardial Cysts: Observation or surgical elimination for symptomatic cases.
- Pericardial Tumors: Surgical elimination, and in all likelihood chemotherapy or radiation.
- Pericarditis: Corticosteroids, anti-inflammatory drugs, and treatments for underlying causes.
- Pericardial Adhesions: Medication to treat symptoms and indicators, as well as potential surgery.
These treatment options are intended to cope with each of the signs and symptoms and underlying reasons of disorders affecting the pericardial space and, via extension, the pericardial veins. The choice of treatment depends on the unique situation, its severity, and the patient’s universal fitness.
Are there surgical or clinical interventions available?
Yes, there are both surgical and medical interventions available for handling conditions related to the pericardial veins and pericardial area. Here’s a detailed overview of those interventions:
Medical Interventions
Medications
Anti-Inflammatory Drugs:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Used to lessen inflammation and aches in situations like pericarditis and pericardial effusion.
- Colchicine: Often used for pericarditis to lessen infection and prevent recurrence.
- Corticosteroids: Prescribed for severe instances of pericarditis or continual irritation, particularly whilst NSAIDs are insufficient.
- Diuretics:
- Purpose: Help manipulate fluid overload in conditions that include pericardial effusion or constrictive pericarditis through decreasing fluid buildup.
- Uses: May help reduce symptoms associated with fluid overload and muscle stiffness.
- Antibiotics/Antibiotics:
- Purpose: Treatment of underlying pathology causing pericarditis or pericardial effusion.
- Use Target unique infections based on simple lifestyle outcomes.
Drug/Radiation Therapy:
- Purpose: These treatments for cancer or tumors associated with malignancy are aimed at treating the underlying cancer.
- Use: Mainly given according to the kind and stage of cancer.
Antifibrotic drugs: Objective: An experimental or adjuvant approach to the management of fibrosis in constrictive pericarditis, to reduce scarring and increase cardiac function.
Surgical Interventions
Pericardiocentesis
- Description: A needle is placed behind the heart to remove excess fluid.
- Goal: Facilitates diagnostic fluid analysis and offers prompt release of pressure brought on either heart failure or pericardial effusion.
- Symptoms: Used in acute conditions to relieve symptoms and stabilize the patient.
Pericardial window
- Description: Surgery by opening a small opening in the pericardium to continuously drain fluid from the lungs.
- Purpose: The goal is to sustain or restore perfusion by providing extended perfusion.
- Indications: Used when pericardiocentesis is inadequate or when prolonged drainage is required.
Pericardiectomy resection
- Description: Surgical removal of part or all of the pericardium.
- Objective: Prevent pericardium thickening or fibrosis in constrictive pericarditis or chronic urinary tract infections.
- Indications: Considered in severe stable pericarditis, chronic pericardial effusion, or recurrent effusion unresponsive to other therapies
Surgical Removal of Pericardial Tumors
- Explanation: The Surgical resection of primary or metastatic tumors located in the pericardial space.
- Ambition: Seek to excise the tumor while minimizing its effects on heart function.
- Manifestation: For tumors that induce signs and symptoms or effects, each benign and malignant. Endomyocardial Biopsy
- Description: This process involves taking a small sample of heart muscle for analysis.
- Purpose: Helps diagnose precise situations affecting the pericardium or myocardium, along with infiltrative diseases.
- Indications: Used in instances in which a biopsy can provide important diagnostic statistics.
Summary of Interventions
Medical Interventions:
- Anti-Inflammatory Drugs: It is used For reducing infection and aches.
- Diuretics: To manage fluid overload.
- Antibiotics/Antivirals: To deal with infections.
- Chemotherapy/Radiation: For malignancy-associated troubles.
- Antifibrotic Agents: For experimental or supportive remedy.
Surgical Interventions:
- Pericardiocentesis: For instant fluid elimination and pressure relief.
- Pericardial Window: For extended drainage of fluid.
- Pericardiectomy: To relieve constriction and persistent effusion.
- Surgical Removal of Tumors: To cope with primary or metastatic pericardial tumors.
- Endomyocardial Biopsy: For unique analysis of infiltrative situations.
The preference among these scientific and surgical interventions relies upon the precise circumstance affecting the pericardial area, the severity of signs and symptoms, and the underlying causes. In many cases, an aggregate of treatments can be used to correctly manipulate and cope with the circumstance.
What are the implications of pericardial vein abnormalities on overall health?
Pericardial vein abnormalities may have enormous implications for universal health, more often than not due to the fact they may be regularly related to disorders that affect the pericardial area and, through extension, cardiac function. Here’s an outline of ways abnormalities within the pericardial veins can impact universal fitness:
Impact on Cardiac Function
Pressure at the Heart:
- Abnormalities such as pericardial effusion or cardiac tamponade can increase stress within the pericardial space. This strain can compress the heart, proscribing its capability to fill nicely at some stage in diastole (the rest section of the heart), which impairs cardiac output and usual coronary heart function.
- Symptoms: Due to decreased cardiac output, sufferers may additionally revel in exhaustion, shortness of breath, and decreased workout tolerance.
- Impaired Venous Return: One feature of the pericardial veins is to facilitate venous return to the coronary heart by way of emptying the pericardial region. Their characteristic may also be impacted by abnormalities, primarily due to congestion in the systemic venous system.
- Symptoms: This can result in jugular venous distension, peripheral edema, and symptoms of coronary heart failure.
Increased Risk of Heart Failure
Chronic Conditions:
- Conditions like constrictive pericarditis or persistent pericardial effusion can lead to chronic changes in the pericardium, which may affect the heart’s ability to function normally.
- Symptoms: As heart failure progresses, symptoms include dyspnoea, intolerance to physical activity, and oedema in the legs or belly.
Complications from Fluid Accumulation
Pericardial Effusion:
- Excess fluid accumulation in the pericardial space can cause cardiac tamponade, a lifestyle-threatening condition if no longer managed right away.
- Symptoms: Symptoms include excessive shortness of breath, chest pain, and immoderate blood stress, all of which require at once scientific attention.
Risk of infection or growth
- Infections: Infections that cause coronary heart irritation or bleeding can spread and cause systemic issues
- Symptoms encompass fever, chills, and dizziness. If left untreated, it can lead to deterioration of the fitness of the whole affected man or woman.
- Tumors: Primary or metastatic tumors within the heart region can have an effect on the heart muscle with the aid of obstructing or compressing muscle mass.
- Symptoms: Include indications and symptoms like weight loss, a chronic cough, and chest pain that are connected to tumor growth and metastasis.
Reduced Life Quality
Chronic Symptoms:
- Persistent or intense signs and symptoms from pericardial vein abnormalities, inclusive of chronic chest ache, dyspnea, or generalized fatigue, can appreciably impact someone’s high quality of existence.
- Management: Regular monitoring and treatment are necessary to reverse symptoms and improve quality of life.
- Possible medical emergency
Difficult circumstances:
- Sudden changes in an acute cardiac condition, including tachycardia or congestive heart failure, can rapidly deteriorate cardiac function and are of immediate scientific interest.
- Symptoms: May include severe chest pain, dyspnea, and high blood pressure, which will require immediate intervention to prevent serious consequences
Summary of Implications:
Cardiac Function:
- Pressure on Heart: Reduced cardiac output, impaired filling.
- Venous Return: Congestion, systemic symptoms of heart failure.
Heart Failure Risk: Heart failure signs and progression can result from continual sicknesses.
Fluid Accumulation Complications:
- Pericardial Effusion: Risk of cardiac tamponade and associated signs and symptoms.
Infection/Tumor Risks:
- Infections: Complications and systemic consequences of infections.
- Tumors: Blockage, unfold, and associated fitness troubles.
Quality of Life:– Persistent symptoms will have a huge effect on ordinary existence and popular health.
Acute Medical Emergencies:
Treatment for sudden deterioration will be essential right away to avoid the main repercussions. To keep popular fitness and health, control and therapy of pericardial vein anomalies usually center on treating the underlying issues affecting the pericardial region, easing symptoms, and warding off headaches.
Disclaimer:
The records approximately coronary heart costs are furnished completely for educational reasons and aren’t supposed for use as scientific advice. A licensed healthcare practitioner ought to continually be consulted before beginning the analysis and treatment of any scientific trouble. Individual exams and professional hints should be the muse for any remedy decisions, because the morphology and body shape of the myocardium may vary among individuals.
FAQs
What research is currently being conducted on the pericardial vein?
Although pericardial vein research is limited, it often focuses on sophisticated imaging techniques and fluid management tactics and examines the vein’s role in disorders such as pericardial effusion and cardiac tamponade. Current efforts additionally explore its involvement in systemic venous congestion and cardiac characteristics, in addition to enhancements in diagnostic and treatment strategies for related pericardial issues.
Are there any anatomical variations in the pericardial vein among individuals?
Anatomical interpretations within the pericardial vein are rare and no longer properly documented. Most interpretations are related to the presence of additional or variant venous channels within the pericardial vicinity in priority to good-sized deviations inside the pericardial veins themselves. As with neural networks, definitions are mostly found in related fields.
Are there any preventive measures for maintaining healthful pericardial veins?
Maintaining average cardiovascular health is crucial. This encompasses dealing with threat factors, including excessive blood pressure, diabetes, and LDL cholesterol. Frequent check-America with a fitness care provider also can help pick out viable issues and address them before they emerge as widespread problems.
What research is being done on pericardial veins?
The present study seeks to understand the broader consequences of the extracardiac space and its interaction with the heart. Conditions affecting the outer sac of the heart and its supply vessels are being identified to improve diagnostic and therapeutic strategies.
How do pericardial veins vary from coronary veins?
While coronary veins at once drain the myocardium, or coronary heart muscle, pericardial veins largely drain the pericardial sac and surrounding systems. Though they play different tasks and have different locations within the architecture of the heart, both systems are essential for cardiovascular health.
Can lifestyle changes impact the health of pericardial veins?
Overall cardiovascular fitness can be more advantageous via living a coronary heart-healthful way of life, even though there aren’t always a lot of records to help direct lifestyle influences on pericardial veins. A balanced weight-discount method, everyday schooling, and abstaining from smoking all contribute to the overall fitness of cardiac function.