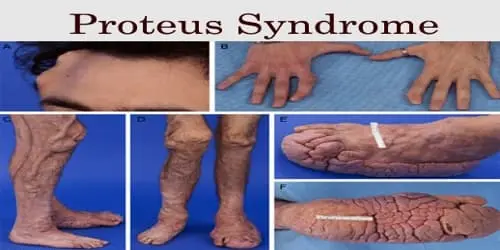
Proteus syndrome
What is Proteus syndrome?
Proteus syndrome is a rare genetic disease that causes extreme growth of your skin, bones, organs, and/or tissues. The condition causes parts of your body to expand out of proportion with the rest of it. The overgrowth is generally asymmetrical, suggesting it involves the right and left sides of your body differently.
Newborn infants with Proteus syndrome generally don’t display any signs of the disease. The atypical growth begins to seem between the ages of 6 months and 18 months. It rapidly grows within 10 years and gets more extreme as you age. Along with differences in physical appearance, some patients with Proteus may feel neurological problems. Patients with Proteus syndrome also have a raised risk of forming blood clots and tumors.
Proteus was the Ancient Greek god of transformation. Scientists named the disease Proteus syndrome because it can generate your body structures to transform shapes over time.
What are the signs and symptoms of Proteus syndrome?
Every person defined with Proteus syndrome presents just differently, but the characteristics defined below happen in many of them.
Abnormal bone and soft tissue growth
Overgrowth of digits (fingers and toes), limbs, and skull. Overgrowth is generally unnecessary and asymmetric.
Scoliosis (curvature of the spine) from abnormal vertebral development
Unnecessary overgrowth and focal atrophy (wasting away) of the upper arm muscles and neck, conducting to the hunched-over look
Abnormal skin and connective tissue growth
Raised irregular skin (verrucous epidermal naevi) or a flat, soft type of epidermal naevi
Deep lines and overgrowth of soft tissue on the soles of the feet or posterior part of the feet (cerebriform connective tissue naevi)
Local overgrowth of fat (lipomas) or invasive lipomas that create big intra-abdominal or intrathoracic lesions that can be medically hazardous
Abnormal development of blood or lymphatic vessels (vascular malformations) can develop vascular lesions like port wine stains or lymphatic malformations.
Cafe au lait macules are frequently present
Common facial features contain:
- Prominent occiput (enlarged back of the head)
- Drooping eyelids
- Low nasal bridge and wide, upturned nostrils
- Long, narrow face
- Open mouth at rest
Internal organs involved contain the spleen and thymus, which can evolve enlarged. The disease also generates quite important physical disfigurement and understanding of disabilities or developmental delays. Affected patients are prone to blood clots (thrombosis, embolus).
Causes of Proteus syndrome
Proteus syndrome happens during fetal development. It’s generated by what specialists call a mutation, or permanent alteration, of the gene AKT1. The AKT1 gene assists control of growth.
No one knows why this mutation happens, but doctors or physicians doubt it’s spontaneous and not inherited. For this cause, Proteus syndrome is a condition that is passed on from one generation to the following. The Proteus Syndrome Foundation emphasizes that this disease isn’t caused by something a parent did or didn’t do.
Scientists have also found that the gene mutation is mosaic. That suggests it involves some cells in the body but not others. This assists to describe why one side of the body may be involved and not the further, and why the severity of symptoms can differ so significantly from one patient to another.
Differential diagnosis
- Macrodystrophia lipomatosis
- Fibrolipomatous hamartoma
- Neurofibromatosis type 1
- Klippel-Trnaunay syndrome
- Parkes Weber syndrome
- Sotos syndrome
- Hemangiomas
How is Proteus syndrome diagnosed?
Your healthcare provider will conduct a physical examination to analyze Proteus syndrome. They’ll use a precise checklist of features of the disease. Three general characteristics of the condition must be present for your provider to assess the diagnosis. These contain:
Mosaic distribution: Mosaic allotment indicates the locations of extreme growth on your body are patchy. Somebody regions show signs of overgrowth and further don’t.
Sporadic occurrence: Sporadic event indicates no one in your family has features of the disease.
Progressive course: Progressive course indicates that overgrowth has altered the look of your involved body regions, especially over time.
In addition, your healthcare provider will look at further precise features. You must have precise characteristics from per category on your provider’s checklist for them to analyze you with Proteus syndrome.
Tests
The genetic mutation that generates Proteus syndrome isn’t present in every cell in your body. This can create genetic testing difficult because a blood sample may not include the mutation or only include small traces of it.
Yet, healthcare providers can see the mutated gene via DNA testing of a biopsy of some of your involved tissue. They’ll use DNA from the specimen to examine for the mutated gene.
Treatment of Proteus syndrome
There’s no treatment for Proteus syndrome. Treatment commonly concentrates on minimizing and controlling symptoms.
The disease involves many regions of the body, so your child may require treatment from several doctors, involving the following:
- cardiologist
- dermatologist
- pulmonologist (lung specialist)
- orthopedist (bone doctor)
- physical therapist
- psychiatrist
Surgery to extract skin overgrowths and extra tissue may be suggested. Doctors may also recommend surgically extracting growth plates in the bone to control extreme growth.
Complications of this syndrome
Proteus syndrome can generate numerous difficulties. Some can be life-threatening.
Your kid may develop large masses. These can be disfiguring and lead to extreme mobility issues. Tumors can squeeze organs and nerves, resulting in something such as a collapsed lung and loss of feeling in a limb. Overgrowth of bone can also conduct to loss of mobility.
The developments can also induce neurological difficulties that may involve mental growth, and conduct to loss of vision and seizures.
Patients with Proteus syndrome are more prone to deep vein thrombosis because it can involve blood vessels. Deep vein thrombosis is a blood clot that happens in the body’s deep veins, generally in the leg. The clot can break free and travel around the body.
If a clot evolves wedged in an artery of the lungs, known as a pulmonary embolism, it can block blood flow and lead to death. Pulmonary embolism is a leading reason of death in a patient with Proteus syndrome. Your kid will regularly be observed for blood clots. Familiar symptoms of a pulmonary embolism are:
- shortness of breath
- chest pain
- a cough that can occasionally bring up blood-streaked mucus
FAQ
How long can you live with Proteus syndrome?
Most persons have normal neuro psychomotor growth, with a life expectancy between 9 months and 29 years, according to the severity and site of the abnormalities.
Who usually gets Proteus syndrome?
Classically, men have been considered to be more generally involved than women, but new investigations with genetically verified patients have not yet been posted. The genetic mutation that generates Proteus Syndrome is a somatic mutation that happens after conception and is reproduced in one or more subsets of embryonic cells.
What antibiotic kills Proteus?
The tested antibiotics contained: ceftriaxone, nitrofurantoin, ciprofloxacin, and gentamicin. Of them, ciprofloxacin offered the most increased activity. Up to a 93% decrease in biofilm, construction was performed using a concentration of ciprofloxacin corresponding to 1/2MIC.
Is Proteus infection serious?
Proteus is seen abundantly in soil and water, and although it is a portion of the normal human intestinal flora (along with Klebsiella species, and Escherichia coli), it has been known to generate severe illnesses in humans.
What is the lifespan of someone with Proteus syndrome?
Life longing is 9 months to 29 years, according to the severity of the irregularities. The fourth leading reason for premature death is pulmonary thromboembolism and respiratory failure, which are predisposed by surgical convalescence, vascular malformations, and (in severe patients of deformity) limited mobility.