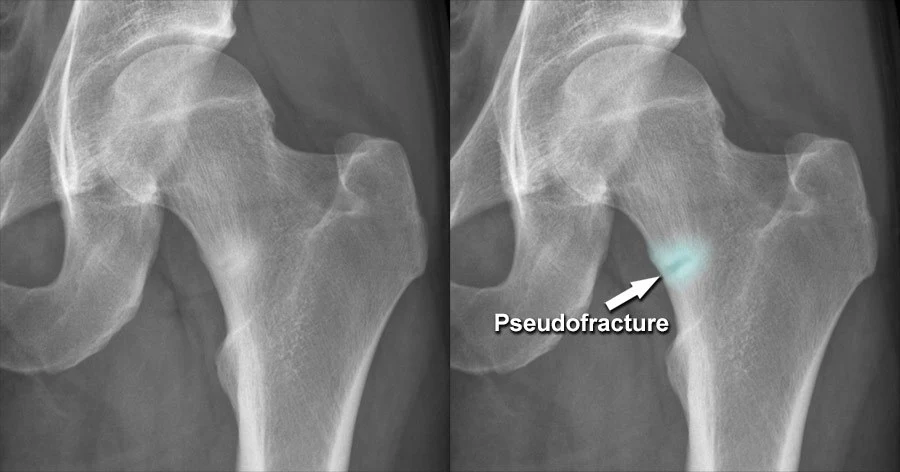
Pseudo Fracture
What is a Pseudo Fracture?
Pseudo fracture is typically an impression of a fake fracture in the bone. Alongside the surface of the cortical bone, a strip of less dense bone material is developing as the periosteum thickens. It is typical for calluses to form in the afflicted area, giving the impression that there has been a fake fracture.
The most common conditions linked with looser zones include osteomalacia and rickets. Looser zones are large horizontal areas with sclerotic boundaries that cross portions of the bone. They are also known as cortical lesions, Milkman’s lines, or pseudo clefts. The Looser Zone is named after Emil Looser, a Swiss physician.
Paget’s disease of the bones, hyperparathyroidism, renal osteodystrophy, osteogenesis imperfecta, fibrous dysplasia, and hypophosphatasia are some uncommon conditions that can result in pseudofracture.
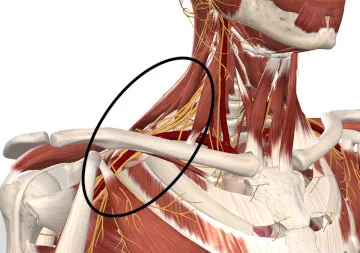
These lesions are not osteomalacia diagnostic in and of themselves because they represent a form of insufficiency fracture. When they are bilaterally symmetric and in a traditional site, such as the axillary border of the scapula, rib, or posterior ulna, osteomalacia is the strongly preferred diagnosis. The medial aspect of the femoral neck and the superior and inferior pubic rami are additional often implicated locations. These vulnerable spots may become completely fractured.
History
In honor of Swiss surgeon Emil Looser (1877–1936), who practiced in Zurich, looser zones were created.
American radiologist Louis Arthur Milkman (1895–1951) wrote about the discoveries in landmark publications published in 1930 and 1934.
Pathology
Because of the presence of hyperparathyroidism, looser zones typically have areas of demineralized osteoid and osteitis fibrosa cystica overlaid.
Location
In weight-bearing bones, looser zones appear when insufficiency fractures do:
- Rectal ramus
- Femoral neck medial
Referring to fractures in the lateral cortex of the proximal femoral shaft that is connected to bisphosphonates, the medial proximal femoral shaft–
They frequently happen along nutrient foramina in non-weight-bearing bones and are real pseudofractures:
- Sideways scapula
- Proximal posterior ulna
- Rib
- Wing of Iliac
Structure
Along the bone’s surface, a ring of less dense bone material may develop. The periosteum becomes thicker. In the impacted area, calluses are frequently formed. There appears to be a fake fracture as a result. The axillary borders of the scapula, the ribs, the pubic rami, the proximal ends of the femur, and the ulna are typical sites of involvement.
Causes of Pseudo Fracture
- Congenital abnormalities (anatomical variations)
- Osteomalacia
- Renal osteodystrophy
- Fibrous dysplasia
- Hyperthyroidism
- Paget disease of bone
- X-linked hypophosphatemia
- Osteogenesis imperfecta
- Hypophosphatasia
- Child development results (growth plates, ossification centers): a need for comparison
- Older patients’ degenerative conditions, old trauma
- Foramina of the nutrient artery
- Artifacts of imaging (such as the Mach band next to overlapping bones)
- Improper or poor posture
How does a person know if they have a pseudofracture?
If you feel any pain, bruising, swelling, or discomfort around your bones, call your doctor right once. Pseudofractures may result in discomfort that improves with rest and gets worse with routine everyday activity.
Wherever you are experiencing pain or discomfort, your doctor will set up an X-ray. This kind of picture will reveal pseudofractures.
While pseudo fractures do not necessitate immediate surgical intervention like true fractures, their proper identification is essential to avoid unnecessary treatments and interventions. The challenge lies in distinguishing them from true fractures, as misdiagnosis can have significant consequences for the patient.
Pseudofracture in osteomalacia
In osteomalacia, a pseudofracture, also known as a Looser zone, is a diagnostic feature.
Because osteomalacia can appear with several clinical and radiographic signs that resemble those of other musculoskeletal illnesses, it is frequently ignored. It is a recognized factor in the occurrence of chronic, vague musculoskeletal discomfort. Patients with osteomalacia can present with diffuse pain that may mislead to be diagnosed as fibromyalgia. Patients with osteomalacia on bone biopsies have a pseudofracture image on radionuclide scans accompanied by regional or systemic pain.
The mechanical stress of the great vessels located on the uncalcified cortical bone of the osteogenic bone is thought to be the determining factor in the location of the pseudo-symmetric fractures. “Pseudo-cracks” usually appear as rare horizontal regions, 1 mm to 1 cm in width. They are numerous and often symmetrically distributed, often occurring in apparently normal bones. Their distribution is mainly in the waist-pubic, iliac-pubic, femur, tibia, radius, fibula, or at the level of the pelvis.
Other common sites are the lower ribs and the subdural area of the shoulder blades.
Treatment
Treatment of pseudo fractures involves addressing the underlying condition responsible for their formation. For example, in cases of osteomalacia, correcting the deficiency of vitamin D, calcium, or phosphate through supplements and dietary changes can help. In the case of renal osteodystrophy, managing the underlying kidney disease and maintaining proper mineral balance are essential.
It’s important to consult with a qualified healthcare professional for an accurate diagnosis and appropriate management if you suspect you may have a pseudo fracture or any related medical condition.
Summary
The pseudo fracture may affect the entire skeletal system and affects both long and flat bones. Although solitary lesions may be discovered, it typically affects paired bones in advanced cases in a more or less symmetrical manner. The flaws are different from genuine fractures in a number of ways. They seem to form on their own without severe stress, but severe trauma may cause them to become actual fractures. A patient and therapist need to understand the details about pseudo fractures which are given in above article.
FAQs
What is a pseudo fracture?
With the periosteum thickening, a strip of less dense bone material is formed along the cortical bone’s surface. It is typical for calluses to form in the affected area, which mimics the appearance of a fracture.
What causes a pseudofracture?
Pseudofractures are described as small, radiolucent cortical abnormalities that can be bilateral or multilocular and are present in patients with severe osteomalacia, whether the condition is inherited (e.g., X-linked hypophosphatemia) or acquired. They can also be present in patients with severe vitamin D deficiency.
What is another name for pseudofracture?
Looser zones are also another name for pseudofractures. Osteomalacia and rickets are the two disorders that are most frequently linked to looser zones. Looser zones are broad, transverse lucencies with sclerotic borders that extend halfway through a bone. They are also known as cortical infractions, Milkman lines, or pseudofractures.
Where does pseudo fracture occurs?
The pubic rami, the medial part of the femur’s neck, the iliac bones, the radii, and the ulnae are where these pseudofractures are most frequently observed. All these are the most common sites for pseudo fracture and it can convert into true fracture if not taken care of.
What are pseudofractures in osteomalacia?
The most common conditions associated with looser zones include osteomalacia and rickets. Looser zones are broad, transverse lucencies with sclerotic borders that extend halfway through a bone. They are also known as cortical infractions, Milkman lines, or pseudofractures.



One Comment