Spasticity Treatment in Hemiplegia : Physiotherapy Treatment, Exercise
Introduction :
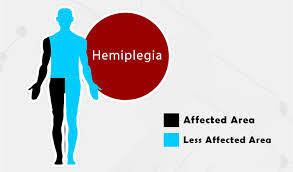
- Spastic Hemiplegia (hem-uh-PLEE-jee-uh) is paralysis with increase muscle tone that affects the motor function of one side of the body.
Definition of Spastic Hemiplegia :-
- Spastic Hemiplegia is a condition caused by mostly brain damage or spinal cord injury that leads to paralysis on one side of the body.
- It causes weakness, with loss of movement control, and muscle tightness and Difficulty in walking and performing day to day activity.
- The degree of hemiplegia symptoms vary depending on the location and type of the injury.
- If hemiplegia occur before birth, during birth, or within the first 2 years of life, it is known as congenital hemiplegia. If hemiplegia develops later in life, it’s known as acquired hemiplegia. Hemiplegia is a non-progressive.
Causes of Spastic hemiplegia :-
Stroke:-
- Strokes are one of the most ordinary causes of hemiplegia. The severity of muscle weakness is depend on the size and location of a stroke. Strokes in the womb are the most common cause of hemiplegia in children. Spastic hemiplegia occurs either at birth or in the womb.
Brain infections:-
- A brain infection like meningitis, multiple sclerosis, and encephalitis can cause permanent damage to the cortex of the brain.
- Most infections are caused by bacteria, but other infections may also be viral or fungal.
Brain trauma:-
- A sudden violent contact or strike to your head can cause permanent damage to your brain. If the trauma only affects one side of your brain, hemiplegia can develop.
- Common causes of trauma include car collisions, sports injury, explosive blasts and other combat injuries and assaults.
Genetics:-
- Very rare mutation of the ATP1A3 gene can cause a condition known as alternating hemiplegia in children.
- It causes temporary weakness on one side of the body that come and go. This disorder affects about 1 in 1 million people.
Brain tumor:-
- Brain tumors can lead to a variety of physical problems including hemiplegia.
- it’s symptoms may get worse as the tumor grows in the brain.
Mechanism of Spasticity :-
- Damage to the Corticospinal Tract cause the injury on the opposite side of the body.
- This happens because the motor fibers of the Corticospinal Tract , which take origin from the motor cortex of the brain , cross to the opposite side in the lower part of medulla oblongata and then descend down in spinal cord to supply their respective muscles.
Depending on the Site of lesion in brain , the severity of hemiplegia varies :-
| Site of lesion | Signs and symptoms |
| Internal capsule | Dense and uniform Hemiplegia Hemisensory blunting Homonymous hemianopia |
| Cortex | Non dense non uniform weakness Monoplegia Cortical signs ( Dysphasia , Apraxia , Cortical sensory loss , Convulsions ) |
| Sub cortex | Pattern of weakness similar to cortical |
| Brainstem | Crossed hemiplegia Ipsilateral LMN cranial nerve Palsy and contralateral hemiplegia Cerebellar signs. |
| Midbrain | Crossed cerebellar ataxia with Ipsilateral Third nerve palsy ( Claude’s Syndrome ) Weber’s syndrome – Third nerve palsy and contralateral hemiplegia Contralateral hemiplegia – Cerebral peduncle Contralateral rhythmic , ataxic action tremor ; rhythmic postural or holding tremor (rubral tremor) |
| Pons | LMN Facial and contralateral hemiplegia Fifth nerve and contralateral hemiplegia Lateral Gaze palsy and contralateral hemiplegia |
| Medulla- Lateral medullary Syndrome | Same side ( Horner’s Syndrome , Loss of pain and touch on the face , Cerebellar signs , Palate weakness ) Opposite side ( Loss of pain and temperature sensation on the body and limbs ) |
| Medulla- Medial medullary Syndrome | Same side ( wasting and weakness of the tongue ) Opposite side ( hemiplegia without facial palsy ) |
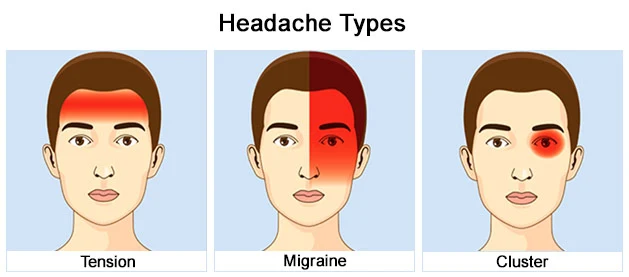
Spastic hemiplegia symptoms :-
- Hemiplegia can affect either the left or right side of your body. Whichever side of your brain is affected causes symptoms on the opposite side of your body.
- People can have different symptoms from hemiplegia depending on its severity.
Symptoms can include:
- muscle weakness or stiffness on one side
- muscle spasticity or permanently contracted muscle
- muscle tightness
- poor fine motor skills
- Difficulty in walking
- poor balance
- Difficulty in grabbing objects
What is the Major Difference Between Spastic Hemiplegia and Hemiparesis?
- The primary difference in the spastic hemiplegia vs. hemiparesis debate for most people is symptom severity.
- Spastic Hemiplegia often causes complete paralysis on one side of the body with spasticity, while hemiparesis only creates muscle weakness or partial paralysis.
Examination:-
- The selection of examination procedures will vary based upon a number of factors including patient age ,location and severity of stroke , stage of recovery , data from initial screenings , phase of rehabilitation and home /community / work situation , as well as other factors.
General examination :-
General appearance including posture , motor activity :
Vital signs :-
- Level of consciousness
- pulse
- BP
- look for pupil size
- conjugate deviations of eyes
- Meningeal signs.
Neurocutaneous markers-
- Neurofibroma over the skin ( may have associated Tuberous sclerosis of brain )
- Sebaceous adenoma
- Sturge Weber Syndrome – facial nerve (port wine stain ) involving one half of face with upper eyelid – associated with atrophy and calcification of ipsilateral cerebral hemisphere and increased pressure in the eye (glaucoma).
- Lymphadenopathy
- Cyanosis ( a bluish discoloration of the skin)
- Clubbing ( an abnormal, rounded shape of the nail bed)
- Shortening of limb (hemiplegic side ) – indicates it is dating from early childhood
- Irregular pulse of atrial fibrillation
Higher examination :-
1. Consciousness
| Behavior | Response | Score |
| Eye opening response | Spontaneously To speech To pain No response | 4 3 2 1 |
| Best verbal response | Oriented to time, place, and person Confused Inappropriate words Incomprehensible words No response | 5 4 3 2 1 |
| Best motor response | Obeys commands Moves to Localized pain Flexion withdrawal from pain Abnormal flexion (decorticate) Abnormal Extension (decerebrate) No response | 6 5 4 3 2 1 |
| Total score | Best response Comatose client Totally unresponsive | 15 8 or less 3 |
2. Orientation
- In time , person , space , place are tested.
3. Memory
- It includes Immediate memory , short term memory , long term memory.
- Check with family or friends of the patient if he is right.
4. Intelligence
5. Speech
- Speech disturbances APHASIA (inability to understand or produce speech) may occur
6. Emotion
- Anxious / depressed / elated / mood swings
7. Judgment
8. Behaviour
9. Presence of hallucination/ illusion
- hallucination :- An experience involving the apparent perception of something not present.
- illusion :- An instance of a wrong or misinterpreted perception of a sensory experience.
Sensation :-
- Sensory integration is the ability of the brain to organise , interpret , and use sensory information .
- Examination of sensory function involves testing patient’s ability to interpret and discriminate among incoming sensory information.
| Pattern of sensory loss | Site of lesion |
| 1. Mono-neural | Peripheral nerve |
| 2. Stock and glove | |
| 3. Maculo-anesthetic (leprosy) | |
| 4. Radicular sensory loss | Root |
| 5. Saddle area loss | Conus |
| 6. Dissociated sensory loss (Brown-Squared Syndrome) joint position / vibration / light touch on same side and pain / temperature on opposite side | Unilateral cord lesion |
| 7. Sensory level | Extra-medullary lesion |
| 8. Jacket sensory loss (dissociated) | Intra-medullary lesion |
| 9. Crossed hemihyposthesia | Lateral medullary Syndrome |
| 10. Hemi-hyposthesia | Capsular & brain stem lesions |
| 11. Corticalsensory loss numbness , agnosia , loss of two point discrimination , astereognosis , graphanaesthesia ,sensory inattention | Area(1, 2, 3) of parietal lobe |
Motor function :-
Tone :-
An examination of tone is essential . Passive motion testing can be done to determine the presence
of hypertonicity or spasticity. Severity of spasticity can be graded on the basis of resistance to passive
stretch using the Modified Asthworth Scale.
Modified Ashworth Scale :
| Scale No | Spasticity Description |
| 0 | Normal Muscle Tome |
| 1 | Slight increase of Muscle tone / Catch – release at the End of ROM |
| 1+ | Slight more increase of Muscle tome / Catch – release at the mid to End ROM (1/2 ROM) |
| 2 | More Marked increase muscle tone through ROM / But affected part moved easily. |
| 3 | Considerable increase in muscle tone, Passive movement difficult |
| 4 | Affected part in rigid flexion / Extension with Passive movement is too Hard. |
Stage of flaccid paralysis:-
- this stage is called shock stage . It lasts from 2 to 6 weeks , the shorter the duration better the prognosis.
- On the paralysed side there is complete loss of muscle tone (flaccidity) , absence of deep reflexes and no plantar reflex.
- This stage is prolonged by general poor condition of the patients health , infection in the chest and urinary tract infection and bed sores.
- During recovery from the shock stage ,tone of the muscle and deep reflexes reappear and gradually increase.
- Babinski sign becomes positive .
- The stage of spasticity sets in. If the onset is associated with coma , the paralysed side is determined by the following :
- The limb on the side of paralysis are more flaccid and drop passively.
- The cheek on the side of paralysis moves in and out with respiration.
Stage of flaccid paralysis :- Stage of established hemiplegia where there is :
1. Paralysis of one side of the body :
- This paralysis shows a pyramidal distribution .
It affects the pro-gravity muscles more than the anti-gravity muscles as the former are normally weaker than the latter.
- In upper limb , the extensors are weaker than the flexors.
- In lower limb, the flexors are weaker than the extensors.
It affects the distal more than the proximal muscles.
- The hand is weaker than the shoulder.
- The foot is weaker than the hip.
2. Hypertonia (spasticity) of the paralysed muscle of clasp knife :
It affects the anti-gravity more than the pro-gravity muscles as the former normally have a stronger
muscle tone :
- In upper limb, the flexors are more spastic than the extensors.
- In lower limb , the extensors are more spastic than the flexors.
Clonus –
Series of involuntary and rhythmical muscle contraction occurring in response to maintenance of tension in muscle tone .
It is due to gamma neuronal discharge. Sustained clonus is a sign of the pyramidal Tract lesion.
Reflexes :-
- Reflexes are altered and also vary according to the stage of recovery .
- Initially , stroke result in hyporeflexia with flaccidity .
- When spasticity and synergy emerges , hyperreflexia is seen .
- Deep tendon reflexes are hyperactive and patient may demonstrate clonus , clasp-knife response and positive Babinski , all consistent finding of upper motor neuron Syndrome.
- There are certain pathological reflexes looked for in hemiplegia .
- In upper limb clinically significant – if markedly active and asymmetrical are Hoffman’s sign , Wartenberg’s sign .
- Superficial reflexes in hemiplegia are loss of Abdominal reflex and cremastric reflex which is a sign of upper motor neuron Lesion .
Voluntary movements :-
- Abnormal and highly stereotyped obligatory synergies emerge with spasticity following stroke .
- Thus the patient is unable to perform an isolated movements of a single limb segment without producing movements in the remainder of the limb.
- Two distinct abnormal synergy patterns have been described for each extremity : flexion and extension synergy.
Obligatory Synergy Patterns Following Stroke :-
| Flexion Synergy Components | Extension Synergy Components | |
| Upper extremity | Scapular retraction/elevation or hyperextension Shoulder abduction, external rotation Elbow flexion Forearm supination Wrist and finger flexion | Scapular protraction Shoulder adduction, internal rotation Elbow extension Forearm pronation Wrist and finger flexion |
| Lower extremity | Hip flexion, abduction, external rotation Knee flexion Ankle dorsiflexion, inversion Toe dorsiflexion | Hip extension, adduction, internal rotation Knee extension Ankle plantar-flexion, inversion Toe planter flexion |
Spastic Hemiplegia Treatment :-
Aims :-
- Prevent recurrent stroke
2. Monitor vital signs, dysphasia adequate nutrition, bladder & bowel function.
3. Prevent complications
4. Mobilize the patient
5. Encourage resumption of self-care activities
6. Provide emotional support & education for patient & family
7. Screen for rehabilitation and choice of settings
8. regain independence
9. Reduce spasticity
Following are the Primary treatment protocol started from day one :
- Care of the skin
- Frequent changes of the patient’s position in every 2 hours and of the bed sheets.
- Frequent wash of the skin of the back and pressure points by alcohol followed by talc powder.
2. Care of respiration
- Suction of nasal and pharyngeal secretions.
- Oxygen inhalation via catheter or mask specially in cases of coma.
- Tracheostomy in urgent cases.
- Breathing exercises
- Chest expansion exercise
- Huffing and coughing technique to remove the secretions.
- Postural drainage
3. Care of nutrition and fluid balance
- Tube feeding giving fruit juices , milk and pureed food , besides I.V. Fluids , in comatosed patients.
4. Care of urinary bladder
- Foley’s self retaining catheter in case of retention or incontinence.
- Urinary antiseptics : Gentamycin 80 mg I.M . every 12 hours.
- Care of bowels : Daily enema.
5. Prevent from deconditioning
- Early bed activity (active rolling or turning, supine to sit, sit to supine, sitting, sit to stand)
- Pelvic bridging exercise
- Early propped up positioning, sitting then progress to standing
- Moving around the bed
- Facilitate movement of functioning limbs
- passive ROM exercise
once the patient’s condition is stable then he is made to move out of the hospital bed and attends the
Rehabilitation therapy clinic of the concerned Hospital or is referred to such clinics outside.
6. Reduce spasticity

- Cryotherapy is one of the most commonly used interventions by physical therapist to reduce spasticity.
- ice cube stroking and ice massage can reduce spasticity to spastic muscles.
- cooling and sustained passive stretching as treatment techniques for reduction of spasticity in hemiplegics using H- reflex.
Rehabilitation :-
- Stroke rehabilitation begins almost immediately, preferably within 24-36 hours once a patient is found medically stable.
- The Physiotherapist focuses on joint range of motion and strength by performing exercises and re-learning functional tasks such as bed mobility, transferring from bed to chair or one place to another place, walking and other gross motor functions.
- Physiotherapists can also work with patients to improve awareness and use of the hemiplegic side.
- Rehabilitation involves working on the ability to produce strong movements or the ability to perform tasks using normal patterns.
- Emphasis is often concentrated on functional tasks and patient’s goals.
- One example physiotherapists employ to promote motor learning involves constraint-induced movement therapy.
- Through continuous practice the patient relearns to use and adapt the hemiplegic limb during functional activities to create lasting permanent changes.
Physiotherapy Treatment :-
A. Conventional therapies (Therapeutic Exercises,Traditional Functional Retraining) :-
- Range Of Motion (ROM) Exercises
- Streching of tight muscles
- Muscle Strengthening Exercises
- Mobilization activities
- Fitness training
- Compensatory Techniques
B. Neurophysiological Approaches :-
- Muscle Re-education Approach.
- Neurodevelopmental Approaches :Neurology Treatment Techniques Sensorimotor Approach (Rood, 1940S) Movement Therapy Approach (Brunnstrom, 1950S)
- NDT Approach (Bobath, 1960-70S) PNF Approach (Knot and Voss,1960-70S)
- Motor Relearning Program for Stroke (1980S)
- Contemporary Task Oriented Approach (1990S)
Posture : Primary focus, Potential Treatment, Benefits , Activities :-
| Posture/description | Primary focus/benefits/activities |
| Prone on elbow Prone ,weight bearing on elbows Stable posture Wide BOS Low COM | Focus on improving upper trunk, UE and neck/head control Improve ROM in hip extension Improve shoulder stabilizers Activities in posture : holding , weight shifting , UE reaching , assumption of posture Modified prone on elbows can be achieved in sitting and plantigrade positions |
| Quadruped All four positions (hands and knees) Weight bearing at knees through extended elbows and hands Stable posture Wide BOS Low COM | Focus on improving trunk , LE , UE and neck/head control Improve trunk , hip , shoulder and elbow stabilizers Decrease extensor tone at knees by prolonged weight bearing Decrease flexor tone at wrist , elbows and hands by prolonged weight bearing Promote extensor ROM at elbows, wrist and fingers Lead up for I plantigrade activities , floor to standing transfers , anti gravity balance control Activities in posture : holding , weight shifting , UE reaching , LE lifts , assumption of posture , locomotion on all fours. |
| Bridging Weight bearing at feet and ankles , upper trunk Stable posture Wide BOS Low COM | Focus on improving lower trunk and LE control Improve hip and ankle strategies Weight bearing at feet and ankles Lead up for bed mobility , sit to stand transfers , standing and stair climbing Activities in posture : holding weight shifting , assumption of postures , LE lifts |
| Sitting Weight bearing through trunk and at buttocks , feet Can include weight bearing through extended elbows and on hands Intermediate BOS Intermediate height COM | Focus on improving upper trunk , lower trunk , LE and head/neck control Important for upright balance control Lead up for UE ADL skills ; wheelchair locomotion Activities in posture : holding , weight shifting , UE reaching , assumption of posture |
| Kneeling and half kneeling | Focus on improving upper trunk , lower trunk , LE and head/neck control Weight bearing through hips and at knees ; upright anti-grade position Decrease extensor tone at knee by prolonged weight bearing Improve hip and trunk stabilizers Weight bearing through ankle in half kneeling Lead up for upright balance control , standing and stepping , floor to standing transfers Activities in posture ; holding , weight shifting , UE reaching ,assumption of posture , knee walking |
| Modified plantigrade Standing with weight bearing on hands through extended elbows (on support surface) and through trunk, LEs Modified upright anti gravity position Wide BOS High COM | Focus on improving head/neck, trunk, and UE/LE control in supported, modified upright posture Decrease tone in elbow, wrist, and finger flexors by prolonged weight bearing Increase extensor ROM at elbows, wrists, and fingers Hips flexed, COM forward of weight bearing line creating an extension moment at the knee Increased safety for early standing (four-limb posture) Lead-up for upright balance control, standing and stepping; standing UE ADL tasks Activities in posture: holding, weight shifting, UE reaching, LE stepping, assumption of posture |
| Standing Weight bearing through trunk and LEs Full upright, anti gravity position Narrow BOS High COM | Focus on improving head/neck, trunk, and LE control in fully upright posture Hips and knees fully extended Lead-up for upright balance control, stepping, locomotion, stair climbing; standing UE ADL skills Activities in posture: holding, weight shifting, UE reaching, LE stepping, assumption of posture |
Gait training :-

- Conventional gait training has focused on part-practice of components of gait in preparation for walking.
It includes:
- Symmetrical Weight bearing training
- Weight shifting
- Stepping training (swinging / clearance )
- Heel strike
- Single leg standing
- Push off / Calf rise.
Followed by,
- Circuit training (reaching in sitting and standing, sit-to-stand, step-ups, step-downs, heel lifts, isokinetic strengthening, walking over obstacles, up and down slopes).
- Traditional approaches to stroke recovery have a focus on neuro facilitation or neuro developmental techniques (NDT) to inhibit excessive tone, stimulate muscle activity if hypotonia is present and to facilitate normal movement patterns through hands-on techniques. Practice based on the framework advocated by Berta Bobath remains the predominant physical therapy approach to stroke patients in the UK and is also common in many other parts of the world, including Canada, United States, Europe, Australia, Hong Kong and Taiwan.
- The Bobath framework has evolved from its original foundations, however, therapists surveyed on the core Bobath elements still emphasize normal tone and the necessity of normal movement patterns to perform functional tasks. Strength training to improve walking ability Task-specific training to improve walking ability.