HEMIPLEGIA
WHAT IS HEMIPLEGIA ?
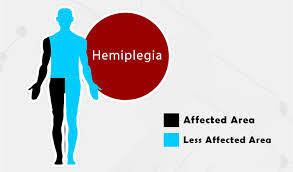
- Hemiplegia is a condition caused by brain damage and spinal cord injury that leads to paralysis on one side of the body. It causes paralysis of one side of body, with loss of movement control, and muscle tightness (Increase muscle tone).
- Hemiplegia is total paralysis of the arm,leg and trunk on the same side of the body .
- Severe or complete loss of motor function on one side of the body .
- Hemiplegia is more severe than hemiparesis, where in one half of body has less weakness.
- Hemiplegia may be congenital or acquired from an illness or stroke.
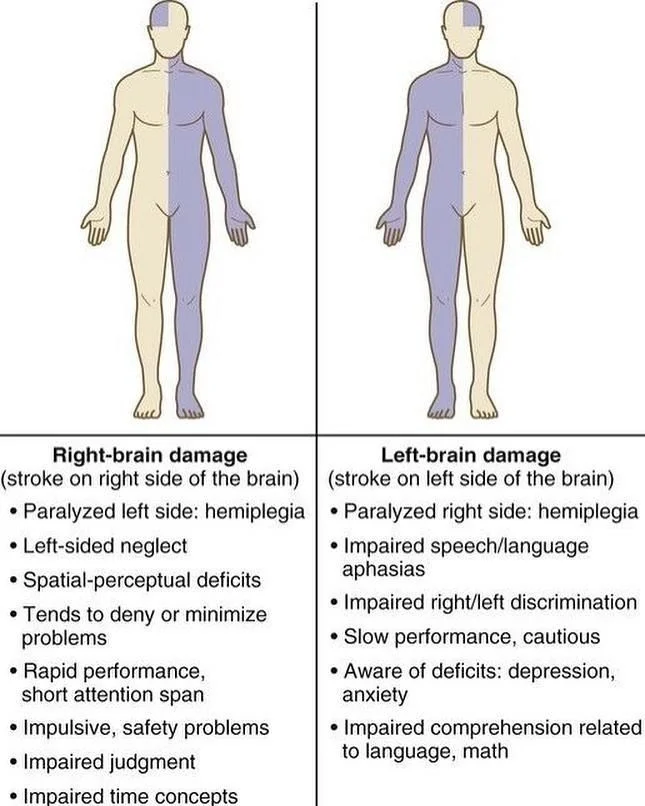
Right Hemiplegia vs Left Hemiplegia
- Left hemiplegia is the paralysis of limbs on the left side of the body, while right hemiplegia indicates paralysis on the right side of the body. Like hemiparesis, right or left hemiplegia may be caused by damage to the nervous system.
- One common cause of left or right hemiplegia is an incomplete spinal cord injury. In an incomplete SCI, only part of the spinal cord is severed, so there may still be some function below the injury site. For example, an incomplete spinal cord injury in the cervical spinal cord might paralyze the left side of the body while leaving the right side functional — though this isn’t guaranteed because the specific nerves severed may alter the effects of the injury.
WHAT ARE THE CAUSE OF HEMIPLEGIA?
Stroke
- Strokes and transient ischemic attacks one of the most common causes of hemiparesis,” which can develop into hemiplegia as symptoms worsen.
Brain and Nervous System Infections
- Infections, particularly encephalitis and meningitis. Some serious infections, particularly sepsis and abscesses in the neck, may spread to the brain if left untreated. This can not only cause hemiplegia, it can affect a person’s ability to think and even cause death.
Brain Trauma
- This includes traumatic brain injuries to one side of the brain. These TBIs may be caused by car accidents, falls, acts of violence, and other factors.
Genetic Disorders/Congenital Diseases
- Congenital abnormalities, including cerebral palsy and neonatal-onset multi-inflammatory disease. Genetic disorders can impact the development of the nervous system and lead to conditions like hemiplegia, paraplegia, or even quadriplegia.
Brain Tumors
- Cancerous growths in the brain can apply pressure to different parts of the brain required for motor control. Left unchecked, brain tumors can grow and make symptoms worse over time or even affect things other than muscle function.
Brain Lesions
- Lesions in the brain can cause hemiplegia or hemiparesis. This is because these lesions can impede function on one side of the brain. Lesions are areas of tissue in the brain that have been damaged by injury or disease. Sometimes, these get confused with brain tumors, but lesions are a bit different.
- What makes a lesion different from a tumor is that it typically will not keep growing on its own (unless repeated injuries occur at the site of the lesion because of strokes or infections).
Brain Diseases
- Brain diseases include conditions that cause demyelination of the brain, such as multiple sclerosis and some other autoimmune diseases. There are many brain diseases that may cause brain lesions or other issues that lead to hemiplegia or hemiparesis.
Psychological Conditions
- Rarely, psychological causes, such as some states of catatonia can cause hemiplegia. People with parasomnia—a sleep disorder leading to unusual nighttime behavior—may experience nighttime episodes of hemiplegia.
Cardiovascular Problems
- Cardiovascular problems, particularly aneurysms and hemorrhages in the brain, can lead to hemiplegia or hemiparesis.
Loss of Oxygen to the Brain
- A loss of oxygen to the brain due to choking, drowning, anaphylactic shock, or cardiovascular problems can result in permanent brain damage. This, in turn, may lead to hemiplegia.
Causes of Right-Sided Hemiplegia?
The causes of hemiplegia include neurological conditions such as:
- Cerebrovascular Accident (CVA)
- Thrombosis, Embolism, or hemorrhage
- Transient Ischemic Attack (TIA)
- Migraine syndrome
- Head Trauma
- Brain contusion
- Subdural Hematoma
- Epidural Hematoma
- Todd s paralysis
- Diabetes Mellitus
- Infection
- Subdural empyema
- Meningitis
- Vasculitis
- Hereditary disease
- Leukodystrophies
- Stroke
- Traumatic brain injury
- Cerebral palsy
- Degenerative disorders like Parkinson’s
- Brain cancer or brain lesions
TYPES OF HEMIPLEGIA
Facial Hemiplegia
- People with facial hemiplegia experience paralyzed muscles on one side of their face. Facial hemiplegia may also be coupled with a slight hemiplegia elsewhere in the body.
Spinal hemiplegia
- Spinal hemiplegia is also referred to as Brown- sequard syndrome It involves damage on one side of the spinal cord that results in paralysis on the same side of the body as the injury. It also causes loss of pain and temperature sensation on the opposite side of the body.
Contralateral hemiplegia
- This refers to paralysis on the opposite side of the body that brain damage occurs in.
Spastic hemiplegia
- This is a type of hemiplegia that predominately affects one side of the body. The muscles on the affected side are constantly contracted or spastic.
SYMPTOMS OF HEMIPLEGIA
Symptoms of hemiplegia include:
- Difficulty moving, or the inability to move, one side of the body.
- Difficulty with bowel or bladder control.
- Changes or loss in sensation on one side of the body.
- Keeping one hand in a fist.
- Difficulty swallowing or with speech.
- Breathing difficulties.
HEMIPLEGIA AND PARAPLEGIA DIFFERENCE
- There are three general types of paralysis: paraplegia, hemiplegia and quadriplegia. Paraplegia is paralysis of the legs and lower body resulting from injury to nerves in the areas of the lumbar or thoracic vertebrae. Hemiplegia is paralysis of one side of the body. The most common of brain injury, and spinal cord injury.
| NO | HEMIPLEGIA | PARAPLEGIA |
| 1 | There is paralysis of arm ,leg and trunk on one side of the body. | There is paralysis of lower segment of body including both lower limbs. |
| 2 | It occurs mainly due to brain damage. | It occurs mainly due to spinal cord injury. |
| 3 | There is motor function loss present. | There is both motor and sensory function loss present. |
| 4 | If there is only weakness present then it called hemiparesis. | If there is only weakness present then it called paraparesis. |
| 5 | Circumductory Gait in present | Absent |
| 6 | There is difficulty in hand function EXAMPLE : Grasping , Griping , Writing etc. | There is not difficulty in hand function. |
| 7 | Reflexes is exaggerated | Reflexes is exaggerated |
| 8 | Sudden loss of balance and co-ordination. | Sudden loss of balance and co-ordination. |
| 9 | Bowel and Bladder Dysfunction is present . | Bowel and Bladder Dysfunction is present . |
HEMIPLEGIA VERSUS HEMIPARESIS
Hemiparesis Definition
- Hemiparesis is weakness on half of the body. This may manifest in multiple ways, such as a loss of motor control, inability to feel one side of the body, or general sensations of weakness.
Right Hemiparesis vs Left Hemiparesis
- As the name implies, right hemiparesis is weakness on the right side of the body, while left hemiparesis is weakness on the left side of the body. What causes this weakness in one side of the body and not the other varies, but damage to the nervous system from injury, infection, or degenerative conditions can result in hemiparesis.
- In the case of degenerative conditions such as multiple sclerosis or amyotrophic lateral sclerosis (ALS), hemiparesis may progress into hemiplegia with time.
Symptoms of Hemiparesis
- Difficulties with motor skills, particularly standing.
- Weakness in large areas on one side of the body. For example, a patient might be unable to lift his or her arms.
- Pusher syndrome: a common byproduct of traumatic brain injuries, pusher syndrome causes a person with hemiparesis to shift their weight to the affected side, thereby undermining motor skills and making walking difficult and potentially painful. Doctors use a scale to assess the severity of pusher syndrome. This scale can help doctors make accurate prognostications, in addition to identifying the cause of symptoms.
- Strain on the unaffected side of the body, which may overcompensate for injuries on the hemiparetic side.
- Unusual sensations or tingling on the affected side.
Hemiplegia Definition
- Where hemiparesis indicates weakness on one side of the body, hemiplegia indicates partial or total paralysis instead. Because paralysis is an extreme form of weakness and nerve dysfunction, hemiplegia can be considered an extreme form of hemiparesis.
- Hemiplegia should not be confused with paraplegia , which is a condition that affects the lower body. However, the causes of hemiplegia and paraplegia are frequently similar.
Right Hemiplegia vs Left Hemiplegia
- Left hemiplegia is the paralysis of limbs on the left side of the body, while right hemiplegia indicates paralysis on the right side of the body. Like hemiparesis, right or left hemiplegia may be caused by damage to the nervous system.
- One common cause of left or right hemiplegia is an incomplete spinal cord injury. In an incomplete SCI, only part of the spinal cord is severed, so there may still be some function below the injury site. For example, an incomplete spinal cord injury in the cervical spinal cord might paralyze the left side of the body while leaving the right side functional — though this isn’t guaranteed because the specific nerves severed may alter the effects of the injury.
Symptoms of Hemiplegia
- Difficulty moving, or the inability to move, one side of the body.
- Difficulty with bowel or bladder control.
- Changes or loss in sensation on one side of the body.
- Keeping one hand in a fist.
- Difficulty swallowing or with speech.
- Breathing difficulties.
Hemiparesis and Hemiplegia Causes
- here are a number of conditions that can cause hemiparesis or hemiplegia. Examples of hemiparesis and hemiplegia causes include strokes, brain injuries, spinal cord injuries, infections, and a handful of other conditions affecting the central nervous system.
- Both hemiparesis and hemiplegia are nervous system disorders, not caused by injury to the affected side of the body. For example, an injury to the spinal cord or brain interferes with the body’s ability to send or receive signals to the region of the body affected by the injury. So, while the left or right side of the body haven’t been damaged directly, the spinal cord injury may cause hemiparesis or hemiplegia.
- The most common cause of both injuries is a stroke. Strokes interfere with blood flow to the brain. If a region of the brain that affects movement or perception is affected, hemiparesis or hemiplegia may develop. The affected region is usually the opposite of the side of the brain affected, so an injury to the right side of the brain will affect the left side of the body.
- Some other causes of hemiparesis and hemiplegia include:
- Brain infections such as meningitis or encephalitis
- Brain cancer or lesions
- Damage to the neurons due to a degenerative disorder such as Parkinson’s
- Traumatic injuries, such as a blow to the head during a car accident
- Congenital disorders such as cerebral palsy.
Hemiparesis vs Hemiplegia
- Hemiparesis and hemiplegia are part of the same continuum of central nervous system injuries. Both interfere with movement and sensation. Both can be difficult to treat, and often severely constrain normal functioning.
- Though the symptoms are different, the two conditions are essentially different versions of the same underlying problem. Mild to moderate nerve or brain damage will produce hemiparesis, while moderate to severe nerve or brain damage will result in hemiplegia. Moreover, the same injury can produce both symptoms at different times. This is especially true when nerves are compressed or the spinal cord is swollen, since changes in swelling or compression can also produce changes in symptoms.
- Particularly early in an injury’s course, it’s impossible to determine whether a patient will be left with hemiparesis or hemiplegia.
What’s the Difference Between Hemiparesis and Hemiplegia?
- Hemiparesis is characterized by weakness on one side of the body. A person with hemiparesis might not be able to move their arm, or may feel tingling or other odd sensations on just one side.
- Hemiplegia is paralysis on one side of the body. Though stereotypes of paralysis suggest that paralysis completely removes the ability to move, the reality is a bit more complicated. People with paralysis may retain some sensation, and the degree to which they are paralyzed can change over time. Thus it can be hard to establish a clear line that separates hemiparesis and hemiplegia, particularly in the case of mild hemiplegia and severe hemiparesis.
PHYSIOTHERAPY MANAGEMENT IN HEMIPLEGIA
General :
- n acute (shock ) stage of hemiplegia and in the comatosed patient.
- Treatment of the adult with Hemiplegia, following stroke starts from the very acute stage, when the patient in the ICU or Hospital bed.
- Treatment should be based on assessment by the relevant health professionals, including physiotherapists, Physicians and occupational therapists.
- Muscles with severe motor impairment including weakness need these therapists to assist them with specific exercises.
Weight-bearing help Reduce spasticity:
- Any weight bearing of the upper extremity either at the wall, table, or floor helps sends signals to the brain that reminds it the arm is still there.
- Strengthening can improve spasticity in two ways. By strengthening the antagonist (opposing) muscle, it can help inhibit the reaction of the spastic muscle.
Icing reduces spasticity :
- Efferent and afferent neurotransmission is reduced through prolonged use of ice,
- which is effective for the reduction of spasticity. In order to achieve this, the muscle spindles need to be cooled

- requiring that ice is applied until there is no longer an excessive reflex response to stretching.
Heat decrease spasticity :
- Sometimes heat or ice can be used to temporarily relax a spastic muscle.
- Warm baths or swimming pools can also help to relax a spastic muscle.
- Care of the skinICE
- Frequent changes of the patient’s position (every 2 hours) and of the bed sheets.
- Frequent wash of the skin of the back and pressure points by alcohol followed by talc powder.
2 Care of respiration
- Suction of nasal and pharyngeal secretions.
- Oxygen inhalation via catheter or mask specially in cases of coma.
- Tracheostomy in urgent cases.
- Breathing exercise
- Chest expansion exercise
- Huffing and coughing technique
- Postural drainage
3. Care of nutrition and fluid balance
- Tube feeding giving fruit juices , milk and pureed food , besides I.V. Fluids , in comatosed patients.
4. Care of urinary bladder
- Foley’s self retaining catheter in case of retention or incontinence.
- Urinary antiseptics : Gentamycin 80 mg I.M . every 12 hours.
- Care of bowels : Daily enema.
5. Prevent from deconditioning
- Early mobilization in the bed (activeturning, supine to sit, sit to supine, sitting, sitto stand)
- Pelvic bridging exercise
- Early propped up positioning, sitting & thenlater to standing
- Moving around the bed
- Facilitate movement of functioning limbs
Rehabilitation :
- Repetitive practice of functional tasks with the affected arm to stimulate motor pathways and improve upper limb function.
- Active and passive range of movement exercises to strengthen muscles in the arm leg and trunk and relieve pain and stiffness.
- Stroke rehabilitation begins almost immediately, preferably within 24-36 hours once a patient is found medically stable.
- The Physiotherapist focuses on joint range of motion and strength by performing exercises and re-learning functional tasks such as bed mobility, transferring, walking and other gross motor functions.
- Physiotherapists can also work with patients to improve awareness and use of the hemiplegic side.
Physiotherapy Treatment protocol :
a. Conventional therapies (Therapeutic Exercises, Traditional Functional Retraining)
- Range Of Motion (ROM) Exercises
- Muscle Strengthening Exercises
- Mobilization activities
- Fitness training
- Compensatory Techniques
STRETCHING EXERCISE FOR HEMIPLEGIA :
b. Neurophysiological Approaches:
- Muscle Re-education Approach.
- Neurodevelopmental Approaches: Neurology Treatment Techniques
- rood’s approch
- Movement Therapy Approach (Brunnstrom)
- NDT Approach (Bobath)
- PNF Approach (Knot and Voss)
Hese basic level exercises are a starting point to add flexibility and mobility to your affected arm after a hemiplegia :
- Exercise #1 Inner Arm Stretch.
- Exercise #2 Wrist and Hand Stretch.
- Exercise #3 Elbow Stretch.
- Exercise #4 Crawling Stretch.
- Exercise #5 Wrist Motion.
- Exercise #6 Elbow Weight Training.
- Exercise #7 Finger Walk.
PROGRAM :
Duration :
- The overall duration of the session will be one hour. The total duration of the aerobic/cardiac exercise training should increase from 15 minutes (week one) to 40 minutes by week 12.
Intensity
The intensity of exercise should aim to be moderate as opposed to low. This effort level is required for all components but will be adjusted for each individual according to health status on a session-by-session basis.
Frequency
- The frequency of the session should be three times per week wherever possible.
Functional electrical stimulation (FES):
- FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve.
- In Hemiplegia Physical Therapy, FES has been demonstrated to be beneficial to restore motor control, spasticity, and reduction of hemiplegic shoulder pain and subluxation.
- It is concluded that FES can enhance the upper extremity motor recovery of acute stroke patient.
- FES could reduce spasticity in stroke patient. A recent meta- analysis of randomized controlled trial study showed that FES improves motor strength.
- FES can significantly improve arm function, electromygraphic activity of posterior deltoid, range of motion and reduction of severity of subluxation and pain of hemiplegic shoulder.
Biofeedback:
- Biofeedback is a modality that facilitates the cognizant of electromyographic activity in selected muscle or awareness of joint position sense via visual or auditory cues.
- In Hemiplegia Physical Therapy the result of studies in biofeedback is controversial.
- A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in hemiplegic patient.
- Another meta-analysis study on EMG has showed that EMG biofeedbcak is superior to conventional therapy alone for improving ankle dorsiflexion muscle strengthbshowed that biofeedback could improve earlier postural control to improve impaired sitting balance.
Conventional gait training:
Conventional gait training has focused on part-practice of components of gait in preparation for walking.
It includes
- Symmetrical Weight bearing training
- Weight shifting
- Stepping training (swinging / clearance )
- Heel strike
- Single leg standing
- Push off / Calf rise.
DISCHARGE PLANNING
- Discharge should be considered when the treatment goals are attained
- Home visit should be made prior to the discharge to determine home environment,accessibility.
- Do Exercise regularly .
- Regular follow up should be made .
- Use of affected side as much as possible .
- No vigorous massage .




10 Comments