Temporomandibular joint disorder
What is Temporomandibular joint disorder?
Temporomandibular disorders (TMDs) are a group of more than 30 diseases that cause aches and dysfunction in the jaw joint and muscles that regulate jaw motion. TMDs refers to the diseases, and TMJ refers only to the temporomandibular joint itself. A person has two TMJs; one on per side of the jaw. You can touch them by putting your fingers in front of your ears and opening your mouth.
The National Institute of Dental and Craniofacial Research categorizes TMD by the following:
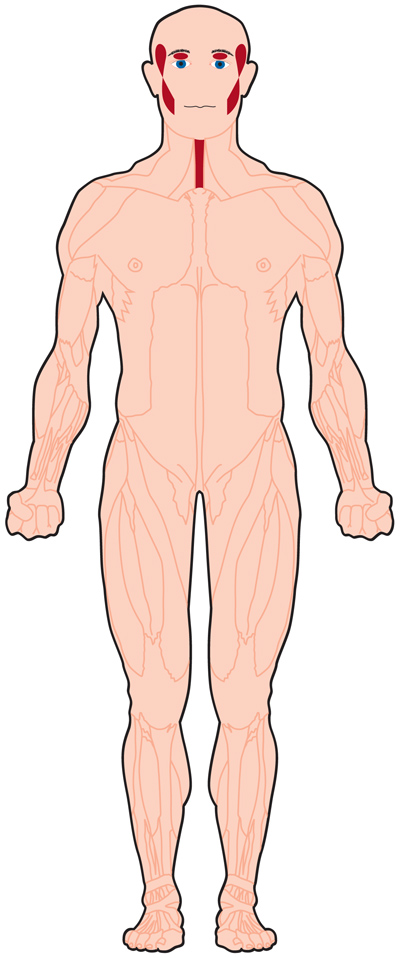
- Myofascial pain. This is the most typical form of Temporomandibular disorder – TMD. It results in discomfort or aches in the fascia (the connective tissue surrounding the muscles) and muscles that regulate the jaw, neck, and shoulder role.
- Internal derangement of the joint. This signifies a dislocated jaw or displaced disk, (cushion of cartilage between the head of the jaw bone and the skull), or damage to the condyle (the spherical end of the jaw bone that communicates with the temporal skull bone).
- Degenerative joint disease. This contains osteoarthritis or rheumatoid arthritis in the jaw joint or junction.
You can have one or more of these diseases at the exact time.
TMD is categorized as intra-articular or extra-articular.
Masticatory Muscle Diseases (Extra-articular)
- Muscle Pain:
- Myalgia
- Tendonitis
- Myositis
- Spasm
- Contracture
- Hypertrophy
- Neoplasm
Temporomandibular Joint Disorders (Intraarticular)
- Joint Pain:
- Arthralgia
- Arthritis
- Joint Disorders:
- Disc Disorders
- Hypo-mobility Disorder
- Hyper-mobility Disorders
- Joint Diseases:
- Degenerative Joint Disease
- Osteoarthrosis
- Osteoarthritis
- five further diseases that occur less commonly
- Fractures
- Congenital and Developmental Disorders
- Aplasia
- Hypoplasia
Epidemiology
Temporomandibular disorders – TMD symptoms can occur at any age, but a peak incidence happens in grown-ups between 20 to 40 years. Females are much more possible to be involved than males, the cause for which is still unrecognized. Even though up to 60 to 70% of the population displays signs of Temporomandibular disorders – TMJ disorders, only 5% to 12% of patients notice symptoms and need treatment.
What causes the temporomandibular joint disorder?
Temporomandibular joint – TMJ disorder can be induced by damage to the jaw joints or junctions or surrounding tissues. Further Temporomandibular disorders – TMD causes contain:
- Bruxism (teeth grinding/clenching).
- Dislocation of the disc between the ball and socket junction or joint.
- Arthritis in the Temporomandibular joint – TMJ.
- Stress.
- Acute trauma.
- An improper bite.
What are common TMJ symptoms?
Temporomandibular joint – TMJ dysfunction is most familiar in those 20 to 40 years of age and is more familiar in females than in males. Some of the most familiar Temporomandibular joints – TMJ symptoms contain:
- Jaw pain.
- Headaches.
- Earaches.
- Ache in the neck or shoulders.
- A problem in opening your mouth wide.
- Jaws lock in the open or either closed mouth position.
- Clicking, popping, or grating sounds in the jaw joint or junction when opening or closing your mouth.
- A tired feeling on your face.
- A problem in chewing.
- Tinnitus, or ringing in your ears.
- Changes in the way your teeth fit jointly.
- Swelling on the side of your face.
- Toothache.
Risk factors
While some factors are frequently associated with the development of Temporomandibular joint TMJ disorders, they haven’t been confirmed to be a direct cause.
Some of these contain:
- female hormones (it’s theorized that estrogen may recreate a function in the development of Temporomandibular joint – TMJ)
- poor posture affects the muscles of the neck and face
- prolonged pressure
- joint or junction hypermobility
How is TMJ dysfunction diagnosed?
In most patients, Temporomandibular joint – TMJ dysfunction is analyzed during a dental checkup. Your healthcare provider or doctor will:
Observe the range of movement when you open and close your mouth.
Squeeze on your face and jaw to specify places of discomfort.
Touch around your jaw joints or junctions as you open and close your mouth.
In extra, radiographs (X-rays) may be brought to view the jaw joints or junctions and define the extent of the damage. These may contain:
Panoramic X-rays. This kind of dental X-ray demonstrates a wide summary of your teeth, jawbone, and Temporomandibular joint – TMJs.
CBCT scans. Cone beam computed tomography (CBCT) inspects and captures thousands of images of your jaws, teeth, facial bones, and sinuses. These images are then sewn together for a detailed 3-D picture. Dental CT scans provide your healthcare provider or doctor with a more precise picture of your facial anatomy.
MRI scans. In some patients, magnetic resonance imaging (MRI) may be used to view soft tissues in and around the jaw joints or junctions. These pictures display the position of the disk, inflammation, and likely jaw locking. This can inform your healthcare provider or doctor if the Temporomandibular joint – TMJ disc is working correctly and in a fine state.
You may be guided to a specialist for additional care and therapy. An oral maxillofacial surgeon or doctor specializes in treating skeletal diseases such as Temporomandibular joint – TMJ dysfunction.
Treatment of Temporomandibular disorders
Medical treatment
To ease aches and swelling, try over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), like aspirin, ibuprofen (Advil, Motrin), or naproxen (Aleve). Your healthcare provider or doctor can specify higher doses of NSAIDs or other medications for pain like narcotic analgesics.
Muscle relaxants, particularly for a patient who grind or clench their teeth, can assist loosen tense jaw muscles. Anti-anxiety medications can assist reduce tension, which is occasionally thought to aggravate Temporomandibular joint – TMJ symptoms. A low dose of antidepressants can also assist to decrease or prevent pain. Muscle relaxants, anti-anxiety medications, and antidepressants are available by prescription solely.
Physiotherapy treatment in Temporomandibular disorders
Stretching activities can enhance the range of movement but do not always ease the pain. The generally used manual methods are joint or junction mobilization, soft tissue mobilization, resistance activities, muscle conditioning, assisted muscle stretching, passive muscle stretching, and postural training. Other physical treatment modalities contain ultrasound, thermotherapy, electro galvanic stimulation, and cold laser.
Transcutaneous electrical nerve stimulation (TENS). This treatment uses low-level electrical currents to decrease aches by resting your jaw joint or junction and facial muscles. TENS can be conducted at home or at your healthcare provider or doctor’s office.
Ultrasound. This is a deep heat therapy that is applied to the temporomandibular joint – TMJ to reduce soreness or enhance joint or junction motion.
Use a hot or cold compress
Ice assists to decrease swelling and pain, while heat can improve blood flow and loosen your jaw muscles. Use a hot or cold compress on your jaw for 15 to 20 minutes at a time using a light coating between the compress and your skin.
Radio wave therapy. Radio waves facilitate the joint or junction, which improves blood flow and reduces aches.
Low-level LASER therapy. This lowers aches and inflammation and assists you move your neck more willingly and open your mouth broader.
In some patients, surgical therapies may be needed, however, generally, the discomfort and ache associated with temporomandibular joint TMJ disorders are temporary and can be reduced with non-invasive treatments, involving doing temporomandibular joint – TMJ activities.
Relaxed Jaw Exercise
Rest your tongue slightly on the top of your mouth and after your upper front teeth. Then permit your teeth to come split while you rest your jaw muscles.
Goldfish Exercises (Partial Opening)
Put your tongue on the top of your mouth and one of your fingers in front of your ear where your temporomandibular joint – TMJ is situated. Place your pointer finger on your chin, lower your lower jaw center and then close it. You should sense mild opposition but no pain. A variation of this activity is to put one finger on per temporomandibular joint – TMJ point as you lower your lower jaw center and then close it again.
Goldfish Exercises (Full Opening)
Maintaining your tongue on the top of your mouth, put one finger on your temporomandibular joint – TMJ point and another on your chin (or you can do both temporomandibular joints – TMJs at the exact time). Lower your lower jaw fully, and then close your mouth again. One set of activities includes doing this six times, and you should accomplish one set six times a day.
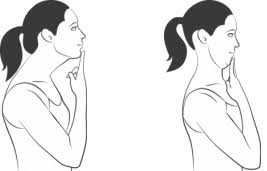
Chin Tucks
With your chest elevated and your shoulders retracted, drag your chin directly back and make a double chin. Maintain this pose for three seconds and replicate it ten times.
Resisted Mouth Opening
Put your thumb under your chin and open your mouth gradually while you slightly push against your chin for the opposition. Maintain for three to six seconds, and then close your mouth gradually.
Resisted Mouth Closing
Press your chin with your thumb and index finger with one hand. Close your mouth as you slightly put stress on your chin. This activity will assist strengthen the muscles that assist you to chew.
Tongue Up
Gradually open and close your mouth while your tongue is feeling the top of your mouth.
Side-To-Side Jaw Movements
Put a half a centimeter thing (such as a tongue depressor or art stick) between your front teeth. Gradually move your jaw from side to side. As this activity becomes more comfortable, improve the consistency of the thing between your teeth.

Forward Jaw Movement
Put a half a centimeter thing (such as a tongue depressor or art stick) between your front teeth. Move your lowest jaw forward, so your lowest teeth are in front of your roof teeth. Improve the consistency of the thing between your teeth as this activity becomes more comfortable.
Reduce stress
Try meditation methods to assist ease and relax your jaw. Yoga exercises can also assist put a minor strain on your muscles, and gardening is a great exercise to try to relax your mind and soothe your face.
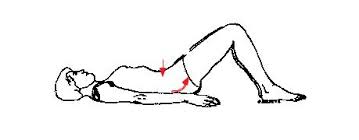
Get a good posture
Sleep is essential for many parts of good fitness. To assist minimize temporomandibular joint – TMJ pain, rest on your back and use cushions to keep your neck. You should avoid resting on your stomach, and if resting on your side, accomplish not put your hand on your jaw.
Correct your posture
Sitting in an unideal position for long periods can induce you to feel more aches in your jaw.
When performing, select a chair with a back asset and take regular breaks to enhance your posture. While driving, put your seat to be as good as possible, and while doing leisure exercises, like watching TV or reading, select a space that permits you to sit erect and put a cushion behind your back for an asset.
The subsequent activity to update your sitting or standing posture: Lift your chest bone, drag your shoulders back and slightly press your shoulder edges to straighten your back muscles.
Alternative TMJ treatments
Many healthcare providers or doctors suggest using alternative treatments in combination with traditional therapies. These treatments may contain:
Relaxation techniques. Mindfulness or meditation can assist you to slow your breathing and relax tight muscles. As an outcome, aches can be decreased.
Acupuncture. This technique includes inserting thin syringes into the body at different points. Acupressure points may activate the central nervous system and facilitate your body’s natural recovery processes.
Biofeedback. Electronic devices can be used to catch places of tension and tightness in your body. This offers you a greater understanding of where you’re having tension so you can concentrate on calming these muscles.
Pain management referrals. In some patients, you may be referred to an ache psychologist or ache management clinic to assist to reduce their symptoms.
Trigger-point injections. Pain medicine or anesthetic is injected into tender muscles of the face (known as “trigger points”) to reduce pain.
Radio wave therapy. Radio waves make a low-level electrical impulse to the joint or junction, which improves blood flow and delivers temporomandibular joint – TMJ ease.
Botulinum Toxin (Botox). These injections assist to decrease muscle mass and inflammation.
TMJ surgery
Temporomandibular joint – TMJ surgery should only be considered after all other therapy choices have been tried and severe pain stays. While temporomandibular joint – TMJ surgery is the best choice for many patients, it’s essential to weigh your choices and create an informed decision.
There are three kinds of temporomandibular joint – TMJ surgery: arthrocentesis, arthroscopy, and open-joint or junction surgery. The type of surgery required depends on the temporomandibular joint – TMJ symptoms and the complexity of the issue.
Arthrocentesis. This minor method is conducted in the office, generally under local anesthesia. It’s frequently suggested when the jaw suddenly locks in the closed position. It can also assist to decrease inflammation in the temporomandibular joint – TMJ. Syringes filled with sterile fluids are inserted into the involved joint or junction and the joint or junction is washed out. Sometimes, a surgical tool is required to remove scar tissue or to dislodge a disc that has shifted out of position.
Arthroscopy. This method is conducted under general anesthesia. Your surgeon or doctor creates a small incision in front of the ear and inserts a small, thin device that includes a lens and light. This device is tied up to a video screen, which permits your surgeon or doctor to inspect the temporomandibular joint – TMJ and the surrounding region. Depending on the cause of your temporomandibular joint – TMJ pain, your surgeon or doctor may withdraw inflamed tissue or realign the disc or another location of the temporomandibular joint – TMJ. Because arthroscopic surgery is conducted via tiny incisions, there is minor scarring, a shorter healing time, minor discomfort, and fewer difficulties compared with open-joint surgery.
Open-joint surgery. If you undergo open-joint or junction surgery, you’ll be offered general anesthesia. Unlike arthroscopy, open surgery is the traditional method in which a long incision is created to insert tools. Open-joint or junction surgeries may be required if:
- The bony structures that make up the jaw joint or junction are wearing out.
- There are tumors in or close to the temporomandibular joint – TMJ.
- There is extreme scarring or bone chips in the joint or junction.
Compared to arthrocentesis and arthroscopy, open-joint or junction surgery results in a longer recovery time plus has a more significant possibility of tissue scarring and nerve damage. Yet, there are examples in which open-joint or junction surgery is the best solution. Your healthcare provider or doctor can assist you to decide which method is right for your unique requirements
Home remedies for TMJ disorder
If you’ve been analyzed with temporomandibular joint – TMJ disorder, your healthcare provider or doctor will likely suggest conservative therapy choices first. Many of these treatments can work in combination with one another to provide temporomandibular joint – TMJ ease:
Use moist heat or cold packs. Use an ice pack to the side of your face and temple site for approximately 10 minutes for acute aches. Accomplish a few simple stretching activities for your jaw (as recommended by your healthcare provider or doctor). After exercising, use a warm towel or washcloth on the side of your face for approximately five minutes. Accomplish this a few times per day.
Eat soft foods. To maintain your jaw from performing overtime, eat soft foods like mashed potatoes, yogurt, soup, cottage cheese, fish, scrambled eggs, beans, cooked fruits and vegetables, and grains. Avoid stiff and crunchy foods (such as pretzels, hard rolls, and raw carrots) and chewy foods (such as caramels and taffy). Accomplished chew gum.
Wear a splint or night protection. Splints and night protection are mouthpieces that hold over your upper or lower teeth. When worn, the mouthpieces deliver steady tooth contacts during closure. When worn, mouth guards also fix your bite by putting your jaw in a more good position. The main contrast between splints and night guards is those night guards are solely worn at night and splints are worn full time. Your healthcare provider or doctor can decide which kind of oral appliance you may require.
Undergo corrective dental therapies. These therapies involve substituting missing teeth or using crowns, bridges, or braces to obtain your bite into good balance and alignment.
Avoid extreme jaw movements. For example:
- Maintain yawning and chewing to a minimum.
- Don’t relax your chin on your hand or maintain the telephone between your shoulder and ear. Practice the right posture to decrease neck and facial pain.
- Maintain your teeth barely apart as frequently as you can to reduce stress on the jaw. To prevent clenching or grinding during the day, put your tongue on the palate behind your upper front teeth.
- Know relaxation techniques to assist in managing muscle tension in the jaw.
Take notice of bad habits
You may have a few tendencies that can induce temporomandibular disorder – TMD pain. Such habits contain:
- Nail biting
- Chewing cheeks and lips
- Resting your jaw in your hand
- Clenching your teeth
- Grinding your teeth
- Clenching jaw muscles pushing the tongue opposite your teeth
- Take note of your daily habits and jot them down to concern with your doctor o physician. Hold in mind how frequently you do them.
Prognosis
Up to 40% of persons say the remission of symptoms without any intervention, and most persons have a favorable reaction to conservative therapy. A small numeral of persons produces refractory or persistent temporomandibular disorder – TMD. There are no known risk factors associated with chronic temporomandibular disorder – TMD. But, just published information related to heightened sympathetic tone with chronic temporomandibular joint – TMJ pain
FAQ
Does TMJ disorder go away?
Recall that for most people, pain from temporomandibular joint TMJ disorders will finally go out on its own. Simple self-care techniques are frequently useful in reducing symptoms. If therapy is required, it should be established on a reasonable diagnosis, be conservative and reversible, and be customized to your special requirements.
Is TMJ disorder serious?
After being analyzed with the temporomandibular joint disorder (TMD), many of our Nashville, TN, peoples ask, Is TMJ disorder severe? The explanation is that although the situation is not life-threatening, it can have substantial negative impacts on your dental and overall fitness.
Should I be worried about TMD?
Failure of jaw cartilage and bone mass: Without corrective actions, temporomandibular disorder – TMD can permanently harm the jaw. The cartilage that helps the joint or junction can wear away, while the jawbone may deteriorate. This causes aching friction in the jaw and improves the possibility of jaw dislocation.
What happens if you don’t treat TMD?
Although not life-threatening, if temporomandibular joint TMJ disorder is left untreated, it can contribute to considerable pain and tension. Chronic aches can even lead to the growth of conditions such as anxiety and depression.
What do dentists do for TMD?
Therapy from an orthodontist can relieve temporomandibular joint – TMJ symptoms in many patients. If your temporomandibular joint – TMJ arrives from teeth grinding or clenching, your dentist may suggest that you wear a traditional dental device. Frequently known as a bite plate or a splint, this device will support your upper teeth from grinding against your inferior teeth.






4 Comments