Vitamin A
What is Vitamin A?
Animals require fat-soluble vitamin A as one of their basic nutrients. The word “vitamin A” refers to a class of chemically related organic substances that comprises various provitamin (precursor) carotenoids, most notably beta-carotene, retinoic acid, retinol, and retinal (also known as retinaldehyde).
Vitamin A performs a variety of tasks, including immune system maintenance, embryonic development and growth, and vision, where it interacts with the protein opsin to generate rhodopsin, the light-absorbing molecule required for color and low-light (scotopic) vision.
There are two main types of vitamin A found in food: Retinol can be found in animal-based foods in two forms: A) as retinol or bound to a fatty acid to form a retinyl ester and B) as provitamin A in herbivorous and omnivorous animals that have the enzymes to cleave and convert provitamin carotenoids to retinal and then to retinol.
Alpha-, ß-, gamma-, and beta-carotene, as well as beta-cryptoxanthin, are carotenoids that contain ß-ionone rings and act as provitamin A. This enzyme is absent in certain carnivorous species. There is no vitamin action in the remaining carotenoids.
Passive diffusion is how dietary retinol is taken up from the digestive tract. In contrast to retinol, ß-carotene is absorbed by enterocytes through the membrane transporter protein scavenger receptor B1 (SCARB1), which experiences an increase in expression during periods of low vitamin A.
In the liver, retinol is stored in lipid droplets. Because retinol has great potential for long-term storage, well-nourished people can go for months without eating enough vitamin A or ß-carotene while still having acceptable blood levels.
Deficiency signs and symptoms appear only when the liver resources are almost completely exhausted. Hundreds of genes are activated by the reversible conversion of retinol to retinal and subsequently irreversibly to retinoic acid.
In underdeveloped nations, particularly in Sub-Saharan Africa and Southeast Asia, vitamin A insufficiency is prevalent. Although deficiency can strike anyone at any age, it most frequently affects preschool-aged children and expectant mothers, the latter of whom must transfer retinol to the developing fetus.
Approximately one-third of children under the age of five worldwide are thought to be affected by vitamin A deficiency, which leads to hundreds of thousands of cases of blindness and fatalities from childhood diseases due to immune system failure.
One sign of low vitamin A status early on is reversible night blindness. A biomarker called plasma retinol is used to confirm vitamin A insufficiency. Retinol in breast milk from nursing mothers may be a sign of a deficit. The state of the liver reserves is not indicated by either of these metrics.
Upper limits for safe intake have been established by the European Union and other nations, along with recommendations for dietary intake. When the body accumulates too much vitamin A, it can lead to vitamin A toxicity, also known as hypervitaminosis A.
Nervous system effects, liver abnormalities, exhaustion, muscle weakness, alterations in the skin and bones, and other symptoms are possible. Stopping the use of high-dose supplements reverses the negative effects of both acute and chronic poisoning.
Definition
As a fat-soluble vitamin, vitamin A belongs to the same class as vitamins D, E, and K. A ß-ionone ring is present in all of the vitamers, which are chemically related naturally occurring molecules or metabolites that make up the vitamin.
The main dietary form is retinol, which when stored in the liver can link a fatty acid molecule to produce retinyl ester. Retinol dehydrogenases catalyze the conversion of retinol to retinal, which is then converted back to retinol by retinaldehyde reductases. Retinol is the transport and storage form of vitamin A.
retinal + NADPH + H+ ? retinol + NADP+
retinol + NAD+ ? retinal + NADH + H+
dehydrogenase has the ability to permanently convert retina (also known as retinaldehyde) to all-trans-retinoic acid.
retinal + NAD+ + H2O ? retinoic acid + NADH + H+
Diffusing into the cell nucleus, retinoic acid binds directly to gene targets through retinoic acid receptors to regulate over 500 genes.
Apart from retinol, retinal, and retinoic acid, carotenoids derived from plants, fungi, or bacteria can also be converted to retinol through metabolism, making them vitamin A metabolites.
Additionally, there are retinoids known as second, third, and fourth generation, which are not regarded as vitamin A vitamers due to their inability to be converted into retinol, retinal, or all-trans retinoic acid. Some are oral or topical prescription medications with different purposes. Adapalene, bexarotene, tazarotene, trifarotene, acitretin, and etretinate are a few examples.
Absorption, Metabolism, and Excretion
In the small intestine lumen, retinyl ester hydrolases react with retinyl esters from animal-based diets (or synthetic sources for human and domestic animal dietary supplements) to liberate free retinol. Via passive diffusion, the retinal reaches intestine absorptive cells. The range of absorption effectiveness is 70% to 90%.
Because there are no systems in place to prevent the absorption of vitamin A or eliminate excess in the urine, humans are susceptible to acute or chronic vitamin A toxicity. Retinol is coupled to retinol-binding protein 2 (RBP2) inside the cell. Lecithin retinol acyltransferase then uses it to enzymatically reesterify it, and the resulting chylomicrons are released into the lymphatic system.
The membrane transporter protein scavenger receptor B1 (SCARB1) is responsible for the uptake of ß-carotene by enterocytes, in contrast to retinol. When there is a vitamin A shortage, the protein is overexpressed. When vitamin A levels are within normal limits, SCARB1 is downregulated, which lowers absorption.
The enzyme that codes for the BCMO1 gene, beta-carotene 15,15′-dioxygenase (formerly known as beta-carotene 15,15′-monooxygenase), which symmetrically cleaves ß-carotene into retinal, is also downregulated. Either absorbed ß-carotene is coupled to RBP2 or is first transformed to retinal and then retinol, which is then integrated into chylomicrons.
Approximately two-thirds of the chylomicrons are absorbed by the liver following a meal, with the remaining portion going to the peripheral tissues. Chylomicron ß-carotene can also be converted to retinol by peripheral tissues.
Because the liver has the ability to retain retinol, well-nourished people can spend months without showing any symptoms of a vitamin A deficit. Hepatocytes and hepatic stellate cells are the two types of liver cells that are in charge of storage and release (HSCs). Hepatocytes absorb the chylomicrons rich in fat, attach retinol to RBP4 (retinol-binding protein 4), and then move the retinol-RBP4 to HSCs where it is stored as retinyl esters in lipid droplets.
The process is reversed during mobilization when free retinol is released by retinyl ester hydrolase, transported to hepatocytes, bound to RBP4, and injected into the bloodstream. More than 95% of the retinol in circulation is bound to RBP4, with the exception of periods following meals or when excessive consumption surpasses liver storage capacity.
Carnivores
Compared to omnivores and herbivores, strict carnivores handle vitamin A in a different way. Because they can excrete retinol and retinyl esters in their urine, carnivores are able to withstand higher retinol doses. Because they have a higher ratio of liver HSCs to hepatocytes than omnivores and herbivores, carnivores can also store more in their livers.
The range of liver content in humans is 20-30 µg/gram wet weight. Because of its very high content—which has been known to vary from 2,215 to 10,400 µg/g wet weight—polar bear liver is extremely poisonous to humans. As mentioned, retinol circulates attached to RBP4 in humans. R-RBP4 is kept within a narrow range by carnivores, who also have retinyl esters in their system. Cells receive bound retinol delivery during Urine containing the esters that are expelled.
Carnivore animals are generally poor converters of ionone-containing carotenoids, and pure carnivores, such as felidae (cats), are completely devoid of the cleaving enzyme. Their diets must contain retinol or retinyl esters.
Herbivores
Carotenoids containing ionone are consumed by herbivores, who then turn them into retinal. There are detectable levels of beta-carotene in the blood and stored in body fat, resulting in yellow fat cells, in certain species, such as horses and cattle. The majority of animals lack beta-carotene in their blood and have white fat.
Activation and excretion
Alcohol dehydrogenases, which are also in charge of converting ethanol to acetaldehyde, reversibly convert retinol to retinal in the liver and peripheral tissues of humans. Aldehyde dehydrogenases convert the retina into retinoic acid (RA) in an irreversible manner. Gene activation and inactivation are regulated by RA.
RA causes oxidative deterioration; its presence causes its elimination, resulting in a transcribing gene signal with a short half-life. A series of cytochrome P450 (CYP) enzymes, namely CYP26A1, CYP26B1, and CYP26C1, mediates this deactivation. In the human liver, CYP26A1 is the most common type; CYP26B1 was found in higher concentrations in all other adult human organs.
The majority of CYP26C1 expression occurs during embryonic development. Retinoic acid is converted by all three into 4-oxo-RA, 4-OH-RA, and 18-OH-RA. The oxidized metabolites combine with glucuronic acid to generate water-soluble glucuronide conjugates, which are subsequently eliminated in urine and feces.
Metabolic Functions
All-trans retinoic acid (RA) mediates the metabolic actions of vitamin A, except vision. Retinal can only create RA, and it cannot be reversed. Its short half-life allows it to be rapidly oxidized and removed, preventing the buildup of RA.
Retinoic acid oxidation is catalyzed by three different cytochromes. Elevated levels of RA stimulate the genes encoding Cyp26A1, Cyp26B1, and Cyp26C1, so establishing a self-regulating feedback loop.
Vision and Eye Health
Two distinct processes are involved in vitamin A status and eye health. Rod and cone cells in the retina respond to light exposure by transmitting nerve signals to the brain, and the retina is a crucial component of this process. Night blindness is an early indicator of vitamin A insufficiency. Renin, or vitamin A, is necessary for the proper operation of epithelial cells.
Severe vitamin A deficiency results in xerophthalmia, which is characterized by dryness of the cornea and conjunctival epithelium. This condition is frequent in infants and young children in Southeast Asia. If left untreated, xerophthalmia can lead to blindness and corneal ulcers.
Vision
Retinal molecule plays a specific role in vitamin A’s role in the visual cycle. The retinal pigment epithelium’s RPE65 enzyme transforms retinol into 11-cis-retinal. Rhodopsin in rod cells and iodopsin in cone cells are the result of the binding of 11-cis-retinal to the protein opsin within the eye. The 11-cis-retinal is isomerized to the all-trans form as light enters the eye. In a process known as photo-bleaching, the all-trans-retinal separates from the opsin.
A nerve signal is produced by this isomerization and travels via the optic nerve to the brain’s vision center. Following their split from opsin, the entire through a series of enzymatic activities, trans-retinal is recycled and transformed back into the 11-cis-retinal form. The cycle is finally completed when trans-retinal binds to opsin to generate rhodopsin in the retina.
Furthermore, a portion of the all-trans retina may be transformed into all-trans retinol and subsequently delivered to the retinal pigmented epithelium cells via an interphotoreceptor retinol-binding protein. Reusable storage of all-trans-retinol within pigment epithelial cells is made possible by subsequent esterification into all-trans-retinyl esters.
Because of this, a vitamin A deficit will prevent rhodopsin from reforming, which will result in night blindness, one of the initial symptoms.
Night blindness
Night blindness due to a vitamin A deficiency (VAD) is a temporary impairment in the eyes’ ability to acclimate to low light levels. It frequently occurs in young infants whose diets are deficient in beta-carotene and retinol. In reaction to low light levels, photopigment levels usually increase due to a process known as dark adaption.
This can lead to a 100,000-fold increase in light sensitivity over standard daylight settings. notable improvement at night Although vision appears in ten minutes, the procedure may take up to two hours to fully manifest. In order to avoid reversing the adaptation, people who anticipated working in a dark setting wore red-tinted goggles or were in an environment with red light, as opposed to yellow or green light, which causes rhodopsin to be depleted.
Xerophthalmia and childhood blindness
The pathologic dryness of the cornea and conjunctival epithelium characterizes xerophthalmia, which is brought on by a severe vitamin A deficiency. The conjunctiva thickens, wrinkles, and becomes dry.
Bitot’s spots, which are accumulations of keratin debris inside the conjunctiva, are indicative. Excessive xerophthalmia can cause damage to the cornea and retina, which can lead to dry eye syndrome, corneal ulceration, and finally blindness.
While xerophthalmia is a condition affecting the eyes, retinoic acid that has been generated from the retinal rather than the 11-cis-retinal to rhodopsin cycle plays a role in its prevention and reversal.
Estimates for subclinical vitamin A deficiency and night blindness in children under six years old are high throughout Southeast Asia; the major cause of avoidable childhood blindness is xerophthalmia. According to estimates, there are 350,000 cases of childhood blindness brought on by a vitamin A shortage.
Pregnancy-related vitamin A deficiency, low transfer of vitamin A during nursing, and low-vitamin A or beta-carotene diets for infants and children are the causes.
Because childhood vitamin A insufficiency considerably increases all-cause death, the proportion of pre-school-age children blinded by vitamin A deficiency is lower than expected from the incidence of new cases alone.
A 2017 Cochrane review found that vitamin A deficiency, defined as serum retinol less than 0.70 µmol/L, is a significant public health issue that affects an estimated 190 million children under five in low- and middle-income nations, mostly in Southeast Asia and Sub-Saharan Africa.
Instead of or in addition to food fortification initiatives, numerous nations have established public health campaigns where children are administered very large oral doses of synthetic vitamin A (retinyl palmitate) on a regular basis to treat and prevent VAD.
Children between the ages of six and eleven months received doses of 50,000 to 100,000 IU (International units), whereas children between the ages of twelve months and five years received doses of 100,000 to 200,000 IU, usually every four to six months.
There was also a reported 24% decrease in all-cause mortality along with outcomes pertaining to the eyes. At follow-up, the prevalence of Bitot’s spots was decreased by 58%, night blindness by 68%, and xerophthalmia by 69%.
Gene regulation
Retinoic acid receptors (RARs; RARa, RARß, RAR?) are nuclear receptors that bind to DNA in heterodimers with retinoid “X” receptors (RXRs; RXRa, RXRß, RXR?) and are responsible for regulating gene transcription. Before RARs and RXRs can attach to DNA, they need to dimerize. More than 500 genes have an effect on retinoic acid-responsive expression.
RAR-RXR heterodimers function by identifying retinoic acid response sites on DNA. Co-repressors separate from the receptors as a result of a conformational shift in the receptors. After that, coactivators can attach to the receptor complex, which could interact with the transcriptional machinery or aid in releasing the chromatin structure from the histones.
Target genes, including those that code for the receptors themselves, have their expression either upregulated or downregulated as a result of this reaction. The overabundance of RA needs to be broken down and removed in order to avoid buildup.
Cyp26A1, Cyp26B1, and Cyp26C1 are the three cytochromes that catalyze the oxidation of RA. High levels of RA stimulate the genes encoding these proteins, hence offering a regulatory feedback mechanism.
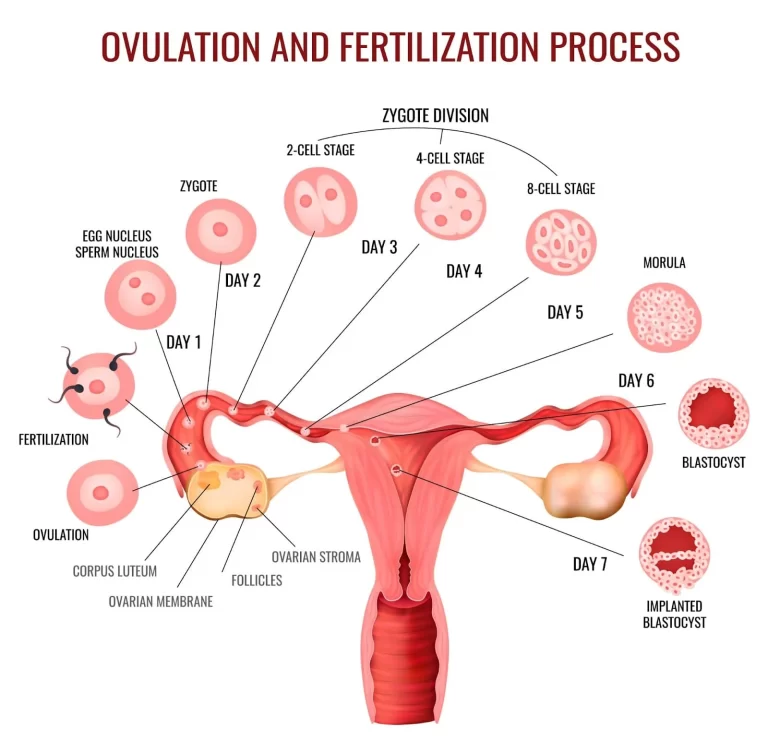
Embryology
Invertebrate chordates and vertebrates, RA plays a critical function in development. Congenital vascular and cardiovascular disorders are among the birth malformations caused by varying levels of endogenous RA signaling during early embryology, both too high and too low.
Notably, congenital abnormalities such as craniofacial, auditory, and visual malformations, neurobehavioral abnormalities, and mental disorders are all included in the category of fetal alcohol spectrum disorder.
This resulted from the mother drinking alcohol while she was pregnant. It is suggested that acetaldehyde, an ethanol metabolite, and retinaldehyde (retinal) compete with one another for aldehyde dehydrogenase activity in the embryo, leading to a shortage in retinoic acid and congenital birth abnormalities caused by the absence of RA-triggered gene activation.
This notion is supported by the observation that raising retinol or retinal levels might mitigate developmental abnormalities caused by ethanol.
Concerning the dangers of excessive retinoic acid (RA), the prescription medications isotretinoin (13-cis-retinoic acid) and tretinoin (all-trans-retinoic acid), Because they are proven human teratogens, products intended for topical or oral use in the treatment of acne are accompanied by cautions not to be used by women who are pregnant or planning to become pregnant.
Immune Functions
There is a connection between reduced resistance to viral illnesses and vitamin A deficiency (VAD).
Vitamin A supplementation public health programs started in the 1980s, have been found to lower the prevalence of diarrhea and measles, as well as all-cause mortality, in nations where early childhood VAD is frequent.
Additionally, VAD raises the possibility of an overreaction by the immune system, which can result in autoimmune illnesses, increased allergic reactions, and intestinal inflammation that lasts a long time.
Among the white blood cells that make up the immune system are lymphocytes and monocytes. Natural killer cells, which support innate immunity, T cells, which support adaptive cellular immunity, and B cells, which support antibody-driven adaptive humoral immunity, are examples of lymphocytes.
Dendritic cells and macrophages are produced by monocytes. Certain lymphocytes move to the thymus, where they undergo additional differentiation after emerging from the thymus into a variety of T cell subtypes, also known as “killer” or “helper” T cells.
The cytokines released by each subtype and the organs to which the cells migrate preferentially—a process known as trafficking or homing—determine their functions.
The function of retinoic acid (RA) in the immune system is described in reviews based on in vitro and animal studies. White blood cell production in bone marrow is triggered by receptors in RA.
White blood cell development and proliferation, T cell migration to the intestinal tract, and the up-and down-regulation of lymphocyte activity are all regulated by RA.
Th1 T helper cell subtype is inhibited and Th2, Th17, and iTreg (for regulatory) subtypes are activated if RA is sufficient. Enzymes found in intestinal tissue’s dendritic cells convert retinal to all-trans-retinoic acid, which cells’ retinoic acid receptors will then absorb.
Th2, Th17, and iTreg T cell types migrate to and settle in mesenteric lymph nodes and Peyer’s patches, which are located outside and on the inner wall of the small intestine, respectively, as a result of the process’s activation of gene expression.
Overall, this results in a down-regulation of immune activity, which is manifested as tolerance to food allergens and to the microbiome of the large intestine’s resident bacteria and other species.
Th1 cells that promote inflammation are predominant and innate immunity is weakened in a vitamin A deficient state.
Skin
Vitamin A deficiency has been associated with a higher risk of inflammation and skin infections. Through its metabolite, retinoic acid (RA), vitamin A appears to regulate the innate immune response and maintain mucosal and epithelial tissue homeostasis.
Toll-like receptors in skin cells, which are a component of the innate immune system, react to infections and cell injury by triggering a pro-inflammatory immune response that includes an increase in the production of RA.
The skin’s epithelium comes into contact with viruses, fungi, and bacteria. Antimicrobial peptides (AMPs) are produced and secreted by keratinocytes located in the epidermal layer of the skin. RA stimulates the production of the AMPs resistin and cathelicidin.
Units of Measurement
Since some carotenoids can be turned into vitamin A, efforts have been made to compare the benefits of various foods by figuring out how much of them in the diet is equivalent to a given amount of retinol. Due to the fact that the recognized equivalencies have evolved throughout time, the situation can be unclear.
An international unit (IU) was equivalent to 0.3 µg of retinol (~1 nmol), 0.6 µg of ß-carotene, or 1.2 µg of other provitamin-A carotenoids for a considerable amount of time under the previous equivalency system.
| Material and its chemical surroundings (per 1 μg) | IU (1989) | μg RE (1989) | μg RAE (2001) |
| Retinol | 3.33 | 1 | 1 |
| beta-carotene, dissolved in oil | 1.67 | 1/2 | 1/2 |
| beta-carotene, a common dietary | 1.67 | 1/6 | 1/12 |
| alpha-Carotene, common dietary gamma-Carotene, common dietary beta-Cryptoxanthin, common dietary | 0.83 | 1/12 | 1/24 |
Retinol equivalents (REs) were another way to represent this relationship: one RE was equal to 1 µg of retinol, 2 µg of ß-carotene dissolved in oil, 6 µg of ß-carotene in food, and 12 µg of either a-carotene, ?-carotene, or ß-cryptoxanthin in food.
Recent studies have revealed that provitamin-A carotenoids are approximately half as well absorbed as previously believed. Consequently, the US Institute of Medicine proposed the retinol activity equivalent (RAE) as a new unit in 2001.
One µg of retinol, two µg of oil-derived ß-carotene, twelve µg of “dietary” beta-carotene, or twenty-four µg of the other three dietary provitamin-A carotenoids are equivalent to one µg RAE.
Based on animal models, it has been demonstrated that the membrane transporter protein scavenger receptor class B, type 1 (SCARB1) absorbs ß-carotene at the enterocyte cell wall. Retinal is produced from absorbed ß-carotene, followed by retinol.
In the initial phase of conversion, a single ß-carotene molecule is broken down into two retinal molecules by the enzyme ß-carotene-15, 15′-monooxygenase, which is encoded by the BCM01 gene in humans and other mammals. Gene expression for SCARB1 and BC01 is inhibited when plasma retinol is within the normal range.
This creates a feedback loop that inhibits the absorption and conversion of ß-carotene. Since receptor 36 is not downregulated, absorption suppression is not entirely achieved.
Dietary Recommendations
Dietary Reference Intakes (DRIs) for vitamin A, which included Recommended Dietary Allowances (RDAs), were revised by the US National Academy of Medicine in 2001. Since there was insufficient data to determine an RDA for infants under 12 months of age, Adequate Intake (AI) is displayed in its place.
| Life stage group | US RDAs or AIs (μg RAE/day) | US Upper limits (μg/day) |
| Infants 0–6 months 7–12 months | 400 (AI) 500 (AI) | 600 600 |
| Children 1–3 years 4–8 years | 300 400 | 600 900 |
| Males 9–13 years 14–18 years >19 years | 600 900 900 | 1700 2800 3000 |
| Females 9–13 years 14–18 year >19 years | 600 700 700 | 1700 2800 3000 |
| Pregnancy<19 years >19 years | 750 770 | 2800 3000 |
| Lactation <19 years <19 years | 1200 1300 | 2800 3000 |
Tolerable upper intake limits (ULs) were also developed in the interest of safety. Carotenoids are subtracted from the total vitamin A intake for ULs in safety evaluations.
The combined collection of data is referred to as Dietary Reference Values by the European Food Safety Authority (EFSA), which uses Population Reference Intake (PRI) rather than RDA and Average Requirement (EAR) in place of EAR.
The definitions of AI and UL are the same as in the US. The PRIs are set at 650 and 750 µg RE/day for males and women who are 15 years of age and above, respectively. PRI is 700 µg RE/day during pregnancy and 1300/day throughout lactation.
The PRIs rise with age for children aged 1 to 14 years, from 250 to 600 µg RE/day. These PRIs and US RDAs are comparable.
After reviewing the same safety question as the US, the European Food Safety Agency (EFSA) set upper limits (ULs) for preformed vitamin A (i.e., excluding dietary contributions from carotenoids) at 800 for ages 1-3, 1100 for ages 4–6, 1500 for ages 7–10, 2000 for ages 11–14, 2600 for ages 15–17, and 3000 µg/day for years 18 and older.
Safety
When the body stores too much vitamin A, it can lead to vitamin A toxicity, also known as hypervitaminosis A. It results from consuming preformed vitamin A rather than carotenoids since sufficient retinol inhibits the latter’s ability to convert to retinol.
Retinol safety
There are historical accounts of cases of acute hypervitaminosis from eating fish liver, but otherwise, there is no risk from consuming too much of commonly consumed foods. Arctic explorers have been known to consume bearded seals or polar bear livers, both of which are extremely rich sources of stored retinol.
Acute or chronic poisoning can only be brought on by dietary supplements containing retinol. Acute toxicity happens following a single or brief dosage over 150,000 µg. Within 8 to 24 hours, symptoms include headache, nausea, vomiting, dizziness, and blurred vision. hours.
Babies between the ages of 0 and 6 months who were given an oral dose to prevent the development of a vitamin A deficit showed signs of a bulging skull fontanel after 24 hours, which normally ended by 72.
Long-term vitamin A ingestion at dosages of 25,000–33,000 IU/day for several months may result in chronic toxicity. Even at lesser dosages, excessive alcohol use can cause persistent toxicity.
Nervous system effects, liver abnormalities, exhaustion, muscle weakness, alterations in the skin and bones, and others are possible symptoms. When ingestion is ceased, the negative effects of both acute and chronic toxicity are reversed.
The US Institute of Medicine evaluated three main adverse effects in 2001 in order to determine ULs for adults, and ultimately decided on two: teratogenicity, or the ability to cause birth defects and liver problems.
Decreased bone mineral density was taken into consideration but discarded due to inconsistent human data. Retinol consumption in excess of 4,500 µg/day during pregnancy, particularly in the first trimester, raised the risk of birth abnormalities but not below that level, establishing a “No-Observed Adverse-Effect Level” (NOAEL).
Considering the caliber of the clinical trial evidence, the UL for women of reproductive age was determined to be 3,000 µg/day of preformed vitamin A by dividing the NOAEL by an uncertainty factor of 1.5.
When intakes were above 14,000 µg/day, liver problems were observed in all other people. Owing to the low quality of the clinical data, the UL was set at 3,000 µg/day with rounding using an uncertainty factor of 5.
Even though the US UL is set at 3,000 µg, dietary supplement items that are sold over-the-counter include a label warning “Not intended for long-term use unless under medical supervision” and have 7,500 µg (25,000 IU).
The US Institute of Medicine evaluated three main adverse effects in 2001 in order to determine ULs for adults, and ultimately decided on two: teratogenicity, or the ability to cause birth defects and liver problems.
Decreased bone mineral density was taken into consideration but discarded due to inconsistent human data. Retinol consumption in excess of 4,500 µg/day during pregnancy, particularly in the first trimester, raised the risk of birth abnormalities but not below that level, establishing a “No-Observed Adverse-Effect Level” (NOAEL).
The NOAEL was divided by an uncertainty factor of 1.5, taking into account the quality of the clinical trial evidence, to determine the UL for women of reproductive age to be 3,000 µg/day of performed vitamin A.
When intakes were above 14,000 µg/day, liver problems were observed in all other people. Owing to the low quality of the clinical data, the UL was set at 3,000 µg/day with rounding using an uncertainty factor of 5.
Even though the US UL is set at 3,000 µg, dietary supplement items that are sold over-the-counter include a label warning “Not intended for long-term use unless under medical supervision” and have 7,500 µg (25,000 IU).
After accounting for relative body weight, the adult value was used to extrapolate the ULs for children. Following prolonged intake of 6,000 or more µg/day, some case studies of newborns reported severe effects such as skin peeling, increased intracranial pressure, loss of appetite, and bulging fontanels.
Owing to the limited database, a UL of 600 µg/day was obtained by dividing the uncertainty factor of 10 by the “Lowest-Observed-Adverse-Effect Level” (LOAEL).
ß-carotene safety
Eating foods high in ß-carotene has not been linked to any negative effects other than carotenemia. Taking ß-carotene supplements does not result in hypervitaminosis A.
Two large-scale clinical trials (ATBC and CARET) investigated whether yearly supplementation with oil-filled capsules containing 20 or 30 mg of ß-carotene would lower the incidence of lung cancer in tobacco users.
These trials were conducted because greater ß-carotene diets were associated with a decreased incidence of lung cancer in tobacco smokers, according to observational research.
Remarkably, this high-concentration ß-carotene supplementation led to an increase in both overall mortality and lung cancer incidence.
The U.S. Institute of Medicine determined not to establish a Tolerable Upper Intake Level (UL) for ß-carotene after taking this and other data into account.
Additionally, the European Union opted against setting a UL for ß-carotene through the European Food Safety Authority.
Carotenosis
A surplus of dietary carotenoids causes the outermost layer of skin to turn orange in a benign and reversible medical disorder known as carotenoderma, also called carotenemia.
It is linked to elevated blood levels of ß-carotene. This can happen after consuming foods high in beta-carotene, like carrot juice, tangerine juice, mangos, and, in Africa, red palm oil, for a month or two.
Supplemental ß-carotene in food can also have the same effect. The illness can be distinguished from jaundice by the discoloration that affects the palms and soles of the feet but not the whites of the eyes.
It has been established that chronic consumption of more than 30 mg/day causes carotenemia.
U.S. labeling
To comply with U.S. regulations for food and dietary supplement labeling, the quantity in a serving is stated as a percentage of Daily Value (%DV).
100% of the Daily Value for vitamin A labeling was originally set at 5,000 IU, but on May 27, 2016, it was changed to 900 µg RAE. Reference Daily Intake provides a table with the current and old adult daily values.
Sources
Many foods contain vitamin A. Vitamin A can be found in food in two different forms: provitamin A carotenoids, which are plant pigments that are digested into vitamin A after consuming carotenoid-rich plant foods and are typically red.
Orange, or yellow in color; or preformed retinol, an active form of vitamin A found in animal liver, dairy, and egg products, as well as some fortified foods. Chlorophylls can cover up carotenoid pigments in dark green.
| FODD | μg RAE (2001) per 100 g |
| cod liver oil | 30,000 |
| beef liver (cooked) | 4,970 — 21,145 |
| chicken liver (cooked) | 4296 |
| butter (stick) | 684 |
| cheddar cheese | 316 |
| egg (cooked) | 140 |
veggies with leaves, like spinach. Plant-food carotenoids have a relatively poor bioavailability due in part to their binding to proteins; nevertheless, chopping, homogenizing, or boiling the plant proteins causes disruptions that increase the bioavailability of provitamin A carotenoid.
If a diet includes foods high in carotenoids, such as carrots, spinach, kale, and sweet potatoes, it can supply enough vitamin A in the form of provitamin A carotenoids for vegetarians and vegans. In the United States, the typical daily consumption of ß-carotene falls between 2 and 7 mg.
Certain processed foods and dietary supplements include beta-carotene or vitamin A.
Some firms sell vitamin A (retinal palmitate) as a dietary supplement with doses up to 7,500 µg/day, even though the US has set an upper limit of 3,000 µg/day. WonderLabs and Pure Prescriptions are two such.
Fortification
Certain nations mandate or suggest the fortification of food items. As of January 2022, food fortification of cooking oil, rice, wheat flour, or maize (corn) flour with vitamin A (often as retinyl palmitate or retinyl acetate) is required in 37 countries, the majority of which are in Sub-Saharan Africa.
Examples include 11.7 mg/kg of oil from Pakistan and 6 mg/kg of oil from Nigeria, as well as 2 mg/kg of wheat and maize flour. Twelve other nations, primarily in Southeast Asia, have optional fortification programs. For instance, the Indian government suggests 7.95 mg/kg of oil and 0.626 mg/kg of rice and wheat flour, respectively.
But compared to nations where fortification is required, voluntary fortification countries have lower compliance rates. Europe and North America do not fortify food with vitamin A.
Different from fortifying food by adding artificial vitamin A, genetic engineering methods of food fortification have been investigated.
In 1982, research on rice was started. In 2004, golden rice cultivars were subjected to their first field testing. Using genetic engineering, “Golden Rice” was created—a type of Oryza sativa rice that allows rice’s edible sections to biosynthesize beta-carotene, a precursor to retinol.
Regulatory bodies from the US, Canada, Australia, and New Zealand decided in May 2018 that Golden Rice complied with food safety regulations. The Philippines was the first nation to formally grant biosafety authorization for the commercial cultivation of Golden Rice on July 21, 2021.
However, the Department of Agriculture was ordered to cease the commercial distribution of genetically modified rice in the Philippines by the Supreme Court of the Philippines in a Writ of Kalikasan granted in April 2023.
Vitamin A Supplementation (VAS)
Oral high-dose supplement delivery continues to be the major method for reducing deficiency. As of 2017, semi-annual national campaigns in more than 80 nations are introducing universal VAS programs for children aged 6 to 59 months.
The dosages for these programs consist of one dose every four to six months of 50,000 or 100,000 IU for children ages 6 to 11 months and 100,000 to 200,000 IU for children ages 12 months to five years.
| FOOD | μg RAE (2001) per 100 g |
| Sweet potato, baked, no added fat | 957 |
| Carrot, frozen, cooked, no added fat | 843 |
| Pumpkin, canned, cooked | 767 |
| Spinach, fresh, cooked, no added fat | 341 |
| Kale, fresh, cooked, no added fat | 245 |
Deficiency
Primary causes
In underdeveloped nations, particularly in Sub-Saharan Africa and Southeast Asia, vitamin A insufficiency is prevalent.
Although deficiency can strike at any age, it most frequently affects preschool-aged children and expectant mothers, the latter of whom must transfer retinol to the developing fetus.
The reasons are low consumption of foods high in carotene from plants and foods high in retinol from animals.
An estimated one-third of children under five worldwide are thought to be affected by vitamin A deficiency, which may result in the deaths of 670,000 children under five each year.
Due to vitamin A deficiency, between 250,000 and 500,000 children in developing nations go blind every year.
UNICEF states that “the leading cause of preventable childhood blindness” is a vitamin A deficiency.
Additionally, it raises the chance of dying from common pediatric illnesses like diarrhea. As the fourth of the UN’s Millennium Development Goals, lowering child mortality, UNICEF believes that treating vitamin A deficiency is essential.
Night blindness and dry eyes are diagnostic indicators of vitamin A deficiency that can be identified without the need for biochemical testing.
To verify the presence of vitamin A, plasma retinol is employed. A normal plasma concentration is around 2.0 µmol/L; a moderate vitamin A deficit is indicated by less than 0.70 µmol/L (or 20 µg/dL); a severe vitamin A deficiency is indicated by less than 0.35 µmol/L (10 µg/dL).
Retinol in breast milk less than 8 µg/gram Fat is regarded as inadequate. The fact that retinyl esters in hepatic stellate cells are better markers of liver vitamin A reserves than these measurements is one of their weaknesses.
As long as there are adequate liver reserves, the amount of vitamin A that is bound to retinol-binding protein (RBP) and leaves the liver is tightly regulated.
The blood concentration of vitamin A will only decrease when the liver content falls below 20 µg/gram.
Secondary causes
Other than inadequate dietary intake of vitamin A, deficiencies can also result from low levels of retinol or carotenes. For retinol to be mobilized and exit the liver, a normal rate of synthesis of RBP requires an adequate intake of protein and calories from food.
Even in the absence of protein-calorie deprivation, systemic infections can result in brief reductions in RBP production. Chronic alcohol use decreases the amount of vitamin A stored in the liver.
Fat buildup in the liver is the hallmark of non-alcoholic fatty liver disease (NAFLD), which is the hepatic expression of metabolic syndrome.
The ability of the liver to mobilize hepatic reserves to maintain a normal circulation concentration of retinol is diminished by liver damage resulting from nonalcoholic fatty liver disease (NAFLD).
Animal Requirements
Every species of chordate and vertebrate needs vitamin A, which comes from eating other animals or from dietary carotenoids that are already converted to retinol.
Deficits have been documented in pets, dogs, cats, birds, reptiles, amphibians, and commercially bred chickens and turkeys as well as in laboratory-grown animals.
Herbivore animals like sheep, cattle, and horses can obtain enough ß-carotene from green pasture to be healthy, but long-stored hay and pasture grass that has dried up from drought can have insufficient amounts of the vitamin, which can result in vitamin A deficiency.
Species that are both omnivores and carnivores, particularly those at the top of the food chain, have the ability to store significant quantities of retinyl esters in their livers or, in the event of a surplus, expel retinyl esters in urine. The high-vitamin A and D content of cod liver oil made it a popular nutritional supplement before the invention of synthetic retinol.
Because they are unable to produce retinol or carotenoids, invertebrates must obtain these vital nutrients by eating algae, plants, or animals.
Medical uses
Preventing and treating deficiency
Governments and non-governmental groups are pushing food fortification with vitamin A and developing programs that provide young children substantial bolus-size oral doses of vitamin A every four to six months due to the awareness of its prevalence and implications.
In 40 nations over a ten-year period, vitamin A supplementation prevented 1.25 million deaths from vitamin A insufficiency, according to estimates made by the World Health Organization in 2008.
According to a Cochrane analysis, vitamin A supplementation is linked to a clinically significant decrease in morbidity and death in kids between the ages of six months and five. Diarrhea occurrences were decreased by 12% and overall-cause death by 14%.
The same group did, however, declare in a Cochrane review that there was insufficient evidence to support the widespread recommendation of vitamin A supplementation for newborns between the ages of one and six months, as it did not lower infant mortality or morbidity.
Oral retinoic acid
It has been demonstrated that retinoic acid (RA) taken orally in the forms of all-trans-tretinoin or 13-cis-isotretinoin improves the health of the facial skin by activating genes and transforming keratinocytes, or immature skin cells, into mature epidermal cells.
Bacteria in the ducts and on the skin’s surface are decreased as a result of RA’s reduction of sebaceous gland size and secretion. By inhibiting the chemotactic reactions of neutrophils and monocytes, it lowers inflammation.
Isotretinoin was introduced to the US market in 1982 as a ground-breaking remedy for severe and unresponsive acne vulgaris.
It was displayed. that sebum excretion can be reduced by 90% in a month or two with a daily dose of 0.5–1.0 mg/kg body weight; however, a 4- to 6-month course of treatment is advised.
As a well-known teratogen, isotretinoin exposes fetuses to an estimated 20–35% risk of physical birth defects, including a wide range of congenital conditions such as thymic diseases, cardiovascular and neurological deformities, and craniofacial anomalies.
The percentage of people with neurocognitive deficits who do not have any physical deformities is 30–60%.
These factors led to the creation of physician and patient education programs, which advised women of childbearing age to begin contraception one month prior to beginning oral (or topical) isotretinoin and to continue it for another month following the completion of therapy.
Researchers have looked into off-label applications for dermatological disorders like rosacea, psoriasis, and other conditions in addition to the approved use for treating acne vulgaris.
It has been observed that rosacea responds well to dosages lower than those used for acne. It has been demonstrated that isotretinoin plus UV radiation is an effective combo for treating psoriasis.
Injectable interferon-alpha combined with isotretinoin showed some promise in the treatment of vaginal warts. Combining isotretinoin with injectable interferon-alpha or topical fluorouracil has some promise for treating skin cancer and precancerous skin lesions.
Topical Retinoic Acid and Retinol
Prescription topical drugs called retinoic acids, such as tretinoin (all-trans-retinoic acid) and isotretinoin (13-cis-retinoic acid), are used to treat moderate to severe cystic acne and acne that is not improving with previous therapies.
After cleansing, they are typically applied to the face as a skin cream to get rid of makeup and skin oils. The mechanisms by which retinoids and tretinoin bind to keratinocytes’ two nuclear receptor families are the receptors for retinoic acid (RAR) and retinoid X (RXR).
Reduced follicular occlusion and microcomed one development are the outcomes of these processes, which also help to normalize follicular keratinization and keratinocyte cohesiveness.
A crucial transcription factor implicated in inflammation, AP-1, has coactivator proteins that the retinoid-receptor complex competes for. Retinoic acid products help lessen the amount of sebum secreted from facial pores, which provides bacteria with nutrients.
Because animal reproduction studies have demonstrated a harmful effect on the fetus, these pharmaceuticals are classified as Pregnancy Category C in the US and should not be used by women who are pregnant or planning to become pregnant.
Pregnancy prevention policies involving patient and physician education have been implemented in several nations.
A prescription retinoid called trifarotene is used as a topical therapy for acne vulgaris. It is an agonist of the retinoic acid receptor (RAR)-?.
Retinyl palmitate is frequently included in over-the-counter topical medications that make health claims about how well they can treat dark spots on the skin, lessen wrinkles and lines brought on by age, and reduce facial acne.
According to the theory, this is absorbed, desertified, and converted to free retinol. It then undergoes additional metabolism to become retinaldehyde and all-trans-retinoic acid, which is where it gets similar effects to prescription medications with fewer adverse effects.
Ex vivo data involving human skin suggests that esterified retinol is absorbed and subsequently transformed into retinol. Some of these products contain hydroxypinacolone retinoate, also known as esterified 9-cis-retinoic acid, in addition to esterified retinol.
Synthesis
Biosynthesis
Bacteria, some fungi, and plants all synthesize carotenoids. Because of their structural similarity, carotenes are classified as tetraterpenes. This means that they are produced biochemically from four 10-carbon terpene units, which were first generated from eight 5-carbon isoprene units.
The formation of a 40-carbon phytoene molecule, its desaturation to lycopene, and the subsequent synthesis of ionone rings at both ends of the molecule are intermediate stages.
Because ß-carotene possesses a ß-ionone ring on both ends, it can split symmetrically into two molecules of retinol. With a ?-ionone ring at one end and a ß-ionone ring at the other, a-carotene has half the capacity of retinol.
Retinol is produced in the majority of animal species by the degradation of ß-carotene, a provitamin found in plants. The core double bond of ß-carotene is first broken by the enzyme beta-carotene 15,15′-dioxygenase (BCO-1), resulting in the formation of an epoxide.
Water subsequently attacks this epoxide, resulting in the formation of two hydroxyl groups in the structure’s middle. When NAD+ is used to convert these alcohols to aldehydes, the cleavage takes place.
The enzyme retinol dehydrogenase then swiftly converts the resulting retinal to retinol. In general, omnivore species like wolves, coyotes, foxes, and dogs create less BCO-1 than other species.
Because felids (cats) lack the enzyme, their needs for vitamin A are satisfied by the retinyl ester content of prey animals.
Industrial synthesis
Using xylose as a substrate, ß-carotene can be extracted from the fungus Blakeslea trispora, marine algae Dunaliella salina, or genetically modified yeast Saccharomyces cerevisiae. Hoffman-La Roche’s Grignard reaction or a technique created by BASF are both used in chemical synthesis.
Around 13% of the global market for synthetic retinol is made up of people who use it for dietary supplements, prescription drugs, and animal feed.
Chemical synthesis is the basis for industrial retinol manufacturing methods. Hoffmann-La Roche created the first industrialized synthesis of retinol in 1947. Eight more businesses created their own procedures throughout the ensuing decades.
ß-ionone, produced from acetone serves as the foundation for all industrial syntheses. In every phase, the unsaturated carbon chain is extended. Pure retinol is manufactured and transported in low-temperature, oxygen-free environments due to its great sensitivity to oxidation.
Retinol is stabilized as the ester derivatives retinyl acetate or retinyl palmitate when it is produced as a food additive or dietary supplement. Before 1999, three businesses, Rhone-Poulenc, BASF, and Roche accounted for 96% of vitamin A sales worldwide.
These and five other businesses were fined a total of 855.22 million euros by the European Commission in 2001 for their involvement in eight different market-sharing and price-fixing cartels that began in 1989.
In 2003, Roche sold its vitamin division to DSM. The two companies that produce the most industrially are DSM and BASF.
An alternate method of biosynthesis uses Saccharomyces cerevisiae, a genetically modified yeast species, to produce retinol and retinal utilizing xylose as the initial substrate.
To achieve this, the yeast first produced ß-carotene, which was subsequently broken down by the cleaving enzyme ß-carotene 15,15′-dioxygenase to produce retinal.
Research
Brain
Pre-clinical animal research on mice also showed that the bioactive metabolite of vitamin A, retinoid acid, affects the parts of the brain linked to learning and memory.
Cancer
Results from meta-analyses of observational and interventional trials for different cancer types are inconsistent.
Taking ß-carotene supplements did not seem to reduce the risk of cancer in general or any particular type of cancer, such as colorectal, prostate, breast, pancreatic, melanoma, or skin cancer. Unexpectedly, high-dose ß-carotene supplementation increased the risk of lung cancer and overall mortality in cigarette smokers.
Although the previous review did note a lower risk for higher beta-carotene consumption, there were no impacts of dietary retinol on breast cancer survival, risk of liver cancer, danger of bladder cancer, or risk of colorectal cancer.
On the other hand, retinol intake was found to be negatively correlated with the relative risk of lung cancer, melanoma, pancreatic cancer, ovarian cancer, esophageal cancer, and cervical cancer.
Apart from the retinol findings, there was also an inverse relationship between beta-carotene consumption and lung cancer.
The relative risk decreased by 15 to 20% when high dietary intake was contrasted with low dietary intake.
A meta-analysis of preventive trials found that retinol reduced the relative risk of stomach cancer by 29% 1500 µg of supplements each day.
Fetal alcohol spectrum disorder
Previously known as fetal alcohol syndrome, fetal alcohol spectrum disease (FASD) is characterized by mental impairments, neurobehavioral abnormalities, and craniofacial anomalies that are all linked to the exposure of human embryos to alcohol during fetal development.
Alcohol consumption during pregnancy is associated with a risk of FASD, which is determined by the quantity, frequency, and timing of alcohol consumption.
Birth malformations are known to be caused by ethanol, which is a teratogen. Alcohol dehydrogenase enzymes convert ethanol to acetaldehyde. Acetaldehyde’s subsequent oxidation Enzymes called aldehyde dehydrogenase convert carbon dioxide into acetate.
Competition for the enzymes needed for the manufacture of retinoic acid (RA) from vitamin A is one of the hypothesized mechanisms for the teratogenic effects of ethanol, given that RA regulates a number of embryonic and differentiating processes.
Research on animals indicates that acetaldehyde and retinaldehyde compete with one another for aldehyde dehydrogenase activity in the embryo. According to this idea, retinaldehyde dehydrogenase is inhibited by acetaldehyde in the process of producing retinoic acid.
Elevating retinol, retinaldehyde, or retinaldehyde dehydrogenase levels can help mitigate developmental abnormalities caused by ethanol. Therefore, evidence from animal studies supports the idea that retinoic acid activity decline is an etiological trigger for FASD induction.
Malaria
In sub-Saharan Africa, vitamin A deficiency and malaria are prevalent in young infants. It has been frequently demonstrated that providing vitamin A supplements to children in areas where vitamin A deficiency is prevalent lowers overall death rates, particularly those related to diarrhea and measles.
Clinical study outcomes for malaria are conflicting, either demonstrating that vitamin A treatment had no effect or did not diminish the likelihood of probable malarial fever. incidence, however, it did lower the number of fever episodes, and the parasite density was verified by slides.
It has been questioned whether vitamin A deficiency increases the risk of malaria, whether malaria itself causes vitamin A deficiency or both.
Researchers hypothesized a number of ways in which malaria (and other infections) might lead to a vitamin A deficiency, such as a fever-induced decrease in the production of retinal-binding protein (RBP), which is involved in the transfer of retinol from the liver to plasma and tissues.
However, they did not find any indication that plasma RBP or retinol levels would temporarily decline or recover after a malarial infection was treated.
In History
Frederick Gowland Hopkins showed in 1912 that milk included unidentified auxiliary substances that were required for rat growth in addition to carbs, proteins, and lipids.
Hopkins was awarded a 1929 Nobel Prize for this finding. One of these compounds was separately discovered by Lafayette Mendel and Thomas Burr Osborne at Yale University and Elmer McCollum and Marguerite Davis at the University of Wisconsin–Madison by 1913.
In the end, McCollum and Davis were given credit as they turned in their paper three weeks prior to Osborne and Mendel. In 1913, both papers were published in the Journal of Biological Chemistry in the same issue.
First referred to as “fat-soluble” in 1918, the phrase “accessory factors” was changed to “vitamin A” in 1920. A 1919 study by Harry Steenbock of the University of Wisconsin–Madison suggested a connection between vitamin A and beta-carotene, a pigment found in yellow plants.
molecular structure of vitamin A was described by Swiss chemist Paul Karrer in 1931. David Adriaan van Dorp and Jozef Ferdinand Arens, two Dutch scientists, were the first to synthesize retinoic acid and retinol in 1946 and 1947.
weeks prior to Osborne and Mendel. In 1913, both papers were published in the Journal of Biological Chemistry in the same issue.
First referred to as “fat-soluble” in 1918, the phrase “accessory factors” was changed to “vitamin A” in 1920. A 1919 study by Harry Steenbock of the University of Wisconsin–Madison suggested a connection between vitamin A and beta-carotene, a pigment found in yellow plants.
The molecular structure of vitamin A was described by Swiss chemist Paul Karrer in 1931. David Adriaan van Dorp and Jozef Ferdinand Arens, two Dutch scientists, were the first to synthesize retinoic acid and retinol in 1946 and 1947.
George Wald’s research on the chemical processes involved in vision in the eye earned him a share of the 1967 Nobel Prize in Physiology and Medicine.
Wald had shown in 1935 that rhodopsin, a chromophore made of the proteins opsin and 11-cis-retinal, is present in photoreceptor cells in the eye. When exposed to light, 11-cis retina photoisomerizes to the all-trans retina, which then sends a nerve signal to the brain through a signal transduction cascade.
After being reduced to all-trans-retinol, the all-trans-retinal returns to the retinal pigment epithelium where it is regenerated into 11-cis-retinal and then converted back to opsin. The result of almost 60 years of research was Wald’s work.
Franz Christian Boll discovered in 1877 that the outer segments of the retina’s rod cells contained a pigment that was light-sensitive and that, when exposed to light, bleached or faded but returned when the light source was cut off.
He proposed that this material gave the brain the impression of light through a photochemical mechanism. Wilhelm Kühne began investigating and gave the pigment’s name, rhodopsin—also referred to as “visual purple.” Kühne affirmed that Because rhodopsin is so sensitive to light, it allows vision in low light.
The chemical breakdown of rhodopsin activated nerve impulses in the brain. Research was halted until it was discovered that “fat-soluble vitamin A,” a dietary component present in milkfat but absent from lard, may correct xerophthalmia and night blindness.
Rats lacking in vitamin A were shown by Fridericia and Holm in 1925 to be incapable of regenerating rhodopsin when placed in a dark environment as opposed to a light one.
FAQ
What is vitamin A good for?
Normal growth and development, immunological function, reproduction, and vision all depend on vitamin A. Your heart, lungs, and other organs function better when vitamin A is present. Carotenoids are pigments that give fruits and vegetables their colors—yellow, orange, and red
Which food is highest in vitamin A?
The highest preformed vitamin A concentrations are found in dairy products, fish, eggs, and liver. Leafy green vegetables, orange and yellow vegetables, tomato products, fruits, and certain vegetable oils provide the majority of the dietary provitamin A in the American diet.
What is vitamin A for the skin?
For the treatment of severe acne and psoriasis, prescription creams and pills containing retinoids—a synthetic version of vitamin A—are utilized. Additionally, they have demonstrated promise in the treatment of warts, certain skin conditions, and sun-induced premature aging.
Which fruit gives vitamin A?
Mangos, papayas, various squashes, carrots, sweet potatoes, and maize (not the white kinds) are examples of plant sources of vitamin A. Red palm oil and biruti palm oil are two more excellent sources of vitamin A. (Note: Vitamin A is degraded if these oils are cooked to remove their color.)
How much vitamin A per day?
The unit of measurement for a food’s total vitamin A content is typically micrograms (µg) of retinol equivalents (RE). Men who are between the ages of 19 and 64 require 700 µg of vitamin A each day. 600 µg daily for females.
Which vitamin is good for eyes?
Having healthy eyesight requires vitamin A. It is a part of the rhodopsin protein, which gives the eye the ability to see in dim light. Night blindness can result from a vitamin A shortage, according to the American Academy of Ophthalmology.




2 Comments