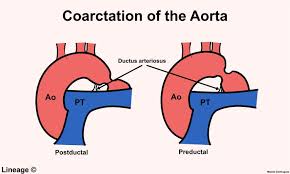
Coarctaction of Aorta
Coarctation (ko-ahrk-TAY-shun) of the aorta — or aortic coarctation — is a narrowing of the aorta, the large blood vessel that branches off your heart and delivers oxygen-rich blood to your body. When this occurs, your heart must pump harder to force blood through the narrowed part of your aorta.
Coarctation of the aorta is generally present at birth (congenital). The condition can range from mild to severe, and might not be detected until adulthood, depending on how much the aorta is narrowed.
Coarctation of the aorta often occurs along with other heart defects. While treatment is usually successful, the condition requires careful lifelong follow-up.
SYMPTOMS
Coarctation of the aorta symptoms depend on the severity of the condition. Most people don’t have symptoms. Children with serious aortic narrowing may show signs and symptoms earlier in life, but mild cases with no symptoms might not be diagnosed until adulthood. People may also have signs or symptoms of other heart defects that they have along with coarctation of the aorta.
Babies with severe coarctation of the aorta may begin having signs and symptoms shortly after birth. These include:
Pale skin
Irritability
Heavy sweating
Difficulty breathing
Difficulty feeding
Left untreated, aortic coarctation in babies might lead to heart failure or death.
Older children and adults with coarctation of the aorta often don’t have symptoms because their narrowing may be less severe. If you have signs or symptoms that appear after infancy, you most commonly will have high blood pressure (hypertension) measured in your arms. However, your blood pressure is likely to be lower in your legs. Signs and symptoms might include:
High blood pressure
Headache
Muscle weakness
Leg cramps or cold feet
Nosebleeds
Chest pain
When to see a doctor
Seek medical help if you or your child has the following signs or symptoms:
Severe chest pain
Fainting
Sudden shortness of breath
Unexplained high blood pressure
While experiencing these signs or symptoms doesn’t necessarily mean that you have a serious problem, it’s best to get checked out quickly. Early detection and treatment might help save your life.
CAUSES
Doctors aren’t certain what causes coarctation of the aorta (aortic coarctation). For unknown reasons, mild to severe narrowing develops in part of the aorta. Although aortic coarctation can occur anywhere along the aorta, the coarctation is most often located near a blood vessel called the ductus arteriosus. The condition generally begins before birth (congenital). Congenital heart defects are the most common of all birth defects.
Rarely, coarctation of the aorta develops later in life. Traumatic injury might lead to coarctation of the aorta. Rarely, severe hardening of the arteries (atherosclerosis) or a condition causing inflamed arteries (Takayasu’s arteritis) can narrow the aorta, leading to aortic coarctation.
Coarctation of the aorta usually occurs beyond the blood vessels that branch off to your upper body and before the blood vessels that lead to your lower body. This can often lead to high blood pressure in your arms but low blood pressure in your legs and ankles.
With coarctation of the aorta, the lower left heart chamber (left ventricle) of your heart works harder to pump blood through the narrowed aorta, and blood pressure increases in the left ventricle. This may cause the wall of the left ventricle to thicken (hypertrophy).
RISK FACTORS
Coarctation of the aorta often occurs along with other congenital heart defects, although doctors don’t know what causes multiple heart defects to form together. The condition is more common in males than in females. You or your child may be more likely to have aortic coarctation if certain heart conditions exist, including:
1.Bicuspid aortic valve. The aortic valve separates the lower left chamber (left ventricle) of the heart from the aorta. A bicuspid aortic valve has two flaps (cusps) instead of the usual three. Many people with coarctation of the aorta have a bicuspid aortic valve.
Patent ductus arteriosus. Before birth, the ductus arteriosus is a blood vessel connecting the left pulmonary artery to the aorta — allowing blood to bypass the lungs.
Shortly after birth, the ductus arteriosus usually closes. If it remains open, it’s called a patent ductus arteriosus.
Holes in the wall between the left and right sides of the heart. You may have a hole in the wall (septum) between the upper chambers of the heart (atrial septal defect) or the lower chambers of the heart (ventricular septal defect) when you’re born.
This causes oxygen-rich blood from the left side of the heart to mix with oxygen-poor blood in the right side of the heart.
2.Aortic valve stenosis. This is a narrowing of the valve that separates the left ventricle of the heart from the aorta (aortic valve). This means your heart has to pump harder to get adequate blood flow to your body.
Over time, this can cause your heart muscle to thicken and lead to symptoms such as chest pain, fainting spells and breathlessness, or heart failure.
3.Aortic valve regurgitation. This occurs when the aortic valve doesn’t close tightly, causing blood to leak backward into the left ventricle.
Mitral valve stenosis. This is a narrowing of the valve (mitral valve) between the upper left heart chamber (left atrium) and the left ventricle that lets blood flow through the left side of your heart.
In this condition, blood may back up into your lungs, causing shortness of breath or lung congestion. Like aortic valve stenosis, this condition can also lead to heart failure.
4.Mitral valve regurgitation. This occurs when the mitral valve doesn’t close tightly, causing blood to leak backward into the left atrium.
Coarctation of the aorta is also more common in people who have certain genetic conditions, such as Turner syndrome. Women and girls with Turner syndrome have 45 chromosomes, with one missing or incomplete X chromosome, instead of 46. About 10 percent of women and girls with Turner syndrome have aortic coarctation.
COMPLICATIONS
Untreated coarctation of the aorta frequently leads to complications. Some complications may be a result of long-standing high blood pressure caused by the aortic coarctation. Complications are also possible after treatment for coarctation of the aorta.
Complications of coarctation of the aorta may include:
Narrowing of the aortic valve (aortic stenosis)
High blood pressure
Stroke
Enlargement in a section of the wall of the aorta (aneurysm)
Aortic rupture or tear (dissection)
Premature coronary artery disease — narrowing of the blood vessels that supply the heart
Heart failure
A weakened or bulging artery in the brain (brain aneurysm) or bleeding in the brain (hemorrhage)
In addition, if the coarctation of the aorta is severe, your heart might not be able to pump enough blood to your other organs. This can cause damage to your heart and also can result in kidney failure or other organ failure.
If your coarctation of the aorta was treated when you were young, you have a risk of the aorta re-narrowing (re-coarctation) over time. You also have a higher risk of developing high blood pressure. You will need lifelong follow-up for coarctation of the aorta, and you may require additional treatments.
PREVENTION
Coarctation of the aorta can’t be prevented, because it’s usually present at birth (congenital). However, if you or your child has a condition that increases the risk of aortic coarctation, such as Turner syndrome, bicuspid aortic valve or another heart defect, or a family history of congenital heart disease, early detection can help.
PHYSIOTHERAPY IN PRE- AND POSTOPERATIVE PERIOD
Physiotherapy in the pre- and postoperative period is indicated in pediatric cardiac surgery in order to reduce the risk of pulmonary complications (retention of secretions, atelectasis and pneumonia) as well as to treat such complications as it contributes to the appropriate ventilation and successful extubation .
In the preoperative, physiotherapy uses techniques of clearance, reexpansion, abdominal support and guidance on the importance and objectives of physiotherapy intervention for parents or escorts, or patients able to understand such guidance . The techniques used by postoperative physiotherapy include vibration in the chest wall, percussion , compression , manual hyperinflation , reexpansion maneuver , positioning postural drainage , cough stimulation, aspiration , breathing exercises , mobilization and AEF (acceleration of expiratory flow) .
There are few current studies on the role of physiotherapy in the postoperative of pediatric cardiac surgery , especially those that approach the effectiveness of physiotherapy in the preoperative to prevent pulmonary complications after heart surgery.
Felcar et al. performed a study with 141 children with congenital heart disease, aged varying between one day old to six years, randomly divided into two groups, whereas one of them received physiotherapy in the pre- and postoperative and the other only postoperatively. The study obtained statistically significant difference regarding the presence of pulmonary complications (pneumonia and atelectasis), being more frequent in the group undergoing physiotherapy only postoperatively. Moreover, when the presence of pulmonary complications was associated with other complications regarding the time of hospital stay, such as sepsis, pneumothorax, pleural effusion and others, the group that received physiotherapy before and after surgery showed a lower risk of developing such complications. These findings demonstrate the importance of preventive action of physiotherapy preoperatively.
The study by Main et al. compared the effectiveness of aspiration with the techniques of respiratory physiotherapy (manual vibration, percussion, compression, manual hyperinflation, positioning and postural drainage) in 83 participants with a mean age of 9 months. The respiratory parameters (expiratory tidal volume, resistance and lung compliance) were measured 15 minutes before treatment and after 30 minutes, and lasting for 60 minutes after the intervention in case there was no need for clinical intervention. The duration of physiotherapy was higher than the aspiration . It was observed that physiotherapy tends to produce improvement in expiratory tidal volume, pulmonary compliance and pulmonary resistance.
According to Kavanagh , the treatment for atelectasis consists of physiotherapy, deep breathing, incentive spirometry. However, sometimes, atelectasis is difficult to reverse and it is necessary association with another method, as in the case report from Silva et al. , in which a child with congenital heart disease underwent heart surgery and developed this pulmonary complication after extubation in the postoperative period and the reversal of this presentation was achieved after the association of respiratory physiotherapy with inhalation of hypertonic saline solution with NaCl at 6%.
Chest radiographs and four physiotherapy sessions lasting 20 minutes were performed daily in this study, using maneuvers of pulmonary reexpansion and bronchial hygiene, bronchial postural drainage and tracheal aspiration. Immediately before and after physiotherapy inhalation of hypertonic saline solution with NaCl at 6% was associated. The authors found that this association was shown to be effective in this case .
Breathing exercises are indicated in cases of atelectasis due to thoracic or upper abdominal surgery, because they improve the respiratory efficiency, increase the diameter of the airways, which helps to dislodge secretions, preventing alveolar collapse, and facilitating the expansion of the lung and peripheral airways clerance .
Campos et al. analyzed the effect of increased expiratory flow (IEF) in heart rate, respiratory rate and oxygen saturation in 48 children diagnosed with pneumonia. The variables were assessed before physiotherapy, in the first and fifth minutes after physiotherapy. The authors found a statistically significant increase in oxygen saturation and statistically significant reduction in cardiac and respiratory rate after intervention with IEF and concluded that this physiotherapeutic technique for bronchial hygiene is effective in improving lung function.




2 Comments