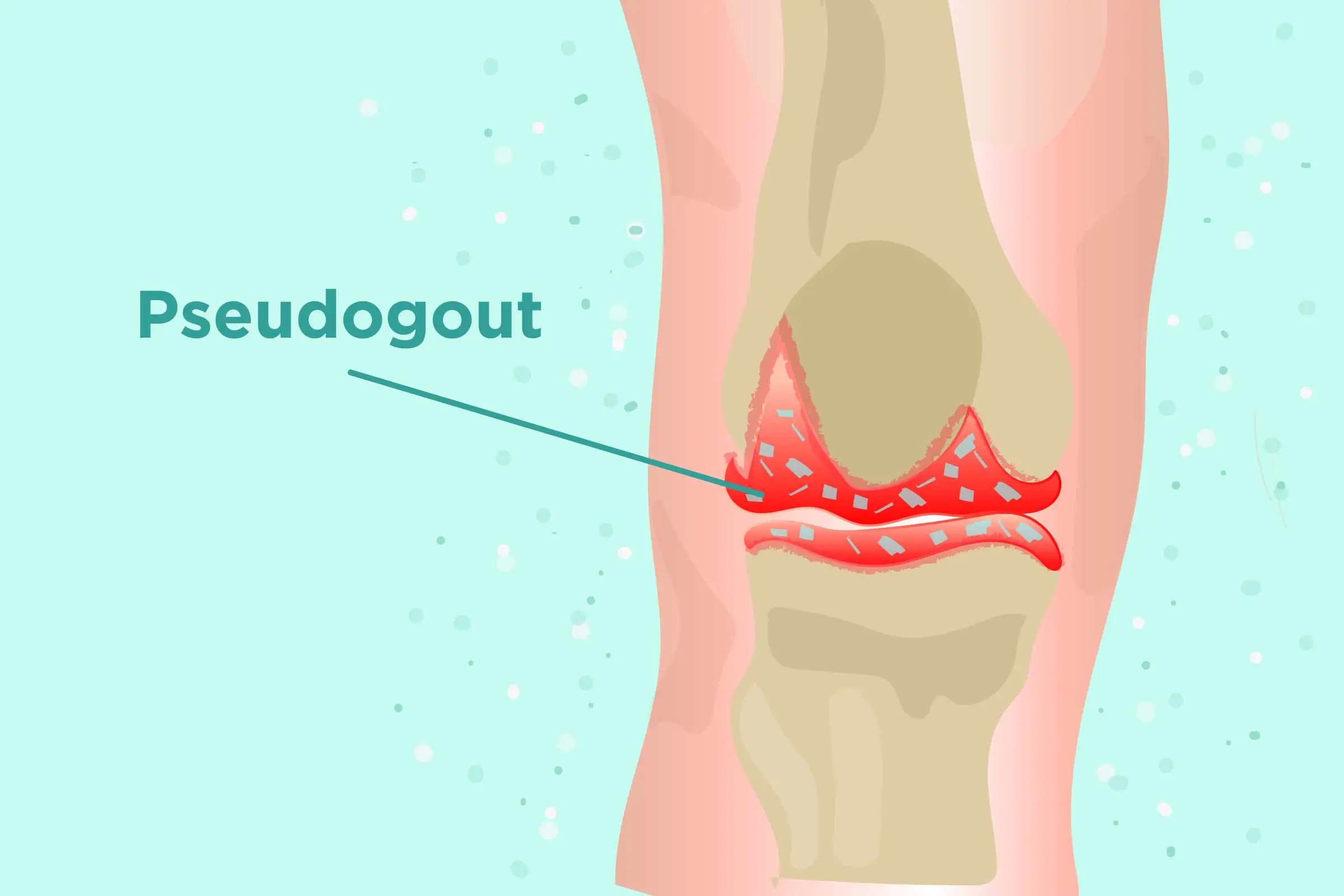
Pseudogout
What is Pseudogout?
Pseudogout is a type of arthritis that causes spontaneous, aching swelling in your joints. It occurs when crystals form in the synovial fluid, the fluid that lubricates the joints. This conducts to inflammation and ache. This disease most frequently involves the knee joints, but it can also affects other joints. It’s more commonly seen in grown-ups over the age of 60.
Pseudogout is also called a calcium pyrophosphate deposition (CPPD) condition. Doctors or physicians may refer to pseudogout as calcium pyrophosphate deposition (CPPD) or acute calcium pyrophosphate crystal arthritis (acute CPP crystal arthritis).
What Is Calcium Pyrophosphate Deposition (CPPD) Disease?
Pseudogout is only one form of calcium pyrophosphate deposition (CPPD) condition. A patient who has calcium pyrophosphate crystals (CPP crystals) in one or more joints or junctions is considered to have CPPD disorder.
Specialists evaluate that 7% to 10% of the population has some form of calcium pyrophosphate deposition – CPPD disorder. The specific forms of the disease contain:
Acute CPP crystal inflammatory arthritis (pseudogout)
This form of calcium pyrophosphate deposition – CPPD induces an immune response that results in severe pain, sudden, redness, swelling, warmth, as well as other probable symptoms. It generally involves fewer than 5 joints or junctions.
Chronic CPP crystal inflammatory arthritis
This form of calcium pyrophosphate deposition – CPPD activates a less intense immune system reaction than pseudogout. It results in chronic, mild, dull pain with some swelling and redness. Chronic calcium pyrophosphate – CPP arthritis can involve one too many joints or junctions. It is most probable to involve the shoulders, wrists, large knuckles, or feet. The symptoms are frequently similar to osteoarthritis or rheumatoid arthritis (pseudo-RA).
Non-symptomatic CPPD disease
Calcium pyrophosphate crystals may be present in a joint or junction but cause no ache. Many patients have no symptoms and are not familiar they have calcium pyrophosphate deposition – CPPD.
How Does CPPD Disease Cause Symptoms?
While specialists have known about calcium pyrophosphate crystals for decades, a study has yet to discover precisely why some patients develop calcium pyrophosphate deposition – CPPD disorder or why some patients experience symptoms and others do not.
Many experts recommend the following steps happen:
Calcium pyrophosphate crystals are made within a joint’s or junction’s cartilage. They can form when too greatly inorganic pyrophosphate (PPi), a combination naturally found in cartilage, collects. The extra PPi binds with calcium, leading to the building of crystals.
This cascade of events may happen because of:
Inaccurate metabolism within the cartilage itself
A more general metabolic disease that is not separated from cartilage. (A systemic metabolic disease involves the body’s capability to process and soak nutrients.)
An endocrine disease, which involves the body’s capability to make hormones.
As calcium pyrophosphate – CPP crystals continue to develop, they collect in the cartilage.
The extra calcium pyrophosphate – CPP crystals may be discharged from the cartilage. This release may occur if the cartilage is upset via normal wear-and-tear, trauma, injury, surgery, or infection.
The released calcium pyrophosphate – CPP crystals enter the joint or junction fluid. (Most joints or junctions are encapsulated by a thin membrane, which creates lubricating joint or junction fluid.) The loose crystals can then lodge in the surrounding soft joint or junction tissue, like the joints or junctions synovial lining, ligaments, bursa, and tendons.
Once accommodated in the joints or junctions soft tissue(s), the calcium pyrophosphate – CPP crystals activate an immune system reaction. This immune system reaction creates pain, inflammation, redness, swelling, and warmth, which may be analyzed as either pseudogout or chronic calcium pyrophosphate – CPP crystal inflammatory arthritis.
What causes pseudogout
Precisely why some patients bring pseudogout and others do not is unknown. Specialists do know several factors can raise and reduce a person’s risk for the condition, which can happen when calcium pyrophosphate (CPP) crystals accumulate in the soft tissues of a junction or joint.
Risk factors
The subsequent risk factors are associated with higher rates of pseudogout, which may be known as calcium pyrophosphate deposition – CPPD condition or acute calcium pyrophosphate – CPP crystal inflammatory arthritis. Unlike gout, pseudogout is not affected by diet, sex, or ethnicity.
Most of these risk factors, like age and genetics, cannot be altered. Underlying diseases that raise risk may be managed with therapy.
Age
Calculations differ regarding how many patients have calcium pyrophosphate crystal deposition, but investigators know for certain that risk rises dramatically with age.
Most patient who creates pseudogout is 60 or older. In reality, after age 60, the probability of creating pseudogout doubles per decade of life. In one often-cited analysis, 3 of 100 patients revealed to a geriatric unit saw signs of pseudogout in the joints or junctions of 44% of patients aged 84 or more senior, though not all the patients saw symptoms.
Joint trauma
A joint or junction injury or surgery can activate a pseudogout flare-up. Specialists theorize this occurs because trauma can cause joint or junction cartilage to discharge the calcium phosphate crystals that have been collected within it. Once discharged, the crystals trigger an immune system reaction that leads to swelling and further pseudogout symptoms.
Family history
Genetics plays a part, making some patients more prone to collecting calcium pyrophosphate crystals in their joints or junctions.
Recent analysis indicates that certain mutations in the ANKH gene, which assists to control metabolism, raise the risk of creating pseudogout. Patients with these genetic mutations are:
More probable to generate pseudogout at an earlier age
More probable to experience calcium pyrophosphate deposition – CPPD-related back ache and issues in the spine
While the CPPD condition is fairly familiar, calcium pyrophosphate deposition – CPPD condition caused by the ANKH gene is considered irregular. Further genes may also play a part in the growth of calcium pyrophosphate deposition – CPPD condition.
A patient who is analyzed with gout is almost 2.5 times more probable to create pseudogout.
Osteoarthritis
Study indicates that calcium pyrophosphate – CPP crystals are 2 to 3 times more familiar in persons who have osteoarthritis than those who do not. Some specialists believe that patients who have osteoarthritis with calcium pyrophosphate deposition may experience more swelling and inflammation than a patient who has osteoarthritis without crystals.
Rheumatoid arthritis
Specialists estimate patients with rheumatoid arthritis are 2 times as possible to get pseudogout.
Underlying conditions
Several metabolic and endocrine disorders can predispose a person to pseudogout (CPPD), including:
Hemochromatosis is an inherited disease that induces the body to reserve excess iron in the organs and tissues around the joints or junctions.
Hyperparathyroidism can induce abnormal quantities of calcium in the blood, and possibly further thyroid diseases that involve the body’s metabolism.
Hypophosphatasia is a metabolic disease that involves bones and teeth.
Hypomagnesemia is a disease in which there are abnormally low magnesium levels in the blood.
Professionals suggest that persons with pseudogout be screened for underlying diseases if they are more youthful than 60 and have no genetic risk of calcium pyrophosphate deposition – CPPD condition.
Signs and Symptoms of a Pseudogout Attack
The specific signs and symptoms of pseudogout are defined below. State that although pseudogout symptoms normally settle within several weeks, they should not be left untreated. Over time pseudogout can lead to permanent joint or junction injury.
Pain
The most prominent symptom of pseudogout is pain at the involved joint or junction. If more than one joint or junction is involved, the pain can be more extreme in one joint or junction and moderate or mild in further joints or junctions.
Swelling
Fluid can create up in the joint or junction, causing prominent swelling.
Changes to the skin
As the joint or junction evolves inflamed, the skin over the joint or junction may seem red or purple (erythema) and may be warm to the touch. The skin may also seem stretched due to swelling.
Stiffness
Considerable swelling and aches may make it hard to bend and flex the joint or junction. In extra to feeling stiff, the joints or junction’s range of movement may be decreased.
Rapid onset
Pseudogout can evolve suddenly and without notice, bringing 6 to 12 hours for ache and swelling to peak in severity. (In contrast, chronic calcium pyrophosphate – CPP crystal arthritis has a more gradual beginning, reaching osteoarthritis. )
Fever and other flu-like symptoms
Pseudogout may induce chills, fever, and/or further body-wide symptoms, like a general feeling of being sick. These inflammatory symptoms may be activated as part of the reaction of the immune system to the calcium pyrophosphate crystals.
Duration of weeks or months
Left untreated, an attack of pseudogout can last days, weeks, or even months.
Pseudogout Symptoms Differ from Gout Symptoms
While the immune system responses that lead to gout and pseudogout create similar symptoms, there are differences:
Unlike gout, which frequently strikes in the middle of the night, pseudogout may appear at any time of day.
While pseudogout ache can be severe, it is generally less severe than the ache caused by an acute gout attack.
Recurrent patients of pseudogout do not result in tophi. Tophi (sing. tophus) are tiny white or yellow chunks of uric acid crystals that can be visually via the skin. They happen in a patient who has sorrowed from chronic gout for several years.
An untreated attack of pseudogout can last several weeks or months. In contrast, an untreated attack of gout generally lasts a couple of weeks or less.
In extra, the symptoms of gout can have an evident trigger, like eating specific foods, consuming alcohol, or a shift in drugs. An attack of pseudogout is less probable to have a clear cause. Investigators are restarting to learn about the disorders underlying reasons and triggers.
How is pseudogout diagnosed?
Physical examination
A doctor or physician will study the patients involved joint or junction, reporting pain points, swelling, and range of movement.
If your doctor or physician believes you have pseudogout, they may recommend the following tests:
a study of joint or junction fluid by removing the fluid from the joint or junction (arthrocentesis) to look for calcium pyrophosphate crystals
X-rays of the joints or junctions to inspect for any injury to the joint or junction, calcification (calcium buildup) of the cartilage, and deposits of calcium in the joint or junction cavities
MRI or CT scans to examine for sites of calcium buildup
ultrasound also to examine for sites of calcium buildup
Looking at the crystals found in the joint or junction cavities assists your doctor or physician assemble a diagnosis.
This disease shares symptoms with a other disease, so it may occasionally be misdiagnosed as:
- osteoarthritis (OA), a degenerative joint or junction disorder caused by loss of cartilage
- rheumatoid arthritis (RA), is a long-term inflammatory disease that may involve several organs and tissues
- gout, which generates painful inflammation of the toes and feet generally but can involve further joints or junctions
What medical conditions may be associated with pseudogout?
Pseudogout can occasionally be associated with other conditions, like:
the thyroid diseases hypothyroidism and hyperparathyroidism
hemophilia, a hereditary bleeding condition that controls the blood from clotting generally
ochronosis, a disease that generates a dark stain to deposit in the cartilage and further connective tissues
amyloidosis, a buildup of an irregular protein in the tissues
hemochromatosis, an abnormally increased level of iron in the blood
Treatment of Pseudogout
There’s no cure for pseudogout, but a mixture of therapies can assist ease pain and enhance the joint’s or junction’s function.
Medications
If over-the-counter ache relievers aren’t sufficient, your health care provider or doctor may recommend:
Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription-strength NSAIDs contain naproxen (Naprosyn) and indomethacin (Indocin). NSAIDs can induce stomach bleeding and reduce kidney function, particularly in older grown-ups.
Colchicine (Colcrys, Mitigare). Low-dose drugs of this gout medicine are also useful for pseudogout. If you have regular attacks of pseudogout, you may be recommended to bring colchicine every day as a preventive action.
Corticosteroids. If you can’t bring NSAIDs or colchicine, your healthcare provider or doctor may recommend bringing corticosteroid drugs, like prednisone, to decrease inflammation and end the episode. Long-term use of corticosteroids can weaken bones and induce cataracts, diabetes, and weight gain.
Joint drainage
Withdrawing some of the joint or junction fluid can ease aches and stress in an involved joint or junction. A syringe is used to withdraw the liquid. The method also assists to withdraw some of the crystals from the junction joint. The joint or junction is then injected with a numbing medicine and a corticosteroid to reduce inflammation.
Aspiration
A doctor or physician can aspirate a joint or junction by inserting a syringe into the involved joint or junction and removing some of the fluid that has been collected. Aspiration reduces stress, making the person more relaxed.
Physiotherapy treatment in Pseudogout
To relieve sudden, severe pseudogout ache, a health care provider or doctor may suggest:
Ice
A cool compress used on the involved joint or junction can assist to ease discomfort and reduce swelling.
Rest
It is generally painful to use the involved joint or junction. Resting it for a day or two can assist relieve pain, inflammation, swelling, and additional symptoms.
Elevation
If possible, elevating the involved limb can assist to decrease swelling. If the knee is involved, sitting down with the foot relaxing on a footstool or lying down with the foot supported up on a cushion may provide symptom ease.
Edema (swelling from extra fluid) control
It can be useful to use a light reduction wrap to decrease swelling. When swelling is extreme, the excess fluid makes it hard to move the joint or junction. It is better to control the swelling before it happens; yet, in most patients, the swelling has already happened by the time the person seeks medical supervision. If this is the issue, it’s necessary to decrease swelling fast to enhance function. Ice and elevation can enhance the swelling. And, as soon as the ache permits, movement enhances swelling. Treatment is very useful to get the joints or junctions moving again.
Splints
Splints can enhance pain by restricting painful joint or junction and tendon movement. They should just be utilized for a short time. Longer use can result in immobility.
Electrotherapy modalities
Symptomatic pain-relieving Electrotherapy modalities like TENS, Interferential therapy(IFT), Short wave Diathermy(SWD), and Ultrasound therapy are used to reduce inflammation, ache, and swelling of the joints or junctions.
Exercise
Exercise can assist strengthen the muscles near your joints or junctions, assist keep full motion and use of your joints or junctions and support your body physically fit.
Range of movement activities is especially useful during times when the CPPD crystal deposition condition is active. These are gentle activities done without any weights and designed to maintain the mobility of the joint or junction. The sore joint or junction should be slightly moved via its full available range of movement per day, spending special awareness to the end of the movement where mobility frequently is first lost. Using heat or cold applications before or after exercising can improve your convenience and the significance of these activities. Accomplish a range of movement activities daily to keep or restore movement after checking with your doctor or therapist.
During times when the CPPD crystal deposition condition is not active, strengthening activities can be done to provide maximum function and strength to your joints or junctions. These activities should be taught by a physical or occupational therapist or physician, mainly one who is aware of the CPPD crystal deposition condition.
Walking, bicycling and aquatic activities are frequently suggested for a patient with CPPD crystal deposition condition.
During the aquatic activity, the buoyancy of the water generally saves the joints or junctions from rapid or stressful motion. Your doctor or physical therapist can assist you to plan an activity schedule and can define precise kinds of activity to do during flares and remissions of the disease.
During a sudden episode of inflammation due to CPPD crystal deposition condition, you may require to rest your sore joint(s) or junctions. Occasionally splints are suggested for resting and guarding the joint(s) or junctions. Splints, canes, and additional instruments for protecting joints or junctions can be provided by physical or occupational therapists.
Surgery
If your joints or junctions are wearing out, your doctor or physician may suggest surgery to fix or replace them.
Lifestyle and home remedies
Home therapies may be helpful during pseudogout flare-ups. Examples contain:
NSAIDs. Over-the-counter NSAIDs, like ibuprofen (Motrin IB, Advil, others) and naproxen sodium (Aleve), frequently are useful.
Rest the joint. Try not to use the involved joint or junction for a couple of days.
Ice. Cold packs can assist to decrease the inflammation associated with flare-ups.
Diet for Pseudogout
Fruit: Good choices contain strawberries, cherries, raspberries, and citrus fruits.
Fish: The patient can try consuming herring, salmon, tuna, scallops, sardines, and anchovies.
Nuts: The AF specifically suggests pine nuts, walnuts, almonds, and pistachios.
Beans: Kidney beans and pinto beans are especially wealthy in antioxidants.
Olive oil: The patient should aim for 23 tablespoons every day.
Whole grains: These contain brown rice, oatmeal, and quinoa.
Nightshade vegetables: Instances contain potatoes, eggplant, tomatoes, and red bell peppers. Some patients think that these foods activate arthritis flares, so it is best to monitor symptoms when eating them.
The patient should avoid processed meals and those enriched in saturated fats.
What complications are associated with pseudogout?
In some circumstances, the crystal deposits in the synovial fluid can lead to permanent joint or junction injury. Joints or junctions that have been involved by pseudogout can ultimately create cysts or bone spurs, which are growths that adhere out on the bones. Pseudogout may even result in the defeat of cartilage.
Knee flexion deformity is also familiar where you can see your knee slightly flexing about 10 to 20 degrees and if you are trying to be fully straight is hard or not feasible. It is also known as FFD (Fixed flexion deformity)
What triggers pseudogout?
An episode of pseudogout is activated by CPP crystal formation. Several diseases can activate crystal formation, including:
- Lack of fluid (dehydration).
- An episode of any extreme condition.
- Overactivity of the parathyroid glands (hyperparathyroidism).
- Long-term use of steroid drugs.
- Underactive thyroid gland (hypothyroidism).
- Any cause of arthritis.
- An illness that generates too much iron in the body (hemochromatosis).
- An inherited illness generates a build-up of copper in the body (Wilson’s disease).
- An illness induced by a risen level of growth hormone in the body (acromegaly).
- Kidney dialysis.
- Surgery or injury.
- Low magnesium level in the blood (hypomagnesemia).
How to Prevent Pseudogout?
Therapy of a disease that raises the risk of pseudogout (like hemochromatosis) may control the development of the condition or repeated episodes. Yet, when there is no known reason or trigger, there is no way to control the development of pseudogout. For a patient with frequent episodes, bringing a nonsteroidal anti-inflammatory drug (NSAID) or colchicine every day may control future episodes.
Prognosis
With therapy, the perspective for pseudogout is generally good. Joint or junction aches and swelling generally go away promptly. It’s familiar for episodes to return, but generally, they can be managed with repeated therapy.
FAQ
What’s the difference between gout and pseudogout?
Gout and pseudogout, while both joint or junction issues are caused by crystals, are caused by various kinds of crystals. Gout is induced by sodium urate crystals and pseudogout is induced by calcium pyrophosphate crystals
Is pseudogout a form of rheumatoid arthritis?
Pseudogout evolves when deposits of calcium pyrophosphate crystals accumulate in a joint or junction. Originally, crystals deposit in the cartilage and can induce harm. They also can generate a response with inflammation that leads to joint or junction aches and swelling. This can generate more chronic arthritis that mimics osteoarthritis or rheumatoid arthritis – RA.
What is the most commonly affected joint for pseudogout?
Pseudogout (or “false gout”) is a state of arthritis that results from deposits of calcium pyrophosphate crystals (its medical word is calcium pyrophosphate dihydrate crystal deposition disease or CPPD). It generally involves the knees joints and wrists joints.
Is pseudogout caused by uric acid?
Pseudogout and gout are both kinds of arthritis, and they’re both induced by the collection of crystals in the joints or junctions. While pseudogout is induced by calcium pyrophosphate crystals, gout is induced by urate (uric acid) crystals.
What foods should be avoided with pseudogout?
In the circumstance of gout and pseudogout which are involved by the metabolic factor of the body, it is best to avoid high-purine food such as red meat and shellfish. Consuming beer and soda can also promote the level of uric acid which may worsen the ache and discomfort in joints or junctions





6 Comments