Botulinum toxin (Botox Injections)
Introduction
The bacterium Clostridium botulinum makes a powerful neurotoxic protein known as botulinum toxin or Botox. It is considered one of the most powerful naturally occurring toxins. Botulinum toxin is a type of bacterial exotoxin that works by blocking the release of a chemical called acetylcholine, which is essential for nerve cell communication. Botox is primarily known for its medical and cosmetic uses.
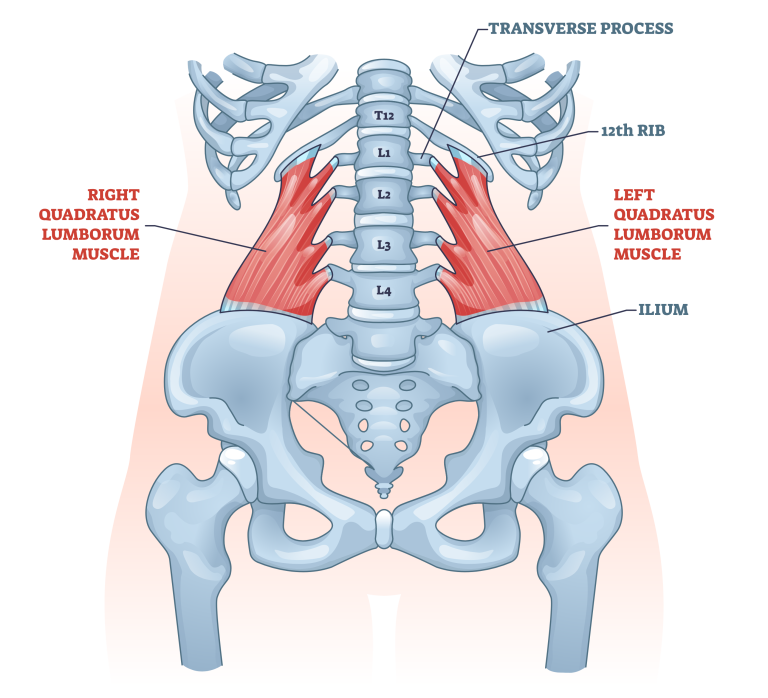
In medicine, it is used to treat various conditions related to muscle spasticity, such as cervical dystonia (a condition characterized by abnormal neck muscle contractions), muscle stiffness in upper and lower limbs, and excessive sweating (hyperhidrosis). It can also be used to manage chronic migraines and certain types of bladder and bowel disorders.
On the cosmetic front, Botox injections are popularly used to temporarily reduce the appearance of facial wrinkles and fine lines by relaxing the underlying muscles. It is commonly used to treat frown lines between the eyebrows, crow’s feet around the eyes, and forehead lines. Botox injections work by inhibiting muscle contractions in the treated areas, leading to a smoother and more youthful appearance. Although botulinum toxin, the generic structure of Botox, is considered to be its base form, this does not ensure that it will be an efficient cosmetic therapy.
Although botulinum toxin is highly toxic in its pure form, when used in small, controlled doses under medical supervision, it has been proven to be safe and effective for various therapeutic and cosmetic purposes. The effects of Botox injections are transient and generally last for a few months, after which the treatment can be repeated if desired. It is important to note that Botox should only be administered by qualified medical professionals who are trained in its usage and familiar with its potential risks and side effects. Improper use or dosage can lead to adverse effects, such as muscle weakness, drooping eyelids, difficulty swallowing, and even respiratory problems.
Overall, botulinum toxin, specifically Botox, has revolutionized the fields of medicine and aesthetics, providing patients with non-surgical treatment options for various conditions and helping them achieve smoother, more youthful-looking skin.
- AHFS/Drug: Monograph
- ATC code: M03AX01 (WHO)
- License data: US DailyMed: Botulinum toxin
- Pregnancy category: : AU: B3;
- Routes of administration: Intramuscular, subcutaneous, intradermal
Toxic proteins made by the CLOSTRIDIUM BOTULINUM species. The poisons are orchestrated as a solitary peptide chain which is handled into a full-grown protein comprising of a weighty chain and light chain joined employing disulfide security. Upon endocytosis into presynaptic nerve endings, the botulinum toxin light chain, a zinc-dependent protease, is released from the heavy chain. The light chain of botulinum toxin breaks down specific SNARE proteins inside the cell, which are necessary for SYNAPTIC VESICLES to secrete acetylcholine. Muscle paralysis is caused by this inhibition of acetylcholine release.
ATC Classification
- M — MUSCULO-SKELETAL SYSTEM
- M03 — MUSCLE RELAXANTS
- M03A — MUSCLE RELAXANTS, PERIPHERALLY ACTING AGENTS
- M03AX — Other muscle relaxants, incidentally acting specialists
- M03AX01 — botulinum toxin
What is Botulinum Toxin?
The bacterium Clostridium botulinum makes a neurotoxic protein which is known as botulinum toxin. It is considered one of the most potent naturally occurring toxins. The toxin works by blocking the release of acetylcholine, a neurotransmitter that plays a crucial role in the communication between nerve cells and muscle fibers. The production of botulinum toxin occurs when Clostridium botulinum bacteria grow in an anaerobic (oxygen-free) environment and produce the toxin as a byproduct. There are seven known types of botulinum toxin, labeled as type A through type G, each produced by different strains of the bacteria. However, the most commonly used types in medical and cosmetic applications are botulinum toxin type A and botulinum toxin type B.
Botulinum toxin type A (BoNT/A) is available in various commercial formulations, including Botox, Dysport, Xeomin, and Jeuveau. It is the most widely used type and has a long history of medical and cosmetic applications. Botulinum toxin type B (BoNT/B) is less commonly used but still has specific medical uses. When botulinum toxin is injected into a muscle, it blocks the release of acetylcholine, preventing the muscle from receiving signals to contract. This causes temporary paralysis or relaxation of the muscle, depending on the dosage and specific application. The effects typically last for a few months, after which the muscle gradually regains its normal function as new nerve terminals form and acetylcholine release resumes.
In the medical field, botulinum toxin is used for a range of conditions related to muscle spasticity, including cervical dystonia (involuntary neck muscle contractions), spasticity in upper and lower limbs, muscle stiffness, chronic migraines, certain types of bladder and bowel disorders, and more. It has been proven effective in reducing muscle tone and alleviating symptoms associated with these conditions. In the cosmetic realm, botulinum toxin injections are popularly used to reduce the appearance of facial wrinkles and fine lines. It is commonly used to treat frown lines between the eyebrows, crow’s feet around the eyes, forehead lines, and other facial wrinkles caused by repetitive muscle contractions. By temporarily relaxing the muscles accountable for these wrinkles, botulinum toxin injections can also result in a smoother and more youthful impression.
It’s important to note that botulinum toxin is a highly potent toxin, and its use should only be administered by qualified medical professionals who are trained in its usage. Improper administration or dosage can lead to adverse effects, such as muscle weakness, drooping eyelids, difficulty swallowing, and respiratory problems. However, when used correctly and under proper medical supervision, botulinum toxin has proven to be safe and effective for various therapeutic and cosmetic applications.
Types of botulinum toxin
There are seven known types of botulinum toxin, labeled as type A through type G. Each type is produced by different strains of the bacterium Clostridium botulinum and has slightly different properties. However, the two most commonly used types in medical and cosmetic applications are botulinum toxin type A and botulinum toxin type B.
- Botulinum Toxin Type A (BoNT/A): This is the most widely used type of botulinum toxin. It is produced by various strains of Clostridium botulinum and is available in different commercial formulations, such as Botox, Dysport, Xeomin, and Jeuveau. Botulinum toxin type A works by blocking the release of acetylcholine, thereby temporarily paralyzing the targeted muscles. It is commonly used for cosmetic purposes to reduce the appearance of wrinkles and fine lines, as well as for medical conditions like muscle spasticity and chronic migraines.
- Botulinum Toxin Type B (BoNT/B): This type of botulinum toxin is produced by specific strains of Clostridium botulinum. It functions in a similar method to type A by inhibiting acetylcholine release. BoNT/B is less commonly used than type A but still has medical applications. It is used for treating cervical dystonia, muscle spasticity, and certain movement disorders.
- Botulinum Toxin Type C (BoNT/C): BoNT/C is produced by Clostridium botulinum type C strains. It is a less prevalent type compared to types A and B. BoNT/C has been associated with botulism outbreaks in animals, but its use in medical or cosmetic applications is limited.
- Botulinum Toxin Type D (BoNT/D): BoNT/D is produced by Clostridium botulinum type D strains. It is similar to types A and B in terms of its mechanism of action. However, it is less well-studied, and its clinical applications are currently limited.
- Botulinum Toxin Type E (BoNT/E): BoNT/E is produced by Clostridium botulinum type E strains. It is relatively rare and less commonly associated with human botulism cases. Its medical and cosmetic applications are limited compared to types A and B.
- Botulinum Toxin Type F (BoNT/F): BoNT/F is produced by Clostridium botulinum type F strains. It shares similarities with other types in terms of its mechanism of action. However, like types C and D, it is less commonly used in clinical applications.
- Botulinum Toxin Type G (BoNT/G): BoNT/G is produced by Clostridium botulinum type G strains. It is considered one of the rarest types of botulinum toxin and has limited clinical significance.
It is important to note that each type of botulinum toxin may have different potencies, durations of action, and specific uses. Medical professionals carefully select the appropriate type and dosage based on the patient’s condition and the desired outcome.
What do your botulinum toxins use for?
Botulinum toxin, also known as Botox, has various medical and cosmetic uses. Botulinum toxin treatments should be administered by qualified healthcare professionals, typically licensed physicians or other medical professionals who have received specific training in its usage. Here are some of the detailed applications of botulinum toxin:
Medical Uses:
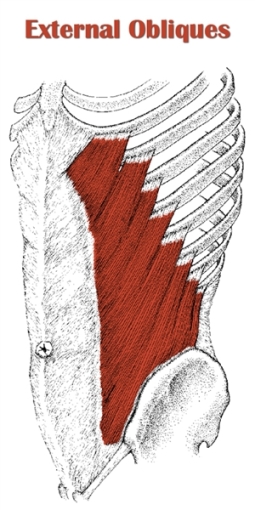
- Muscle Spasticity: Botulinum toxin is used to treat muscle spasticity caused by conditions such as cerebral palsy, multiple sclerosis, spinal cord injury, and stroke. It helps relax the muscles and reduce abnormal muscle contractions, improving mobility and reducing pain.
- Cervical Dystonia: Cervical dystonia, also known as spasmodic torticollis, is a condition characterized by involuntary contractions of the neck muscles, causing abnormal head and neck movements. Botulinum toxin injections can help alleviate muscle spasms and reduce the severity of abnormal head positioning.
- Blepharospasm: Blepharospasm is a condition characterized by involuntary contractions of the eyelid muscles, leading to uncontrollable blinking or eye closure. Botulinum toxin injections can help reduce these muscle spasms and improve eye comfort and vision.
- Chronic Migraines: Botulinum toxin has been approved for the treatment of chronic migraines. It is injected into specific head and neck muscles to reduce muscle tension and decrease the frequency and severity of migraine headaches.
- Hyperhidrosis: Botulinum toxin injections can be used to treat excessive sweating (hyperhidrosis) in areas such as the underarms, hands, and feet. The toxin blocks the nerve signals that stimulate sweat gland activity, reducing sweating.
- Overactive Bladder: Botulinum toxin can be used as a treatment option for overactive bladder. It is injected into the bladder muscle to relax it, reducing urinary urgency and frequency.
Cosmetic Uses:
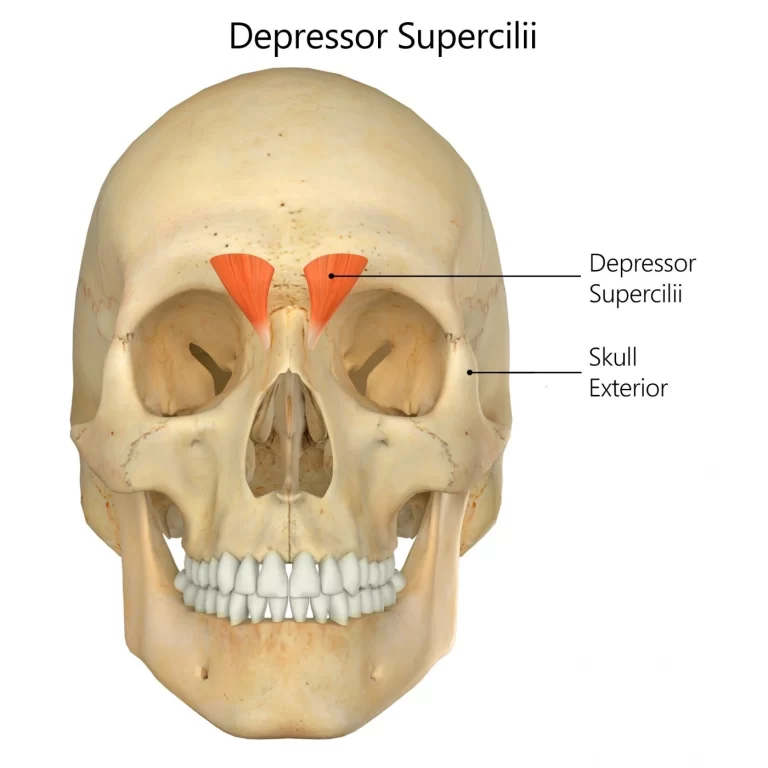
- Wrinkle Reduction: Botulinum toxin injections are widely used for cosmetic purposes to reduce the appearance of facial wrinkles and fine lines caused by muscle contractions. It is commonly used to treat frown lines between the eyebrows (glabellar lines), crow’s feet around the eyes, forehead lines, and other dynamic wrinkles.
- Brow Lift: Botulinum toxin can be used to lift the eyebrows and create a more youthful and open appearance. It is injected into specific muscles to relax them and elevate the brow position.
- Jawline Contouring: Botulinum toxin injections can be used to contour the jawline by relaxing the masseter muscles, which are responsible for chewing. This can help achieve a slimmer and more defined jawline.
- Excessive Salivation: Botulinum toxin injections can be used to treat conditions that result in excessive saliva production, such as sialorrhea. The toxin helps reduce saliva production by blocking the nerve signals that stimulate salivary gland activity.
It’s important to note that these are just a few examples of the medical and cosmetic uses of botulinum toxin. The specific application and dosage may vary depending on the individual’s condition and desired outcome. The administration of botulinum toxin should be performed by qualified healthcare professionals with expertise in its usage. Overall, the administration of botulinum toxin should be carried out by healthcare professionals who have the necessary training and expertise to ensure safe and effective treatment.
How to use Botulinum toxin?
The use of botulinum toxin, specifically for medical and cosmetic purposes, should be performed by qualified healthcare professionals who have received specific training in its administration. Here are the general steps involved in the process of using botulinum toxin:
- Consultation: Before undergoing botulinum toxin treatment, an individual typically has an initial consultation with a healthcare professional who specializes in the desired treatment area, such as a dermatologist, plastic surgeon, neurologist, or other relevant specialists. During the consultation, the healthcare professional will evaluate the individual’s specific needs, discuss their medical history, conduct a physical examination, and determine if botulinum toxin treatment is appropriate and safe for them.
- Treatment Planning: Based on the consultation, the healthcare professional will develop a treatment plan tailored to the individual’s specific concerns and goals. They will determine the optimal dosage, injection sites, and the specific type of botulinum toxin to be used (e.g., type A or type B). The treatment plan will outline the areas to be treated, the expected outcomes, and any potential risks or side effects.
- Preparation: The healthcare professional will prepare the botulinum toxin for injection. Botulinum toxin comes in a powder form and needs to be reconstituted with a sterile liquid, usually saline solution, before use. This is done to ensure the correct concentration and volume of the toxin for safe and effective administration.
- Injection Procedure: The healthcare professional will cleanse the treatment area and may apply a topical anesthetic or ice pack to numb the area and minimize discomfort during the injections. Using a very fine needle, they will carefully inject small amounts of botulinum toxin into the targeted muscles or specific sites, as determined by the treatment plan. Multiple injections may be needed to address the desired areas.
- Post-Treatment Care: After the injections, the healthcare professional may apply ice or a cooling agent to help reduce any potential swelling or discomfort. They may provide specific aftercare instructions, which may include avoiding strenuous activities, touching or massaging the treated area, and refraining from lying down for a certain period. It’s essential to follow these instructions for optimal results and to minimize any potential complications.
- Results and Follow-Up: The effects of botulinum toxin treatment are not immediate and typically take a few days to become noticeable. The individual may start to see the desired effects within a week or two after the treatment. The duration of the results varies depending on the specific application and individual factors but generally lasts for several months. Follow-up appointments may be scheduled to assess the outcomes, address any concerns, and determine if additional treatments are necessary.
It’s important to note that the above steps provide a general overview, and the actual procedure may vary depending on the specific purpose of treatment and the healthcare professional’s technique. Botulinum toxin should only be administered by qualified professionals who are experienced in its usage to ensure safety and optimal results.
Who Cannot take botulinum toxin?
While botulinum toxin injections are generally safe, certain individuals may not be suitable candidates for treatment. Here are some factors that may preclude someone from receiving botulinum toxin injections:
- Allergies or Sensitivities: Individuals with a known allergy or hypersensitivity to botulinum toxin or any of its components should not receive botulinum toxin injections. It’s important to inform the healthcare professional about any known allergies or sensitivities during the consultation.
- Infection at the Injection Site: If there is an active infection or skin condition at the proposed injection site, it is typically recommended to delay botulinum toxin treatment until the infection or condition has resolved. Injecting into an infected area can increase the risk of complications.
- Pregnancy and Breastfeeding: The safety of botulinum toxin injections during pregnancy and breastfeeding has not been established. As a precautionary measure, it is generally recommended to avoid these treatments during pregnancy or while breastfeeding.
- Neuromuscular Disorders: Individuals with certain neuromuscular disorders, such as Eaton-Lambert syndrome, myasthenia gravis, or amyotrophic lateral sclerosis (ALS), may be at an increased risk of adverse effects from botulinum toxin treatment. The use of botulinum toxin in these cases should be carefully evaluated by a healthcare professional with expertise in managing neuromuscular disorders.
- Blood Thinners: If an individual is taking blood-thinning medications, such as warfarin or aspirin, it may increase the risk of bruising or bleeding at the injection site. The healthcare professional should be informed about any medications or supplements being taken to assess the risks and potential adjustments to the treatment plan.
- Certain Medical Conditions: Some medical conditions, such as Lambert-Eaton myasthenic syndrome, peripheral neuropathy, or a history of severe allergic reactions, may require caution when considering botulinum toxin treatment. These conditions can impact the individual’s ability to tolerate the treatment or increase the risk of adverse effects.
It’s important to discuss your medical history, current medications, and any underlying health conditions with a qualified healthcare professional before considering botulinum toxin treatment. They will be able to assess your specific circumstances and determine if you are a suitable candidate for the procedure.
Mechanism of botulinum toxin
The mechanism of botulinum toxin involves its ability to interfere with the normal function of nerve cells, specifically at the neuromuscular junction. Here is a detailed explanation of the mechanism of botulinum toxin:
- Nerve Cell Signaling: Normally, nerve cells (neurons) release a chemical messenger called acetylcholine to transmit signals to muscle cells. Acetylcholine binds to receptors on muscle cells, leading to muscle contractions.
- Botulinum Toxin Binding: When botulinum toxin is injected into the body, it selectively binds to nerve endings in the vicinity of the injection site. The toxin is taken up by the nerve cells through endocytosis, a process in which the cell engulfs the toxin-containing vesicle.
- Disruption of Neurotransmitter Release: Once inside the nerve cell, the botulinum toxin targets a protein called synaptosomal-associated protein 25 (SNAP-25), which is essential for the release of acetylcholine-containing vesicles. The toxin cleaves SNAP-25, preventing its normal function.
- Inhibition of Acetylcholine Release: By cleaving SNAP-25, botulinum toxin interferes with the release of acetylcholine from nerve cells. As a result, the amount of acetylcholine available for transmission is significantly reduced.
- Muscle Paralysis: With decreased acetylcholine release, the signal transmission between nerve cells and muscle cells is disrupted. The muscle cells do not receive sufficient stimulation to contract, resulting in temporary muscle paralysis or relaxation in the targeted area.
- Regeneration of SNAP-25: Over time, the cleaved SNAP-25 molecules are regenerated within the nerve cells, restoring their normal function. This regeneration process typically takes several months.
The effects of botulinum toxin treatment are temporary and gradually wear off as the regenerated SNAP-25 allows for the resumption of acetylcholine release and normal neuromuscular activity. The duration of the effects varies depending on the individual, the specific botulinum toxin type used, and the treatment area. Typically, the effects last for several months before retreatment may be required. It is important to note that the mechanism described here is a simplified explanation of the overall process. The interaction between botulinum toxin and nerve cells involves a complex series of biochemical and molecular events that are the subject of ongoing research and study.
Pharmacodynamics of botulinum toxin
The pharmacodynamics of botulinum toxin refers to how the toxin interacts with the body’s cells and tissues to produce its desired effects. Here is a detailed explanation of the pharmacodynamics of botulinum toxin:
- Mechanism of Action: Botulinum toxin acts on the neuromuscular junction, the connection between nerve cells and muscle cells, to disrupt normal neurotransmitter release. It specifically targets the protein SNAP-25, which is involved in the fusion of acetylcholine-containing vesicles with the cell membrane of the nerve terminal.
- Selective Binding: Botulinum toxin has a high affinity for nerve endings, particularly those responsible for motor function. It selectively binds to the presynaptic membrane of these nerve cells, specifically the cholinergic neurons involved in muscle contraction.
- Internalization and Intracellular Targeting: After binding to the nerve endings, the botulinum toxin is internalized by endocytosis, a process in which the toxin-containing vesicle is engulfed by the nerve cell. Once inside the cell, the toxin undergoes a series of enzymatic processes to become activated.
- Cleavage of SNAP-25: Activated botulinum toxin targets SNAP-25, a protein involved in the formation of the SNARE complex, which is responsible for the release of acetylcholine. The toxin cleaves specific sites on SNAP-25, preventing its proper function and disrupting the docking and fusion of acetylcholine-containing vesicles with the cell membrane.
- Inhibition of Neurotransmitter Release: By cleaving SNAP-25, botulinum toxin blocks the release of acetylcholine from the nerve terminals. This results in a decreased transmission of signals from the nerve cells to the muscle cells, leading to muscle paralysis or relaxation in the affected area.
- Temporal Effects: The effects of botulinum toxin are not permanent. Over time, the cleaved SNAP-25 molecules are regenerated within the nerve cells, allowing for the restoration of normal neurotransmitter release and muscle function. The duration of the effects varies depending on the individual, the specific botulinum toxin type used, and the treatment area. Typically, the effects last for several months before retreatment may be required.
- Spreading and Local Effects: It’s important to note that while botulinum toxin is administered locally to the targeted muscle or tissue, there can be some diffusion or spreading of the toxin to adjacent areas. This spreading can lead to the desired effects in the surrounding muscles or unintended effects if not carefully controlled and administered by a qualified healthcare professional.
The pharmacodynamics of botulinum toxin are complex, involving a cascade of biochemical events that ultimately disrupt normal neuromuscular transmission. Understanding the pharmacodynamics is crucial for healthcare professionals to optimize the therapeutic or cosmetic effects of botulinum toxin and minimize any potential risks or adverse reactions.
Metabolism of botulinum toxin
The metabolism of botulinum toxin involves its breakdown and elimination from the body after administration. Here is a detailed explanation of the metabolism of botulinum toxin:
- Distribution: After administration, botulinum toxin is distributed from the injection site to its target tissues, primarily the neuromuscular junctions where it exerts its effects.
- Binding and Internalization: Botulinum toxin binds to the presynaptic membrane of nerve cells at the injection site and is then internalized by endocytosis, a process in which the toxin-containing vesicle is engulfed by the nerve cell.
- Activation and Cleavage: Once inside the nerve cell, botulinum toxin undergoes a series of enzymatic processes to become activated. The toxin’s heavy chain mediates its translocation into the cytoplasm, where the light chain is released. The light chain of botulinum toxin is responsible for its enzymatic activity and cleaves specific sites on the protein SNAP-25.
- Degradation and Elimination: The cleaved botulinum toxin molecules, including the light chain, are subject to degradation within the nerve cell. The precise details of the intracellular degradation pathways are still being investigated, but it is believed that proteases within the cell break down the toxin into smaller fragments.
- Clearance: The fragments of botulinum toxin, along with any unbound or uninternalized toxin, are eventually cleared from the nerve cells. The exact mechanisms of clearance are not fully understood, but it is thought to involve lysosomal degradation and cellular exocytosis.
- Elimination from the Body: The cleared botulinum toxin fragments, along with other waste products, are ultimately eliminated from the body through normal metabolic processes. They may be excreted in urine or feces.
The metabolism of botulinum toxin is a complex process that involves cellular internalization, enzymatic activity, degradation, and elimination. The exact timeline and rate of metabolism may vary depending on factors such as the specific botulinum toxin type, dose, individual metabolism, and treatment area. It’s worth noting that while the majority of the botulinum toxin is eliminated from the body, trace amounts may persist in the injected muscle tissue for an extended period. However, these residual amounts are typically not associated with any significant clinical effects. Understanding the metabolism of botulinum toxin helps healthcare professionals assess the duration of its effects and determine appropriate dosing intervals for subsequent treatments.
Absorption of botulinum toxin
The absorption of botulinum toxin refers to its uptake into the bloodstream and subsequent distribution to its target tissues after administration. Here is a detailed explanation of the absorption process:
- Injection Site: Botulinum toxin is typically administered via injection directly into the target muscle or tissue. The toxin is introduced into the body at the specific site where it is intended to exert its effects.
- Localized Effects: After injection, botulinum toxin remains primarily localized at the injection site, exerting its effects on the nearby neuromuscular junctions. It acts locally to block the release of acetylcholine and induce muscle paralysis or relaxation in the targeted area.
- Diffusion: Over time, botulinum toxin may undergo diffusion or spread from the injection site to adjacent tissues. This diffusion can lead to the desired effects in the surrounding muscles or unintended effects if not carefully controlled and administered by a qualified healthcare professional.
- Uptake into Circulation: A small portion of the botulinum toxin may be absorbed into the bloodstream from the injection site. The rate and extent of absorption depend on factors such as the injection technique, dose, and the specific botulinum toxin type.
- Systemic Distribution: Once in the bloodstream, the absorbed botulinum toxin is distributed throughout the body via the circulatory system. It can reach distant tissues and organs, although the concentration is typically much lower compared to the localized effects at the injection site.
- Metabolism and Elimination: Botulinum toxin that enters the bloodstream may undergo metabolism and elimination processes similar to those described in the “Metabolism of Botulinum Toxin” response. The toxin is broken down into smaller fragments and eventually cleared from the body through urine or feces.
It’s important to note that the majority of the therapeutic or cosmetic effects of botulinum toxin are achieved through its local action at the injection site, where it blocks the release of acetylcholine and temporarily paralyzes or relaxes the targeted muscles. Systemic absorption and distribution of botulinum toxin are generally limited, and the clinical significance of any systemic effects is generally minimal when administered by a qualified healthcare professional following appropriate guidelines. It’s worth mentioning that the absorption of botulinum toxin can be influenced by factors such as the injection technique, muscle activity, blood flow, and the specific formulation of the toxin. Healthcare professionals consider these factors to optimize the localization of effects and minimize any potential systemic effects.
The half-life of botulinum toxin
The half-life of botulinum toxin refers to the time it takes for half of the administered toxin to be eliminated from the body. The half-life can vary depending on the specific botulinum toxin type, the dose administered, and individual factors. Here are some details regarding the half-life of botulinum toxin:
- Botulinum Toxin Type A: The most commonly used botulinum toxin type A formulations, such as Botox, Dysport, Xeomin, and Jeuveau, have an estimated half-life ranging from 3 to 4 months. This means that after the initial injection, approximately half of the toxin will be eliminated from the body within that time frame.
- Botulinum Toxin Type B: Botulinum toxin type B, available as Myobloc, has a longer half-life compared to type A. It is estimated to have a half-life of around 16 to 23 weeks.
It’s important to note that the half-life of botulinum toxin represents the average time it takes for the toxin to be eliminated from the body, but individual variations may occur. Factors such as the metabolism rate, dose, injection technique, and treatment area can influence the duration of action and the rate at which the toxin is cleared. After the initial injection, the effects of botulinum toxin gradually diminish as the toxin is metabolized and eliminated. Repeat injections are typically required to maintain the desired therapeutic or cosmetic effects.
It’s worth mentioning that the half-life of botulinum toxin should not be confused with the duration of its clinical effects. The duration of effects can be longer than the half-life, as it also depends on factors such as the specific botulinum toxin type, dose, injection technique, and individual response. The duration of effects can vary between individuals, but it generally ranges from several months to up to six months. Consulting with a qualified healthcare professional who has expertise in administering botulinum toxin is essential to determine the appropriate treatment schedule based on individual factors and goals.
Protein binding of botulinum toxin
Botulinum toxin, specifically botulinum toxin type A, does not extensively bind to plasma proteins in the bloodstream. Instead, it remains largely unbound and free to exert its effects. The unbound fraction of botulinum toxin is responsible for its biological activity and ability to interact with target cells. The lack of significant protein binding contributes to the high potency and efficacy of botulinum toxin. It allows the toxin to readily diffuse from the injection site and interact with its target tissues, primarily the neuromuscular junctions.
However, it’s worth noting that there may be some minimal non-specific binding of botulinum toxin to plasma proteins, but it is not considered clinically significant. The primary mode of action of botulinum toxin involves its interaction with nerve cells and inhibition of neurotransmitter release, rather than extensive binding to plasma proteins. The low protein binding characteristic of botulinum toxin contributes to its specificity and localized effects, as it remains primarily concentrated at the injection site and the adjacent neuromuscular junctions.
Route of elimination of botulinum toxin
Botulinum toxin is primarily eliminated from the body through a combination of metabolic and excretory processes. Here are the main routes of elimination for botulinum toxin:
- Renal Excretion: A portion of the botulinum toxin and its metabolites may undergo renal excretion, which means they are eliminated from the body through urine. This route of elimination is relatively minor compared to other routes but can contribute to the overall elimination process.
- Hepatic Metabolism: Botulinum toxin and its fragments can undergo metabolic breakdown in the liver. The liver enzymes help to metabolize the toxin into smaller components that are then eliminated from the body through other routes.
- Fecal Excretion: The majority of the botulinum toxin and its metabolites are believed to be excreted through the feces. Biliary excretion, a process in which the toxin and its metabolites are transported into the bile by the liver, followed by fecal elimination, is the primary route for botulinum toxin elimination.
- Tissue Clearance: Following injection, botulinum toxin is localized in the target tissues, where it exerts its effects. Over time, as the toxin is metabolized and its effects diminish, the remaining fragments are cleared from the tissue by various cellular processes and eliminated through the aforementioned routes.
It’s important to note that the exact proportions of elimination through each route may vary depending on factors such as the specific botulinum toxin type, the dose administered, individual metabolism, and treatment area. The overall elimination process involves a combination of renal excretion, hepatic metabolism, fecal excretion, and tissue clearance. Understanding the routes of elimination of botulinum toxin helps healthcare professionals assess the duration of its effects and the potential for interactions with other medications that are metabolized or excreted through similar pathways.
The volume of distribution of botulinum toxin
The volume of distribution (Vd) of botulinum toxin refers to the theoretical volume that would be required to account for the total amount of the toxin in the body if it were uniformly distributed at the same concentration as in the plasma. However, determining the exact volume of distribution for botulinum toxin is challenging due to its complex pharmacokinetics and localization at the site of injection and target tissues. Additionally, the volume of distribution can vary depending on factors such as the specific botulinum toxin type, formulation, and dose administered.
Botulinum toxin is primarily localized at the injection site and the adjacent neuromuscular junctions where it exerts its effects. It does not have an extensive systemic distribution like many drugs. Therefore, the volume of distribution for botulinum toxin is generally limited and predominantly reflects the distribution within the localized tissues. The actual volume of distribution for botulinum toxin is difficult to quantify precisely. However, studies have shown that botulinum toxin, after injection into the muscle, remains primarily concentrated in the injected muscle and surrounding tissues. The concentration decreases with increasing distance from the injection site, indicating limited distribution beyond the immediate area.
In summary, the volume of distribution for botulinum toxin is relatively low and largely confined to the localized tissues at and near the injection site. The toxin’s distribution is primarily influenced by its mode of action and the specific area being treated, rather than systemic distribution throughout the body.
Pathways of this toxin
Botulinum toxin primarily acts by blocking the release of acetylcholine, a neurotransmitter responsible for muscle contraction, at the neuromuscular junction. The toxin’s pathway involves several steps, including binding, internalization, enzymatic activity, and inhibition of neurotransmitter release. Here is a detailed explanation of the pathways of botulinum toxin:
- Binding to Nerve Endings: Botulinum toxin initially binds to specific receptors on the presynaptic membrane of nerve endings at the site of injection. These receptors are typically proteins involved in the docking and release of neurotransmitters, particularly acetylcholine.
- Internalization: After binding, botulinum toxin is internalized by the nerve cell through endocytosis. The toxin-receptor complex is engulfed by the cell, forming an endosome, a vesicle within the cytoplasm of the neuron.
- Translocation into the Cytoplasm: Within the endosome, the botulinum toxin undergoes a process called translocation. The toxin’s heavy chain mediates its transport across the endosomal membrane into the cytoplasm of the nerve cell.
- Enzymatic Activity: Once in the cytoplasm, the botulinum toxin’s light chain is released. This light chain possesses enzymatic activity and acts as a protease. It specifically cleaves specific proteins involved in the release of acetylcholine, primarily a protein called SNAP-25 (synaptosomal-associated protein 25).
- Inhibition of Neurotransmitter Release: By cleaving SNAP-25, botulinum toxin prevents the fusion of acetylcholine-containing vesicles with the neuronal membrane, inhibiting the release of acetylcholine into the synaptic cleft. As a result, the communication between nerve cells and muscles is disrupted, leading to muscle paralysis or relaxation.
- Regeneration of Nerve Endings: Over time, the effects of botulinum toxin are temporary, as the nerve endings regenerate new SNAP-25 and other necessary proteins. This regeneration process allows for the restoration of normal neurotransmitter release and muscle function.
The pathways of botulinum toxin involve specific interactions with nerve cells, internalization, enzymatic activity, and inhibition of acetylcholine release. Understanding these pathways is crucial for the therapeutic or cosmetic use of botulinum toxin, as it allows for targeted intervention in neuromuscular function to achieve desired outcomes.
Toxicity of Botulinum toxin
Botulinum toxin, when used therapeutically in approved doses and under medical supervision, is generally safe. However, it’s important to note that botulinum toxin is one of the most potent toxins known, and improper use or overdose can lead to toxicity. Here are some details regarding the toxicity of botulinum toxin:
- Mechanism of Toxicity: Botulinum toxin causes toxicity by blocking the release of acetylcholine, a neurotransmitter that signals muscle contraction. This action leads to muscle paralysis and can affect various muscle groups, including those involved in respiration.
- Localized Effects: The primary therapeutic use of botulinum toxin is in localized muscle paralysis for specific medical conditions or cosmetic purposes. When used correctly by a trained healthcare professional, the effects are localized to the injection site and adjacent tissues, minimizing the risk of systemic toxicity.
- Systemic Effects: If botulinum toxin spreads beyond the intended area of injection or is administered in excessive doses, it can lead to systemic effects. These effects can include muscle weakness, difficulty swallowing or speaking, respiratory compromise, and in severe cases, respiratory failure.
- Rare Adverse Events: While rare, severe adverse events have been reported with botulinum toxin use. These include allergic reactions, muscle atrophy, eyelid or brow drooping, and ptosis (drooping of the upper eyelid).
- Duration of Effects: Botulinum toxin’s effects are not permanent, as the toxin is eventually metabolized and eliminated from the body. However, during its presence, the effects can last for several months, and if toxicity occurs, it may persist until the toxin is cleared.
- Patient Factors: Individual factors such as age, underlying medical conditions, sensitivity to the toxin, and the presence of neuromuscular disorders can influence the susceptibility to botulinum toxin toxicity.
It’s crucial to emphasize that botulinum toxin should only be administered by qualified healthcare professionals who have the necessary training and experience in its use. They follow strict guidelines for dosing and injection techniques to minimize the risk of toxicity. In cases of suspected botulinum toxin toxicity, immediate medical attention should be sought. Prompt intervention can help manage the symptoms, provide supportive care, and monitor respiratory function if necessary. Overall, when used appropriately and in approved doses, botulinum toxin is generally safe. However, it should be respected as a potent neurotoxin, and its use should be guided by medical professionals with expertise in its administration.
The function of botulinum toxin
The primary function of botulinum toxin is to inhibit the release of acetylcholine, a neurotransmitter responsible for muscle contraction. By blocking the release of acetylcholine, botulinum toxin causes temporary muscle paralysis or relaxation, leading to various therapeutic and cosmetic effects. Here are some of the main functions of botulinum toxin:
Therapeutic Uses:
- Muscle Spasticity: Botulinum toxin is used to treat muscle spasticity in conditions such as cerebral palsy, stroke, multiple sclerosis, and spinal cord injury. It helps reduce muscle stiffness and involuntary contractions, improving mobility and function.
- Chronic Migraine: Botulinum toxin injections are approved for the preventive treatment of chronic migraines, reducing the frequency and severity of headache episodes.
- Blepharospasm: Botulinum toxin is used to treat involuntary eyelid spasms (blepharospasm) and uncontrolled blinking (hemifacial spasm).
- Hyperhidrosis: It is also employed to manage excessive sweating (hyperhidrosis) by inhibiting sweat gland activity.
Cosmetic Uses:
- Facial Wrinkles: Botulinum toxin is widely used for cosmetic purposes to reduce the appearance of facial wrinkles and lines, such as crow’s feet, frown lines, and forehead wrinkles. It temporarily relaxes the underlying muscles responsible for these wrinkles, resulting in a smoother and more youthful appearance.
- Facial Contouring: In some cases, botulinum toxin can be used for non-surgical facial contouring, such as slimming the jawline or lifting the eyebrows.
Other Uses:
- Overactive Bladder: Botulinum toxin injections can be employed to treat an overactive bladder, helping to reduce urinary frequency and urgency.
- Strabismus: It is used to treat crossed eyes (strabismus) by relaxing specific eye muscles and aligning the eyes.
It’s important to note that botulinum toxin’s effects are temporary, and repeat treatments are typically required to maintain the desired therapeutic or cosmetic effects. The precise function of botulinum toxin depends on the specific treatment area, dosage, and expertise of the administering healthcare professional.
How long should I use an over-the-counter Botulinum toxin?
However, it’s important to note that over-the-counter botulinum toxin products do not exist. Botulinum toxin is a prescription medication that should only be administered by qualified healthcare professionals. It is used for therapeutic and cosmetic purposes under proper medical supervision. If you are considering using any over-the-counter products for cosmetic purposes, it is recommended to consult with a healthcare professional or dermatologist. They can provide guidance and recommend appropriate treatments or skincare products based on your individual needs and goals. It’s crucial to prioritize your health and safety by seeking proper medical advice and avoiding self-administration of medications or treatments that require professional expertise.
How long does Botulinum toxin take to work?
The onset of action of botulinum toxin can vary depending on several factors, including the specific type and formulation used, the dosage administered, the treatment area, and individual variations. Here is a more detailed explanation of the timeline for the effects of botulinum toxin:
- Initial Effects: After the injection of botulinum toxin, it takes time for the toxin to bind to the nerve endings, be internalized by the cells, and inhibit the release of acetylcholine, the neurotransmitter responsible for muscle contraction. Initially, there may be minimal noticeable effects in the first 24 to 48 hours after the injection.
- Days 3 to 5: Typically, within 3 to 5 days after the injection, patients begin to observe the initial effects of botulinum toxin treatment. The muscles targeted by the toxin start to relax, leading to a reduction in muscle activity and the associated symptoms. For cosmetic uses, this may manifest as a softening of wrinkles and lines, while in therapeutic applications, it may result in improved muscle function or decreased muscle spasticity.
- Days 7 to 14: Over the next week or two following the injection, the effects of botulinum toxin become more noticeable and reach their peak. The targeted muscles continue to relax further, and the desired therapeutic or cosmetic outcome becomes more apparent. This is typically when the full effects of the treatment are observed.
- Duration of Effects: The effects of botulinum toxin are not permanent, as the toxin is gradually metabolized and its effects diminish over time. For most individuals, the therapeutic or cosmetic benefits of botulinum toxin can last for approximately 3 to 4 months. However, the exact duration can vary among individuals and may depend on factors such as the specific botulinum toxin type, the dose administered, and individual metabolism.
It’s important to note that the timeline provided is a general guideline and individual responses to botulinum toxin treatment can vary. The effects may also be influenced by factors such as the area being treated, the dosage used, and the expertise of the administering healthcare professional. Consulting with a qualified healthcare professional is essential to receive personalized information and guidance regarding the expected timeline for botulinum toxin treatment in your specific case.
How botulinum toxin is prescribed
Botulinum toxin is a prescription medication that should only be prescribed and administered by qualified healthcare professionals, such as physicians, dermatologists, or plastic surgeons. The prescription process typically involves the following steps:
- Evaluation and Diagnosis: The healthcare professional will first evaluate your medical history and conduct a physical examination to determine if botulinum toxin is an appropriate treatment option for your specific condition. They will consider factors such as the area to be treated, your overall health, any underlying medical conditions, and potential contraindications or interactions with other medications.
- Treatment Plan: Based on the evaluation, the healthcare professional will develop a treatment plan tailored to your needs. They will determine the appropriate dosage, injection sites, and frequency of treatment based on your condition and desired outcomes.
- Informed Consent: Before proceeding with the treatment, the healthcare professional will explain the potential benefits, risks, and side effects of botulinum toxin. You will be provided with information about the procedure, expected results, and any possible complications. Informed consent is essential to ensure you understand the treatment and can make an informed decision about proceeding with it.
- Administration: If you decide to proceed with botulinum toxin treatment, the healthcare professional will administer the injections. The injections are typically performed directly into the targeted muscles or specific areas, using a fine needle. The number of injections and the amount of toxin used will depend on the treatment plan and the specific area being treated.
- Follow-up and Monitoring: After the treatment, the healthcare professional may schedule follow-up appointments to monitor your progress, assess the results, and make any necessary adjustments to the treatment plan. They will evaluate the duration of the effects and determine the appropriate timing for future treatments if needed.
It’s important to note that self-administration of botulinum toxin is not recommended. It should only be administered by qualified healthcare professionals who have the necessary training and expertise in its use. Following the prescribed dosage and instructions is crucial to ensure safe and effective treatment outcomes.
How does my doctor choose that botulinum toxin that’s good for me?
Your doctor will choose the appropriate botulinum toxin-based on several factors, including your specific condition, treatment goals, medical history, and individual factors. Here are some considerations that may influence their decision:
- Approved Indications: Botulinum toxin products are approved for specific medical indications by regulatory authorities, such as the U.S. Food and Drug Administration (FDA). Your doctor will consider if a particular botulinum toxin has been approved for the specific condition you are seeking treatment for. Each approved indication may have specific guidelines and dosing recommendations.
- Efficacy and Clinical Evidence: Your doctor will review the clinical evidence supporting the use of different botulinum toxin products for your condition. They will consider studies, clinical trials, and published data that demonstrate the effectiveness and safety of each product for the intended use. This helps ensure that the chosen botulinum toxin has a track record of providing the desired therapeutic benefits.
- Experience and Expertise: Your doctor’s experience and familiarity with different botulinum toxin products may also play a role in their decision. They may have expertise in using a specific product or have observed favorable outcomes with a particular formulation. Their familiarity with the product’s characteristics, dosing, and administration techniques can contribute to better treatment results.
- Patient-specific Factors: Your doctor will consider your characteristics, such as your medical history, any known allergies or sensitivities, concurrent medications, and potential contraindications. They will take into account factors such as your age, overall health, and previous treatment responses to tailor the treatment plan and choose the botulinum toxin that best suits your needs.
- Patient Preferences: Your doctor may also consider your preferences and expectations regarding treatment. They will discuss the potential benefits, risks, and side effects of different botulinum toxin options with you and take your input into account when making the final decision.
It’s important to have open and honest communication with your doctor, sharing any relevant information about your health and treatment goals. This will help your doctor make an informed decision and select the botulinum toxin product that is most suitable for your specific circumstances.
What are the Botulinum toxin’s side effects?
Botulinum toxin is generally considered safe when administered by qualified healthcare professionals. However, as with any medication, it may cause unwanted effects. It is important to remember that different people may experience different side effects and how bad they are. Here are some of the potential side effects of botulinum toxin:
- Injection Site Reactions: Common side effects include temporary redness, swelling, bruising, or pain at the injection site. Most of the time, these reactions are mild and go away on their own within a few days.
- Muscle Weakness: Botulinum toxin’s primary effect is muscle relaxation, but in some cases, it can cause temporary weakness or drooping of nearby muscles. This can result in symptoms such as drooping eyelids, uneven smile, or difficulty with facial expressions. These effects are usually temporary and resolve as the effects of the toxin wear off.
- Flu-like Symptoms: Some individuals may experience flu-like symptoms, such as fatigue, headache, or mild fever, following botulinum toxin injections. These symptoms mostly relieve within a few days.
- Dry Mouth or Eyes: In rare cases, botulinum toxin injections can lead to temporary dryness of the mouth or eyes. This typically resolves on its own without any specific treatment.
- Allergic Reactions: Although rare, allergic reactions to botulinum toxin can occur. Signs of an allergic reaction may include itching, rash, hives, difficulty breathing, or swelling of the lips, tongue, throat, or face. Allergic reactions require immediate medical attention.
- Systemic Spread: Although extremely rare, there have been reported cases of botulinum toxin spreading to distant areas from the injection site, causing unwanted muscle weakness or other adverse effects. This risk is minimized when the injections are performed by experienced professionals who follow proper administration techniques.
It’s important to discuss any concerns or potential side effects with your healthcare professional before undergoing botulinum toxin treatment. They can provide you with detailed information based on your specific situation and address any questions or doubts you may have.
What should I know regarding the storage and disposal of this toxin?
Storage and disposal of botulinum toxin should be done following the guidelines provided by the manufacturer and local regulations. Here are some general considerations:
- Storage: Botulinum toxin should be stored in a controlled and secure environment, typically in a refrigerator between 2°C and 8°C (36°F and 46°F). Follow the specific storage instructions provided with the product, as different formulations may have varying requirements. Protect the medication from light and avoid freezing.
- Handling: When handling botulinum toxin, it’s important to follow proper aseptic techniques. Use sterile needles, syringes, and other equipment for preparation and administration. Avoid touching the vial stopper or needle to maintain sterility.
- Disposal: Proper disposal of botulinum toxin and associated equipment is crucial to prevent accidental exposure or misuse. Dispose of used needles, syringes, and vials in puncture-resistant containers, following local guidelines for sharps disposal. Check with your local healthcare waste disposal regulations for specific guidelines on disposing of unused or expired botulinum toxin.
- Unused Product: Unused botulinum toxin should be properly stored and not be used beyond the expiration date indicated on the packaging. Discard any expired or unused product according to local guidelines.
- Safety Considerations: It’s important to keep botulinum toxin out of the reach of children and unauthorized individuals. Only healthcare professionals with the necessary training and qualifications should handle and administer the medication.
Always consult the specific storage and disposal instructions provided by the manufacturer of the botulinum toxin product you are using. Additionally, follow the guidelines and regulations set forth by your local healthcare authorities and waste management systems to ensure safe and responsible handling and disposal of botulinum toxin and associated materials.
In what circumstances should I check with my doctor before taking the botulinum toxin
It is important to consult with your doctor before taking botulinum toxin in various circumstances. Here are some situations in which you should check with your doctor before undergoing botulinum toxin treatment:
- Pre-existing Medical Conditions: If you have any underlying medical conditions, such as neuromuscular disorders, myasthenia gravis, Lambert-Eaton syndrome, or any other muscle or nerve-related conditions, it is essential to inform your doctor. Certain medical conditions may increase the risk of complications or may require special considerations when using botulinum toxin.
- Medications and Allergies: Inform your doctor about any medications you are currently taking, including prescription drugs, over-the-counter medications, and herbal supplements. Some medications may interact with botulinum toxin, and adjustments may be necessary. Additionally, disclose any known allergies or sensitivities you have, especially if you have had an allergic reaction to botulinum toxin or any other medications in the past.
- Pregnancy and Breastfeeding: It is important to discuss with your doctor if you are pregnant, planning to become pregnant, or breastfeeding. The use of botulinum toxin during pregnancy and breastfeeding is generally not recommended, as its safety in these situations has not been well-established.
- Previous Botulinum Toxin Treatments: Inform your doctor about any previous botulinum toxin treatments you have undergone, including the type of toxin used and any adverse reactions or side effects experienced. This information will help your doctor determine the most appropriate course of action and potential adjustments to the treatment plan.
- Bleeding Disorders: If you have a bleeding disorder or are taking blood-thinning medications, it is important to inform your doctor. Botulinum toxin injections may increase the risk of bleeding or bruising at the injection site.
- Cosmetic Procedures: If you are considering using botulinum toxin for cosmetic purposes, such as reducing wrinkles or fine lines, it is advisable to consult with a qualified healthcare professional who specializes in cosmetic treatments. They will assess your suitability for the procedure, discuss your expectations, and provide you with the necessary information to make an informed decision.
Always consult your doctor or a healthcare professional who is experienced in botulinum toxin treatments to discuss your specific circumstances and address any concerns or questions you may have before proceeding with the treatment.
Before taking botulinum toxin
Before taking botulinum toxin, it is essential to consult with a qualified healthcare professional who can provide proper guidance and assess your suitability for the treatment. Here are some key considerations before undergoing botulinum toxin treatment:
- Consultation: Schedule a consultation with a healthcare professional who has experience and expertise in administering botulinum toxin. During the consultation, discuss your treatment goals, medical history, any underlying conditions, and previous treatments. This will help the healthcare professional determine if botulinum toxin is appropriate for you and develop a personalized treatment plan.
- Risks and Benefits: Understand the potential risks and benefits associated with botulinum toxin treatment. Your healthcare professional should explain the expected outcomes, possible side effects, and any rare complications that may arise. This information will help you make an informed decision about whether to proceed with the treatment.
- Medical History: Provide your complete medical history to the healthcare professional, including any previous surgeries, medical conditions, allergies, medications, or supplements you are taking. Certain medical conditions or medications may affect the suitability or dosage of botulinum toxin, so it’s crucial to disclose this information to your healthcare professional.
- Treatment Expectations: Discuss your treatment expectations with the healthcare professional. They can provide insights into what botulinum toxin can realistically achieve, the expected timeline for results, and how long the effects may last. Understanding these factors will help you have realistic expectations and avoid disappointment.
- Alternatives and Options: Your healthcare professional may discuss alternative treatment options or combinations of treatments that may be suitable for your specific concerns. They can provide information on the pros and cons of each option, allowing you to make an informed decision.
- Aftercare and Follow-up: Understand the post-treatment care instructions and any recommended follow-up appointments. Your healthcare professional should provide instructions on how to care for the treated area, any activities to avoid, and when to schedule a follow-up visit for assessment and potential touch-up treatments.
- Informed Consent: Before proceeding with the treatment, you will likely be asked to provide informed consent. This involves acknowledging that you have understood the potential risks, benefits, and alternatives of the treatment and voluntarily agreeing to undergo the procedure.
Remember, botulinum toxin should only be administered by qualified healthcare professionals who are experienced in its use. It is important to ask any questions you may have, express any concerns, and fully understand the treatment process before making a decision.
Can botulinum toxin cause allergic reactions?
While allergic reactions to botulinum toxin are rare, they can occur. Botulinum toxin is derived from the bacterium Clostridium botulinum, and like any medication, there is a small risk of allergic reactions in some individuals. Allergic reactions are typically immediate or delayed hypersensitivity responses to the medication.
Symptoms of an allergic reaction to botulinum toxin may include:
- Itching or hives
- Swelling of the face, lips, tongue, or throat
- Difficulty breathing or wheezing
- Rapid heartbeat or palpitations
- Dizziness or lightheadedness
- Nausea or vomiting
If you experience any signs of an allergic reaction after receiving botulinum toxin injections, it is important to seek immediate medical attention. Allergic reactions can be serious and potentially life-threatening, so it is crucial to notify your healthcare professional or go to the nearest emergency department. To minimize the risk of allergic reactions, it is important to disclose any known allergies or sensitivities to your healthcare professional before undergoing botulinum toxin treatment. They can evaluate your medical history and determine if botulinum toxin is appropriate for you or if an alternative treatment should be considered.
It’s worth noting that allergic reactions to botulinum toxin are relatively rare. The majority of individuals tolerate the treatment well and experience the desired therapeutic effects without any adverse reactions. However, it is important to be aware of the potential risk and seek prompt medical attention if you experience any concerning symptoms after receiving botulinum toxin injections.
What should I do if I forget a dose of the botulinum toxin?
If you forget a scheduled dose of botulinum toxin, it is important to contact your healthcare professional for guidance on the best course of action. Here are some general considerations:
- Contact Your Healthcare Professional: Notify your healthcare professional as soon as possible and inform them about the missed dose. They will be able to provide specific advice based on your circumstances and the purpose of the botulinum toxin treatment.
- Follow their Guidance: Your healthcare professional may recommend rescheduling the missed dose or adjusting the treatment schedule. They may also provide instructions on when and how to proceed with the next scheduled dose. It is crucial to follow their guidance to ensure the optimal effectiveness and safety of the treatment.
- Avoid Double Dosing: Do not attempt to compensate for the missed dose by taking an extra dose. Taking more botulinum toxin than prescribed can increase the risk of adverse effects without providing additional benefits.
- Maintain Communication: Keep your healthcare professional updated on any missed doses or deviations from the treatment plan. They can monitor your progress and make any necessary adjustments to ensure the desired therapeutic outcomes.
Remember, this information provides general guidance, and it is important to consult with your healthcare professional for personalized advice regarding missed doses of botulinum toxin. They will consider factors such as the specific indication for treatment, your response, and the overall treatment plan when guiding on managing missed doses.
Enhancing Healthcare Team Outcomes
Enhancing healthcare team outcomes when using botulinum toxin involves a collaborative approach among various healthcare professionals involved in the patient’s care. Here are some ways to optimize outcomes:
- Multidisciplinary Team: Form a multidisciplinary team consisting of healthcare professionals with expertise in botulinum toxin treatments, such as physicians, nurses, and specialists (e.g., neurologists, dermatologists, ophthalmologists). This team can collectively assess the patient’s needs, develop a treatment plan, and monitor progress.
- Comprehensive Assessment: Conduct a thorough evaluation of the patient, including medical history, current medications, allergies, and underlying conditions. This assessment helps identify potential risks, contraindications, and the most appropriate treatment approach.
- Clear Communication: Ensure effective communication within the healthcare team and with the patient. This includes sharing treatment goals, discussing potential risks and benefits, and addressing patient concerns. Clear communication facilitates coordination, enhances patient understanding, and promotes shared decision-making.
- Proper Training and Education: Healthcare professionals involved in botulinum toxin treatments should receive comprehensive training and continuing education to stay updated on the latest techniques, dosing guidelines, and safety considerations. Ongoing education helps maintain competency and ensures safe and effective administration.
- Standardized Protocols: Develop and implement standardized protocols for the administration, monitoring, and follow-up of botulinum toxin treatments. Consistent protocols promote consistency in care delivery, minimize errors, and improve patient outcomes.
- Adverse Event Management: Establish protocols for the management of potential adverse events related to botulinum toxin treatments. This includes recognizing and managing complications, providing appropriate medical interventions, and ensuring prompt referral to specialists if necessary.
- Documentation and Follow-up: Maintain accurate and comprehensive documentation of the treatment process, including dosages, injection sites, and patient responses. Regular follow-up appointments allow for evaluation of treatment effectiveness, adjustment of treatment plans if needed, and addressing any concerns or adverse events.
- Quality Assurance and Improvement: Implement quality assurance measures to regularly assess and monitor the outcomes and safety of botulinum toxin treatments. This can involve peer reviews, case discussions, and ongoing quality improvement initiatives to enhance patient care.
By promoting collaboration, effective communication, proper training, and standardized protocols, the healthcare team can optimize the outcomes of botulinum toxin treatments. This approach ensures patient safety, improves treatment effectiveness, and enhances overall patient satisfaction.
Expert Advice for botulinum toxin
When considering botulinum toxin treatments, it is important to seek expert advice from healthcare professionals who specialize in administering this treatment. Here are a few key points to believe:
- Consultation with a Qualified Healthcare Professional: Schedule a consultation with a qualified healthcare professional who has experience and expertise in botulinum toxin treatments. This may include dermatologists, plastic surgeons, ophthalmologists, or other specialists trained in cosmetic or therapeutic applications of botulinum toxin.
- Experience and Credentials: Inquire about the healthcare professional’s experience and credentials in administering botulinum toxin. Ask how many procedures they have performed and if they have received specialized training in the specific application you are seeking.
- Individualized Assessment: A reputable healthcare professional will conduct a thorough assessment of your specific concerns and goals. They will evaluate your facial anatomy, and medical history, and discuss your expectations to determine if botulinum toxin is suitable for you and develop a personalized treatment plan.
- Informed Consent: Before proceeding with the treatment, ensure that you fully understand the procedure, potential benefits, risks, and any alternative options. You should be provided with informed consent documents outlining the details of the treatment, including potential side effects and complications.
- Transparent Communication: The healthcare professional should communicate the expected outcomes, realistic expectations, and the longevity of results based on your situation. They should address any questions or concerns you have and provide you with all the necessary information to make an informed decision.
- Follow-up and Aftercare: A responsible healthcare professional will schedule follow-up appointments to assess the results of the treatment and address any concerns or touch-up needs. They should also provide aftercare instructions, including any restrictions or precautions to follow post-treatment.
- Safety and Hygiene Practices: Ensure that the healthcare professional follows strict safety and hygiene practices during the administration of botulinum toxin. This includes using sterile equipment, proper disinfection protocols, and adhering to all relevant medical guidelines and regulations.
- Continuing Education: Look for healthcare professionals who prioritize continuing education and stay updated on the latest advancements, techniques, and safety protocols related to botulinum toxin treatments. This demonstrates their commitment to delivering optimal care and staying informed about best practices.
Remember, choosing an experienced and reputable healthcare professional is crucial for achieving safe and satisfactory results with botulinum toxin treatments. Take the time to research and seek recommendations, and do not hesitate to ask questions or seek a second opinion if needed.
Precautions to take when using botulinum toxin
When using botulinum toxin, it is important to take certain precautions to ensure safety and optimize the effectiveness of the treatment. Here are some precautions to consider:
- Qualified Healthcare Professional: Botulinum toxin treatments should only be administered by qualified healthcare professionals who have received appropriate training and have experience in using the toxin. Ensure that you seek treatment from a reputable and licensed healthcare provider.
- Medical History: Disclose your complete medical history to the healthcare professional, including any underlying medical conditions, previous surgeries, allergies, and current medications or supplements. Certain medical conditions and medications may affect the suitability or dosage of botulinum toxin, so it is crucial to provide accurate information.
- Allergies: Inform your healthcare professional if you have a known allergy to any botulinum toxin products or their ingredients. Unfavorably susceptible responses to botulinum poison are intriguing however can happen. If you have experienced an allergic reaction in the past, it is important to discuss this with your healthcare professional.
- Pregnancy and Breastfeeding: Botulinum toxin treatments are generally not recommended during pregnancy or while breastfeeding, as the safety of the toxin in these situations has not been well-established. Consult your doctor before taking medicine if you are pregnant, planning to become pregnant, or breastfeeding.
- Medications and Supplements: Provide a list of all medications, including over-the-counter drugs and herbal supplements, that you are currently taking to your healthcare professional. Some medications and supplements may interact with botulinum toxin, so it is important to disclose this information.
- Infection at Injection Site: Avoid undergoing botulinum toxin treatments if you have an active infection or inflammation at the intended injection site. This includes conditions like cold sores, skin infections, or other localized infections. Treatment should be delayed until the infection or inflammation has resolved.
- Post-Treatment Care: Follow the post-treatment instructions provided by your healthcare professional. This may include avoiding touching or rubbing the treated area, refraining from strenuous exercise or activities that can increase blood flow to the treated area, and avoiding sun exposure or excessive heat.
- Side Effects and Complications: Be aware of the potential side effects and complications associated with botulinum toxin treatments. Common side effects may include temporary bruising, swelling, or mild discomfort at the injection site. In rare cases, more severe side effects or complications may occur. If you experience any concerning symptoms, contact your healthcare professional immediately.
Always consult with a qualified healthcare professional who specializes in botulinum toxin treatments to discuss your circumstances and any precautions specific to your situation. They will guide you on the appropriate precautions to take to ensure a safe and effective treatment experience.
Conclusion
In conclusion, botulinum toxin is a powerful neurotoxin derived from the bacterium Clostridium botulinum. It is widely used in both cosmetic and therapeutic applications to temporarily relax or paralyze muscles, resulting in various medical and aesthetic benefits. Botulinum toxin injections have proven to be effective in treating conditions such as facial wrinkles, muscle spasms, chronic migraines, excessive sweating, and certain neurological disorders. The toxin works by blocking the release of acetylcholine, a neurotransmitter that signals muscle contractions, leading to the desired therapeutic effects.
It is essential to seek guidance from qualified healthcare professionals who have expertise in administering botulinum toxin treatments. They will assess your individual needs, discuss the potential risks and benefits, and develop a personalized treatment plan. Open communication, informed consent, and adherence to post-treatment instructions are vital for optimal outcomes. While botulinum toxin treatments are generally safe, there are potential side effects and risks associated with its use. These can include temporary muscle weakness, bruising, pain at the injection site, flu-like symptoms, and, in rare cases, more severe complications. It is crucial to be aware of these risks and promptly communicate any concerns to your healthcare professional.
Proper storage, handling, and disposal of botulinum toxin are essential to ensure its integrity and prevent misuse. Always follow the recommended storage guidelines and dispose of any unused or expired products as directed by healthcare professionals or local regulations. In summary, botulinum toxin has revolutionized the field of medical aesthetics and therapeutic interventions. Its ability to temporarily relax muscles has provided significant benefits to patients with various conditions. By seeking expert advice, understanding the treatment process, and taking necessary precautions, individuals can experience safe and effective outcomes from botulinum toxin treatments.
FAQ
What does botulinum toxin do?
Intramuscular organization of botulinum poison acts at the neuromuscular intersection to cause muscle loss of motion by repressing the arrival of acetylcholine from presynaptic engine neurons.
Is botulinum toxin good or bad?
The antidote doesn’t invert muscle loss of motion or different side effects that have proactively happened, however, it can forestall the advancement of extra signs or side effects of the illness. Botulinum toxin is a very potent poison that can cause severe illness in humans in small amounts.
What is botulinum toxin for the face?
The bacterium Clostridium botulinum produces a toxin that is the basis for the drug known as Botox. A similar poison causes a perilous kind of food contamination called botulism. It is used in small amounts by doctors to treat the following health issues: Improvement of your appearance and temporary smoothing of facial wrinkles.
What amount does Botox cost in India?
Botox Infusion – Botulinum Poison Infusion Cost in India, Be that as it may, it tends to be anyplace between Rs 6000 to Rs 20000 relying upon the treatment(s) you are picking.
What kills botulinum toxin?
Just preparing or bubbling food annihilates botulinum poison. Freezing doesn’t annihilate the poison. Assuming you get ready or eat generally pre-arranged The Frozen North Local food sources, the sanitation tips underneath may diminish your gamble of botulism.
Can Botox affect your brain?
In a brief study, UCI researchers discovered that botox injections to the forehead may alter how a person’s brain interprets and processes emotions from others. It appears that people unconsciously imitate happy or angry faces when they see them.
Where not to inject Botox?
You ought to try not to infuse botulinum poison into the frontalis muscle, which is the muscle that causes a stir and curves your temple. Several other facial muscles, such as those that allow you to smile or chew, should also be avoided when using Botox.
Can botulinum toxin be cured?
A botulinum counteragent can be used to treat botulism if it is caught early. This prevents the poison from really hurting more in the body. However, muscle paralysis that has already occurred cannot be reversed by the antitoxin, so recovery can take weeks or even months.
At what age is Botox recommended?
Botox can be used to prevent the earliest signs of wrinkles from developing into full-blown wrinkles. The majority of experts agree that patients in their mid-to-late 20s and early 30s are a good age for preventative Botox treatment, and Botox is approved for patients over the age of 18.




7 Comments