Skeletal Muscle Relaxants
Introduction
Skeletal muscle relaxants are a class of medications that are primarily used to reduce muscle spasms and promote muscle relaxation. They work by targeting the skeletal muscle system, which is responsible for voluntary movements in the body. Skeletal muscle relaxants are commonly prescribed to treat conditions such as muscle spasms, muscle strains, sprains, and musculoskeletal disorders.
These medications act on the central nervous system (CNS) or directly on the muscles to provide relief from muscle stiffness, tension, and pain. They can be categorized into two main groups: centrally-acting muscle relaxants and direct-acting muscle relaxants.
Centrally acting muscle relaxants primarily work by targeting the CNS and exerting a sedative effect, which helps to reduce muscle spasms. Examples of centrally-acting muscle relaxants include drugs like baclofen, tizanidine, and diazepam. These medications are often prescribed for conditions such as multiple sclerosis, spinal cord injuries, and cerebral palsy.
Direct-acting muscle relaxants, on the other hand, act directly on the muscles themselves, interrupting the transmission of nerve impulses and causing muscle relaxation. One common example of a direct-acting muscle relaxant is dantrolene, which is used to treat conditions like malignant hyperthermia and spasticity associated with neurological disorders. It is important to note that skeletal muscle relaxants should be used under the supervision of a healthcare professional and as part of a comprehensive treatment plan.
They are typically prescribed for short-term use due to the potential for side effects such as drowsiness, dizziness, and impaired coordination. Additionally, some muscle relaxants have the potential for dependence or abuse, so they should be used with caution. Overall, skeletal muscle relaxants can be effective in relieving muscle spasms and promoting muscle relaxation in various conditions. However, the specific choice of muscle relaxant and the duration of treatment should be determined by a healthcare professional based on the individual’s condition and medical history.
What are Muscle Relaxers?
Muscle relaxers, also known as muscle relaxants, are medications that are prescribed to reduce muscle spasms, and muscle stiffness, and promote muscle relaxation. They work by targeting the skeletal muscle system, which is responsible for voluntary movements in the body. Muscle relaxers can be classified into two main categories: centrally-acting muscle relaxants and direct-acting muscle relaxants.
Centrally Acting Muscle Relaxants: These medications act on the central nervous system (CNS) to reduce muscle spasms. They work by depressing the activity of the nerves in the brain and spinal cord, which helps to calm and relax the muscles. Centrally acting muscle relaxants have a sedative effect and can cause drowsiness. Examples of centrally-acting muscle relaxants include:
- Baclofen
- Tizanidine
- Diazepam
- Carisoprodol
Direct-Acting Muscle Relaxants: Unlike centrally-acting muscle relaxants, direct-acting muscle relaxants act directly on the muscles themselves. They interfere with the transmission of nerve signals to the muscles, which leads to muscle relaxation. Direct-acting muscle relaxants are often used for specific conditions or muscle-related disorders. One example of a direct-acting muscle relaxant is dantrolene.
Muscle relaxers are commonly prescribed to treat conditions such as muscle spasms, muscle strains, sprains, and musculoskeletal disorders. They may be used in combination with other therapies such as physical therapy, rest, and pain management techniques to provide relief. It is important to note that muscle relaxers should be used under the guidance of a healthcare professional, as they can have potential side effects and interactions with other medications. They are typically prescribed for short-term use due to the risk of dependence and abuse. It is essential to follow the prescribed dosage and duration of treatment and communicate any concerns or adverse effects to your healthcare provider.
Are there over-the-counter Muscle Relaxers?
Yes, there are some over-the-counter (OTC) options available for muscle relaxation. These OTC muscle relaxers are generally milder compared to prescription-strength medications and are intended for temporary relief of minor muscle pain or discomfort. However, it is important to note that OTC muscle relaxers may not be as potent as prescription medications and may not be suitable for all conditions. It is always recommended to consult with a healthcare professional before using any medication, including OTC muscle relaxers.
Some common OTC options for muscle relaxation include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): OTC NSAIDs such as ibuprofen (Advil, Motrin) and naproxen (Aleve) can help reduce inflammation and relieve muscle pain and discomfort. While they primarily target pain and inflammation, they can also provide some mild muscle relaxation effects.
- Topical Analgesics: These are creams, gels, or patches that can be applied directly to the skin over the affected muscle area. They typically contain ingredients like menthol or camphor, which produce a cooling or warming sensation and may provide temporary relief from muscle pain and stiffness.
- Magnesium Supplements: Magnesium is an essential mineral that plays a role in muscle relaxation and nerve function. Some people find that taking magnesium supplements can help with muscle cramps and promote relaxation. Nonetheless, it is fitting to talk with a medical services proficient prior to beginning any new enhancements.
It is important to use OTC muscle relaxers as directed and be aware of any potential side effects or interactions with other medications you may be taking. If your symptoms persist or worsen, it is recommended to consult with a healthcare professional for a proper diagnosis and appropriate treatment options.
What are the types of Muscle Relaxers?
Healthcare providers in the United States can also currently specify the subsequent antispasmodic skeletal muscle relaxants:
- Carisoprodol (Soma®, Vanadom®).
- Chlorzoxazone (Lorzone®, Parafon Forte DSC®, Relax-DS®, and Remular S®).
- Cyclobenzaprine (Fexmid®, Flexeril®).
- Metaxalone (Metaxall®, Skelaxin®).
- Methocarbamol (Robaxin®).
- Orphenadrine (Norflex®).
Antispastic skeletal muscle relaxants that providers can also currently prescribe in the U.S. contain:
- Baclofen (Lioresal®).
- Dantrolene (Dantrium®).
Antispasmodic and antispastic effects can be found in two skeletal muscle relaxants. They enclose:
- Tizanidine (Zanaflex®).
- Diazepam (Valium®).
classification of skeletal muscle relaxants
Skeletal muscle relaxants can be classified into different categories based on their mechanism of action or chemical structure. Here are some common classifications of skeletal muscle relaxants:
A centrally-acting drug like,
- Diazepam and other benzodiazepins
- Methocarbamol
- Chlorzoxazone
- Tizanidine
- Baclofen
- Gabapentin
Peripheral drug acting includes acting drugs at the neuromuscular junction and drugs directly acting on skeletal muscle. They are as follows:
Drugs directly acting on skeletal muscle like,
- Dantrolene
Drug acting at the neuromuscular junction, which further classified into other categories which are as follow:
Deloparizing blockers,
- succinylcholine
- Decamethonium
Non-depolarizing blockers, (competitive blockers)
- d-TC
- Atracurium
- Rocuronium
- Pancuronium
- Vecuronium
- Doxacuronium
- Pipecuronium
- Mivacurium
others
- Botulinum toxin A
What do muscle relaxers help treat?
Even though antispastics and antispasmodics are the two kinds of skeletal muscle relaxants, they have explicit and various purposes. Additionally, some of these drugs treat conditions that have nothing to do with muscle function. Diazepam, for instance, is sometimes prescribed by doctors to treat seizures and anxiety. Muscle relaxers, or muscle relaxants, are medications that can help treat various conditions characterized by muscle spasms, muscle stiffness, and related symptoms. Let’s explore in detail some of the specific conditions that muscle relaxers can help treat:
- Muscle Spasms: Muscle relaxers are commonly used to alleviate muscle spasms. Muscle spasms are involuntary contractions of the muscles that can cause pain, discomfort, and restricted movement. Muscle relaxers work by reducing the intensity and frequency of spasms, promoting muscle relaxation, and relieving associated symptoms.
- Musculoskeletal Disorders: Muscle relaxants can be prescribed to manage musculoskeletal disorders such as fibromyalgia, myofascial pain syndrome, and temporomandibular joint (TMJ) disorders. These conditions are often characterized by chronic muscle pain, tension, and spasms. Muscle relaxers help alleviate muscle stiffness and pain, enabling individuals to engage in daily activities with greater comfort.
- Back Pain: Muscle relaxers are commonly included in the treatment plan for acute or chronic back pain, particularly when muscle spasms contribute to the discomfort. By reducing muscle spasms and promoting muscle relaxation, these medications can help alleviate back pain and improve mobility.
- Sprains and Strains: Muscle relaxants can aid in the management of muscle strains and sprains, which typically occur due to overexertion or injury. These conditions often involve damage to the muscles or ligaments, resulting in pain, swelling, and muscle spasms. Muscle relaxers help alleviate muscle tension and spasms, allowing the injured tissues to heal more effectively.
- Spinal Cord Injuries: Muscle relaxers are sometimes prescribed to individuals with spinal cord injuries. Spinal cord injuries can lead to muscle spasticity, which is characterized by excessive and uncontrollable muscle contractions. Muscle relaxants help reduce spasticity, muscle stiffness, and spasms, improving mobility and enhancing the overall quality of life.
- Multiple Sclerosis (MS): MS is a chronic autoimmune disease that affects the central nervous system, resulting in communication difficulties between the brain and muscles. Muscle relaxers can be used to manage muscle spasticity, stiffness, and spasms that are common in individuals with MS. By promoting muscle relaxation, these medications help improve mobility and reduce associated symptoms.
- Cerebral Palsy: Cerebral palsy is a neurological disorder that affects muscle control and movement. Muscle relaxants are beneficial in managing muscle spasticity, which is a common symptom in individuals with cerebral palsy. By reducing spasticity, muscle stiffness, and spasms, muscle relaxers can enhance mobility, increase flexibility, and improve overall function.
It is important to note that muscle relaxers should always be used under the guidance and supervision of a healthcare professional. The specific choice of muscle relaxant, dosage, and treatment duration will depend on the individual’s condition, symptoms, overall health, and potential interactions with other medications.
How common are muscle relaxants?
Muscle relaxants are commonly prescribed medications and are frequently used to treat various conditions involving muscle spasms and muscle-related symptoms. The exact prevalence and usage of muscle relaxants may vary based on factors such as geographic location, healthcare practices, and specific patient populations. However, muscle relaxants are widely prescribed and utilized in clinical practice. Here are a few points to consider regarding the commonness of muscle relaxants:
- Prescribing Frequency: Muscle relaxants are among the most commonly prescribed medications in the United States. They are frequently prescribed by healthcare professionals, including general practitioners, orthopedic specialists, neurologists, and pain management specialists, to manage a range of conditions that involve muscle spasms, such as back pain, musculoskeletal injuries, and certain neurological disorders.
- Conditions Treated: Muscle relaxants are used to treat a variety of conditions, including muscle spasms, sprains, strains, fibromyalgia, myofascial pain syndrome, multiple sclerosis, spinal cord injuries, and cerebral palsy. These conditions are relatively common, and muscle relaxants are often included as part of the treatment plan to provide relief from associated symptoms.
- Short-Term Usage: Muscle relaxants are typically prescribed for short-term use, ranging from a few days to a few weeks. They are often used during the acute phase of muscle spasms or injuries to alleviate pain, reduce muscle tension, and improve functional ability. Long-term usage of muscle relaxants may be limited due to the potential for side effects and the risk of dependence.
- Multimodal Approach: In many cases, muscle relaxants are not used as the sole treatment but as part of a comprehensive approach that includes physical therapy, rest, pain management techniques, and other interventions. This multimodal approach aims to address the underlying cause of muscle spasms and promote overall recovery.
It is important to note that the use of muscle relaxants should be based on a proper evaluation and diagnosis by a healthcare professional. The specific usage patterns may vary depending on the individual patient, the severity of the condition, and the treatment goals. It is recommended to follow the prescribed dosage, duration, and guidelines provided by the healthcare professional when using muscle relaxants.
What function do sedatives serve?
Skeletal muscle relaxants come in a variety of brands and types, and their effects on muscle function vary. The majority of muscle relaxants prevent your nerves from sending pain signals to your brain and either cause a sedative effect or depress the central nervous system. By directly targeting the spinal cord or skeletal muscle, antispasmodic medications typically improve muscle tightness (hypertonicity) and involuntary spasms. Antispasmodic medications lessen muscle spasms by altering your central nervous system (brain and spinal cord).
The function of skeletal muscle relaxant
The primary function of skeletal muscle relaxants is to reduce muscle spasms, muscle tension, and associated pain. These medications act on the skeletal muscle system to promote relaxation, decrease muscle hyperactivity, and improve mobility. Here are some specific functions and effects of skeletal muscle relaxants:
- Muscle Relaxation: Skeletal muscle relaxants work by targeting the neuromuscular junction, the point where nerves connect with muscle fibers. They act on the central nervous system (CNS) or directly on muscle cells to reduce the excitability of muscle fibers, leading to muscle relaxation. This relaxation can help alleviate muscle spasms, cramps, and associated discomfort.
- Pain Relief: Muscle spasms and tension often cause pain. Skeletal muscle relaxants can help relieve pain by reducing muscle contractions and relaxing the muscles. By promoting muscle relaxation, they can help alleviate muscle-related pain, whether it is due to acute injuries, chronic conditions, or musculoskeletal disorders.
- Increased Range of Motion: Muscle relaxants can improve the range of motion by reducing muscle stiffness and tension. By relaxing the muscles, these medications can enhance flexibility and make movement easier, allowing individuals to engage in activities with less restriction and discomfort.
- Improved Functional Mobility: Skeletal muscle relaxants can improve functional mobility in individuals who experience muscle spasms or stiffness. By reducing muscle hyperactivity, these medications can enhance coordination, balance, and overall physical performance, making it easier for individuals to carry out daily activities.
- Facilitation of Physical Therapy: Muscle relaxants are sometimes prescribed in conjunction with physical therapy. By promoting muscle relaxation, these medications can enhance the effectiveness of therapeutic exercises and techniques used in rehabilitation. This can aid in the recovery process for individuals with musculoskeletal injuries or conditions.
It’s important to note that while skeletal muscle relaxants can provide symptomatic relief, they do not address the underlying cause of muscle spasms or pain. They are typically used as part of a comprehensive treatment plan that may include other interventions such as physical therapy, exercise, stretching, and lifestyle modifications. The specific function and effectiveness of skeletal muscle relaxants can vary depending on the individual, the specific medication used, and the underlying condition being treated. It’s important to consult with a healthcare professional who can determine the most appropriate muscle relaxant and treatment approach for your specific needs.
How do you take muscle relaxers?
The specific instructions for taking muscle relaxers can vary depending on the medication prescribed and the individual’s condition. It is essential to follow the guidance of your healthcare professional and the instructions provided with the medication. Here are some general guidelines for taking muscle relaxers:
- Prescription and Dosage: Muscle relaxers are typically prescribed by a healthcare professional. They will determine the appropriate medication, dosage, and duration of treatment based on your condition, symptoms, medical history, and other relevant factors. It is important to follow the prescribed dosage and not exceed or alter it without consulting your healthcare provider.
- Timing and Frequency: Muscle relaxers are usually taken orally, with or without food, as instructed by your healthcare professional. The timing and frequency of the doses can vary depending on the specific medication. Some muscle relaxers may be taken multiple times a day, while others may be taken as a single dose. Follow the prescribed schedule carefully and ensure you understand the instructions for timing and frequency.
- Duration of Treatment: Muscle relaxers are often prescribed for short-term use, typically ranging from a few days to a few weeks. They are primarily used during the acute phase of muscle spasms, injuries, or specific conditions. Longer-term use may be considered in certain cases, but it is important to discuss this with your healthcare provider due to potential side effects and the risk of dependence.
- Precautions and Interactions: Be sure to inform your healthcare professional about any other medications, supplements, or medical conditions you have before starting muscle relaxers. Certain medications, such as sedatives, opioids, or alcohol, can interact with muscle relaxants and increase the risk of side effects. Additionally, inform your healthcare provider if you are pregnant, breastfeeding, or have any liver or kidney issues, as these factors can impact the choice and dosage of muscle relaxers.
- Follow-up and Monitoring: Regular follow-up appointments with your healthcare provider are important to assess the effectiveness of the muscle relaxers and any potential side effects. They can make any necessary adjustments to the treatment plan based on your progress and overall response to the medication.
Always confer with your healthcare professional for specific instructions on how to take muscle relaxers, as they can also provide personalized guidance established on your unique situation. Be sure to follow them.
How effective are muscle relaxants?
Antispastic meds are viable in treating spasticity, however, high dosages can prompt undesirable aftereffects. Spasticity can be treated with physical therapy and Botox® injections, among other treatments. There is a lack of research on whether antispasmodics are more effective than NSAIDs or acetaminophen in treating muscle spasms and pain. Antispasmodics have more aftereffects than NSAIDs and acetaminophen, so it means a lot to converse with your medical care supplier about the advantages and dangers of taking these meds.
What are the side effects of muscle relaxers?
Muscle relaxers, like any medication, can potentially cause a range of side effects. The specific side effects can vary depending on the specific muscle relaxant prescribed, individual factors, and dosage. It is important to consult with your healthcare professional and carefully read the information provided with the medication for a comprehensive understanding of potential side effects. Here are some common side effects associated with muscle relaxers:
- Drowsiness and Sedation: Many muscle relaxants have a sedative effect on the central nervous system, which can cause drowsiness, sleepiness, and reduced alertness. This can interfere with daily activities and may increase the risk of accidents, especially when operating machinery or driving a vehicle. It is important to use caution and avoid activities that require mental alertness until you know how the medication affects you.
- Dry Mouth: Muscle relaxants can lead to a dry mouth or throat, known as xerostomia. This can cause discomfort, difficulty speaking or swallowing, and an increased risk of dental issues. Staying hydrated, using sugar-free gum or candies, or using saliva substitutes can help alleviate the dryness.
- Dizziness and Lightheadedness: Some individuals may experience dizziness or feelings of lightheadedness when taking muscle relaxers. This can result in unsteadiness, difficulty with balance, or a sensation of spinning (vertigo). It is important to avoid sudden movements, get up slowly from a seated or lying position, and take necessary precautions to prevent falls or accidents.
- Cognitive Impairment: Muscle relaxants can sometimes cause cognitive side effects, including confusion, difficulty concentrating, memory problems, or slowed thinking. These effects can impact daily activities and mental performance.
- Blurred Vision: Certain muscle relaxants may cause temporary blurred vision or difficulty focusing. If you experience changes in your vision while taking muscle relaxers, it is important to discuss it with your healthcare provider.
- Gastrointestinal Effects: Muscle relaxants can sometimes lead to gastrointestinal side effects such as nausea, stomach discomfort, indigestion, or constipation. Adequate hydration, a balanced diet, and dietary fiber intake may help alleviate these symptoms. In some cases, your healthcare provider may recommend additional measures or medications to manage gastrointestinal side effects.
- Allergic Reactions: Although rare, allergic reactions to muscle relaxers can occur. Signs of an allergic reaction may include skin rash, itching, swelling (especially of the face, lips, or tongue), dizziness, difficulty breathing, or hives. If any of these symptoms occur, see a doctor right away.
- Other Side Effects: Muscle relaxants can have additional side effects that vary depending on the specific medication. These may include headaches, muscle weakness, changes in heart rate, low blood pressure, urinary retention, urinary frequency, or mood changes. It is important to be aware of the potential side effects associated with the specific muscle relaxant you are taking.
It’s important to note that not everyone will experience side effects, and the severity and occurrence of side effects can vary from person to person. If you have concerns about the side effects of muscle relaxers, discuss them with your healthcare professional. They can offer you advice that is tailored to your particular circumstance.
Do muscle relaxers make you sleepy?
Yes, muscle relaxers can cause drowsiness and make you sleepy. Many muscle relaxants have a sedative effect on the central nervous system, which can result in feelings of sleepiness and reduced alertness. This drowsiness can make it difficult to stay awake and perform daily activities that require mental focus or coordination. It is important to note that the degree of sleepiness can vary among individuals and can be influenced by factors such as the specific muscle relaxant prescribed, the dosage, and individual sensitivity. Some muscle relaxants are known to cause more sedation than others. Additionally, combining muscle relaxers with other sedating medications or alcohol can intensify the sedative effects and increase the likelihood of feeling excessively sleepy or fatigued.
If you experience significant drowsiness or sleepiness while taking muscle relaxers, it is crucial to avoid engaging in activities that may pose a risk, such as driving, operating machinery, or participating in activities where being alert is essential. It is advisable to discuss any concerns about excessive sleepiness with your healthcare professional, as they can help adjust the dosage or consider alternative treatment options if necessary.
Mechanism of action of Skeletal muscle relaxants
Skeletal muscle relaxants work by targeting various mechanisms in the body to reduce muscle spasms, muscle tone, and muscle-related pain. The specific mechanism of action can vary depending on the type of muscle relaxant. Here are some common mechanisms of action for skeletal muscle relaxants:
- Central Nervous System (CNS) Depressants: Many skeletal muscle relaxants, including benzodiazepines like diazepam (Valium) and non-benzodiazepines like cyclobenzaprine (Flexeril), exert their effects by acting as CNS depressants. They enhance the inhibitory effects of the neurotransmitter gamma-aminobutyric acid (GABA) in the brain and spinal cord, resulting in a sedative and muscle-relaxing effect.
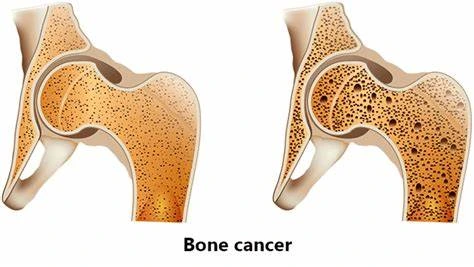
- Calcium Channel Blockers: Some muscle relaxants, such as dantrolene (Dantrium), act by blocking calcium release from the sarcoplasmic reticulum within muscle cells. By inhibiting calcium release, they reduce the contractility of skeletal muscle fibers and thereby decrease muscle spasms.
- NMDA Receptor Antagonists: Certain muscle relaxants, like methocarbamol (Robaxin), can act as N-methyl-D-aspartate (NMDA) receptor antagonists. NMDA receptors play a role in transmitting pain signals. By blocking these receptors, these muscle relaxants can help alleviate pain associated with muscle spasms and tension.
- GABA Receptor Agonists: Baclofen is a muscle relaxant that acts by stimulating GABA receptors in the central nervous system. By increasing GABA activity, it inhibits the transmission of signals within the spinal cord, reducing muscle spasticity and promoting muscle relaxation.
- Direct Muscle Relaxation: Some muscle relaxants, such as chlorzoxazone (Parafon Forte), have a direct effect on skeletal muscle fibers. They may interfere with the excitation-contraction coupling process in muscle cells, reducing muscle hyperactivity and spasms.
It’s important to note that the specific mechanism of action can vary among different muscle relaxants, and some may have additional effects beyond their primary mechanisms. Additionally, the exact way in which these medications work may not be fully understood for some muscle relaxants.
The choice of muscle relaxant and its mechanism of action will depend on the individual’s condition, severity of symptoms, and other factors. It is crucial to consult with a healthcare professional who can determine the most appropriate muscle relaxant for your specific needs.
pharmacological action of Skeletal muscle relaxants
The pharmacological action of skeletal muscle relaxants involves targeting various mechanisms in the body to achieve muscle relaxation. The specific pharmacological actions can vary depending on the type of muscle relaxant. Here are some common pharmacological actions associated with skeletal muscle relaxants:
- Central Nervous System (CNS) Depression: Many skeletal muscle relaxants, such as benzodiazepines and some non-benzodiazepines, exert their effects by acting as CNS depressants. They enhance the inhibitory effects of the neurotransmitter gamma-aminobutyric acid (GABA) in the brain and spinal cord, leading to sedation, reduced muscle tone, and muscle relaxation.
- Neuromuscular Junction (NMJ) Blockade: Certain muscle relaxants, such as non-depolarizing neuromuscular blockers like pancuronium or vecuronium, act by blocking the action of acetylcholine at the neuromuscular junction. This blockade prevents the transmission of nerve impulses to the muscle fibers, resulting in muscle paralysis and relaxation.
- Calcium Channel Blockade: Some muscle relaxants, like dantrolene, act by blocking calcium release from the sarcoplasmic reticulum within muscle cells. By inhibiting calcium release, they reduce the contractility of skeletal muscle fibers, leading to muscle relaxation.
- GABA Receptor Modulation: Muscle relaxants such as baclofen and tizanidine exert their effects by modulating GABA receptors in the CNS. They either stimulate specific GABA receptors (GABA-B agonists) or enhance GABA-mediated inhibitory neurotransmission. This modulation leads to reduced muscle hyperactivity, decreased muscle spasms, and relaxation.
- NMDA Receptor Antagonism: Some muscle relaxants, like methocarbamol and ketamine, can act as N-methyl-D-aspartate (NMDA) receptor antagonists. NMDA receptors play a role in transmitting pain signals. By blocking these receptors, these muscle relaxants can help alleviate pain associated with muscle spasms and tension.
It’s important to note that the specific pharmacological actions and mechanisms of different muscle relaxants can vary. Additionally, some muscle relaxants may have multiple pharmacological actions that contribute to their overall effects. The choice of muscle relaxant and its pharmacological action will depend on the individual’s condition, the severity of symptoms, and other factors. It is crucial to consult with a healthcare professional who can evaluate your specific situation and determine the most appropriate muscle relaxant and treatment approach for your needs.
the half-life of Skeletal muscle relaxants
The half-life of skeletal muscle relaxants can vary depending on the specific medication. The time it takes for a drug’s concentration in the body to drop by half is known as the half-life. Here are the approximate half-lives of some commonly used skeletal muscle relaxants:
- Diazepam (Valium): The half-life of diazepam is approximately 20 to 100 hours, but its active metabolite, desmethyldiazepam, has a longer half-life of around 36 to 200 hours.
- Cyclobenzaprine (Flexeril): The half-life of cyclobenzaprine is approximately 18 hours.
- Carisoprodol (Soma): The half-life of carisoprodol is approximately 1 to 3 hours, but its active metabolite, meprobamate, has a longer half-life of around 6 to 17 hours.
- Methocarbamol (Robaxin): The half-life of methocarbamol is approximately 1 to 2 hours.
- Tizanidine (Zanaflex): The half-life of tizanidine is approximately 2.5 to 4.5 hours.
- Baclofen (Lioresal): The half-life of baclofen is approximately 1.5 to 4 hours.
These half-life values are approximate and can vary depending on individual factors such as metabolism, age, liver function, and other medications being taken. It is important to note that the half-life of a drug does not determine its duration of action, as the effects of the medication can extend beyond its half-life due to factors like accumulation in tissues. It is crucial to consult with a healthcare professional or refer to the specific medication’s prescribing information for accurate and up-to-date information on the half-life and dosing regimen of a particular skeletal muscle relaxant.
Administration of Skeletal muscle relaxants
Skeletal muscle relaxants can be administered through various routes depending on the specific medication and the severity of the condition being treated. Here are the common routes of administration for skeletal muscle relaxants:
- Oral Administration: Most skeletal muscle relaxants are available in oral tablet or capsule form. The most prevalent method of administration is this one. The medication is swallowed with water and absorbed into the bloodstream through the gastrointestinal tract.
- Intravenous (IV) Administration: In certain cases where immediate onset of action is required, skeletal muscle relaxants can be administered intravenously. This involves injecting the medication directly into a vein, allowing for rapid absorption and onset of effects. IV administration is typically done in a healthcare setting under the supervision of a healthcare professional.
- Intramuscular (IM) Administration: Skeletal muscle relaxants can also be administered via intramuscular injection. This involves injecting the medication into a muscle, allowing for gradual absorption into the bloodstream. IM injections are less common for muscle relaxants and are typically reserved for specific situations or when oral administration is not feasible.
It is important to follow the specific instructions provided by your healthcare professional or as indicated on the medication label. The dosage, frequency, and duration of administration will vary depending on the individual’s condition, the specific skeletal muscle relaxant, and other factors. Additionally, it’s important to note that some skeletal muscle relaxants, such as creams or gels containing topical muscle relaxants, can be applied directly to the affected area of the body. This allows for localized absorption and targeted relief of muscle spasms or pain. Always consult with your healthcare professional for proper administration instructions and to determine the most appropriate route and dosage of a skeletal muscle relaxant for your specific condition.
route of elimination of Skeletal muscle relaxants
The route of elimination of skeletal muscle relaxants can vary depending on the specific medication. Here are some common routes of elimination for skeletal muscle relaxants:
- Renal Elimination: Many skeletal muscle relaxants are primarily eliminated from the body through the kidneys. After metabolism in the liver, the drug or its metabolites are excreted in the urine. This includes medications like diazepam, cyclobenzaprine, and tizanidine. It is important to note that dose adjustments may be necessary for individuals with impaired kidney function to prevent the accumulation of the medication.
- Hepatic Elimination: Some skeletal muscle relaxants are metabolized in the liver and eliminated through bile. This includes medications like carisoprodol and meprobamate, where the majority of the elimination occurs through hepatic metabolism and subsequent excretion in the feces. Liver function should be considered when using these medications, especially in individuals with hepatic impairment.
- Mixed Elimination: Certain skeletal muscle relaxants undergo both renal and hepatic elimination to varying extents. For example, methocarbamol is primarily eliminated through the kidneys, but it also undergoes hepatic metabolism to a lesser extent.
- Other Elimination Routes: Some skeletal muscle relaxants may have additional elimination routes. For instance, dantrolene, which is used for specific conditions like malignant hyperthermia, is primarily eliminated through the bile, but a portion of the drug is also excreted unchanged in the urine.
It is important to note that the elimination routes and metabolism of skeletal muscle relaxants can vary among individuals, and factors such as liver or kidney dysfunction can affect the elimination process. It’s recommended to consult with a healthcare professional or refer to the specific medication’s prescribing information for accurate and up-to-date information on the elimination routes and considerations for a particular skeletal muscle relaxant. Before taking any medication, confer with your medic.
Are muscle relaxers addictive?
Muscle relaxers have the potential to be addictive, especially if they belong to a class of medications called benzodiazepines. Benzodiazepine muscle relaxants, such as diazepam (Valium) or carisoprodol (Soma), have a higher risk of addiction and dependence compared to other types of muscle relaxants. Long-term and high-dose use of benzodiazepine muscle relaxants can lead to physical and psychological dependence. Physical dependence means that your body becomes accustomed to the presence of the medication and experiences withdrawal symptoms when you try to stop using it. Psychological dependence refers to a strong desire or craving for the medication due to its perceived calming or euphoric effects.
It’s important to note that not all muscle relaxants have the same addictive potential. Other types of muscle relaxants, such as non-benzodiazepine medications like methocarbamol (Robaxin) or cyclobenzaprine (Flexeril), have a lower risk of addiction and dependence. However, even with these medications, long-term use and misuse can still lead to dependency. To minimize the risk of addiction and dependence, it is crucial to follow your healthcare professional’s instructions and take muscle relaxers as prescribed. Avoid increasing the dosage or using the medication for longer than recommended. If you have a history of substance abuse or addiction, it is essential to inform your healthcare provider so they can consider alternative treatment options or closely monitor your use of muscle relaxants.
If you experience symptoms of dependence, such as cravings, withdrawal symptoms, or an inability to stop using the medication despite negative consequences, it is important to seek help from your healthcare professional. They can provide guidance and support in tapering off the medication safely and exploring alternative treatment options for your condition.
What are the possible troubles or complications of enduring muscle relaxers?
Taking muscle relaxers, like any medication, carries certain risks and potential complications. It’s important to be aware of these risks and discuss them with your healthcare professional. Here are some possible risks or complications associated with the use of muscle relaxers:
- Sedation and Impaired Alertness: Many muscle relaxants can cause drowsiness, sedation, and impaired alertness. This can increase the risk of accidents, falls, and decreased cognitive function, particularly when operating machinery, driving, or engaging in activities that require mental focus and coordination.
- Drug Interactions: Muscle relaxers can interact with other medications, including over-the-counter drugs, herbal supplements, and prescription medications. These interactions can lead to increased sedation, respiratory depression, or other adverse effects. It is important to inform your healthcare professional about all the medications you are taking to avoid potential drug interactions.
- Dependency and Withdrawal: Some muscle relaxers, especially benzodiazepine-based ones, have the potential for dependence and withdrawal symptoms with long-term or high-dose use. Abruptly stopping these medications can lead to withdrawal symptoms such as rebound muscle spasms, anxiety, insomnia, and seizures. It’s important to follow your healthcare professional’s instructions for tapering off muscle relaxers if discontinuing their use.
- Allergic Reactions: While rare, allergic reactions to muscle relaxers can occur. Signs of an allergic reaction may include skin rash, itching, swelling (particularly of the face, lips, or tongue), dizziness, difficulty breathing, or hives. Look for surefire clinical consideration assuming that you experience any of these side effects.
- Gastrointestinal Effects: Muscle relaxants can sometimes cause gastrointestinal side effects such as nausea, stomach discomfort, indigestion, or constipation. Adequate hydration, a balanced diet, and dietary fiber intake may help alleviate these symptoms. Your healthcare provider may recommend additional measures or medications to manage gastrointestinal side effects.
- Pre-existing Medical Conditions: Muscle relaxants may have specific risks or considerations for individuals with certain pre-existing medical conditions. For example, individuals with liver or kidney disease may require dosage adjustments or close monitoring. It’s important to disclose your medical history to your healthcare professional so they can determine the appropriateness and safety of muscle relaxant use.
It’s essential to closely follow the instructions provided by your healthcare professional and report any concerning symptoms or side effects. They can monitor your response to the medication, make adjustments as needed, and provide appropriate guidance to minimize the risks and complications associated with muscle relaxers.
When should I contact my physician?
You ought to have customary meetings with your medical care supplier while taking a muscle relaxant to evaluate how well it’s functioning.
If not, consult your doctor in the following circumstances:
- if you experience unpleasant side effects.
- if your symptoms have gotten worse or are not getting better.
- On the off chance that you believe you are fostering a reliance on the drug.
Are skeletal muscle relaxants safe?
Skeletal muscle relaxants, when used as prescribed and under the supervision of a healthcare professional, are generally considered safe. However, there are potential dangers and things to keep in mind, just like with any medication. Here are some important points regarding the safety of skeletal muscle relaxants:
- Adverse Effects: Skeletal muscle relaxants can cause side effects, as discussed earlier. These can range from mild and temporary effects like drowsiness, dry mouth, or dizziness, to more serious reactions such as allergic reactions. It’s important to be aware of the potential side effects and promptly report any concerning symptoms to your healthcare professional.
- Individual Variations: The safety and tolerability of muscle relaxants can vary among individuals. Factors such as age, overall health, other medications being taken, and individual sensitivity can influence how a person responds to a muscle relaxant. Your healthcare professional will consider these factors when prescribing and monitoring your treatment.
- Drug Interactions: Muscle relaxants can interact with other medications, including prescription drugs, over-the-counter medications, and herbal supplements. These interactions can lead to increased side effects or reduced effectiveness of either medication. It’s crucial to inform your healthcare professional about all the medications you are taking to avoid potential drug interactions.
- Dependency and Addiction: Certain muscle relaxants, particularly benzodiazepine-based ones, have a higher risk of dependency and addiction when used long-term or in high doses. It’s important to follow your healthcare professional’s instructions and use muscle relaxants only as prescribed to minimize the risk of dependence.
- Pre-existing Conditions: Some individuals with specific medical conditions may require caution or dosage adjustments when taking skeletal muscle relaxants. For example, individuals with liver or kidney disease may need careful monitoring. It’s important to inform your healthcare professional about any pre-existing medical conditions you have to ensure the medication is safe for you.
- Pregnancy and Breastfeeding: The safety of muscle relaxants during pregnancy and breastfeeding varies depending on the specific medication. Some muscle relaxants may carry risks to the developing fetus or nursing infant. If you are pregnant, planning to become pregnant, or breastfeeding, it’s important to discuss the potential risks and benefits with your healthcare professional.
It’s important to note that skeletal muscle relaxants should be used under the guidance and supervision of a healthcare professional who can assess your specific condition, weigh the potential risks and benefits, and monitor your response to the medication. They can provide personalized recommendations to ensure the safe use of skeletal muscle relaxants in your particular situation.
Who can take Skeletal muscle relaxants?
Certainly! Here is a more detailed breakdown of specific conditions and who can take skeletal muscle relaxants:
- Muscle Spasms and Spasticity: Skeletal muscle relaxants are commonly prescribed for individuals experiencing muscle spasms or spasticity due to conditions such as:
- Muscle strains or sprains
- Musculoskeletal injuries
- Conditions like multiple sclerosis (MS), cerebral palsy, or spinal cord injury
- Muscle relaxants can help reduce muscle spasms, promote relaxation, and improve mobility.
- Back Pain and Neck Pain: Skeletal muscle relaxants can be beneficial for individuals with acute or chronic back pain or neck pain, particularly if muscle spasms contribute to the discomfort. Muscle relaxants help relax the muscles, alleviate pain, and improve range of motion.
- Fibromyalgia: Chronic fibromyalgia is characterized by widespread pain, fatigue, and tenderness in the musculoskeletal system. Muscle relaxants can be prescribed to individuals with fibromyalgia to manage muscle pain, reduce spasms, and improve overall comfort.
- Spinal Conditions: Skeletal muscle relaxants may be used in individuals with spinal conditions such as herniated discs, spinal stenosis, or degenerative disc disease. These conditions can cause muscle spasms and pain, and muscle relaxants can help provide relief and improve functional mobility.
- Post-Operative Recovery: Muscle relaxants may be used as part of postoperative pain management strategies, especially after orthopedic surgeries or procedures that involve muscle manipulation. They can help reduce muscle spasms, alleviate pain, and promote healing during the recovery period.
- Other Conditions: Skeletal muscle relaxants may also be prescribed in certain situations for conditions such as:
- TMJ (temporomandibular joint) disorders that involve muscle tension and pain in the jaw
- Migraine headaches with associated muscle tension and spasms
- Restless leg syndrome, where muscle relaxants can help reduce leg discomfort and spasms
It’s important to note that the decision to prescribe skeletal muscle relaxants is made on an individual basis, taking into account factors such as the severity of symptoms, the underlying condition, overall health, and potential interactions with other medications. Your healthcare professional will evaluate your specific situation and determine the appropriateness of muscle relaxant therapy based on your condition and needs.
Who can’t take Skeletal muscle relaxants?
While skeletal muscle relaxants can be beneficial for many individuals, there are certain situations or conditions where their use may be contraindicated or require caution. Here are some examples of individuals who may not be able to take skeletal muscle relaxants or may require careful consideration:
- Allergies or Sensitivity: If an individual has a known allergy or hypersensitivity to a specific skeletal muscle relaxant or its components, they should not take that particular medication. It’s important to inform your healthcare professional about any known allergies or adverse reactions to medications.
- Respiratory Impairment: Skeletal muscle relaxants can have sedative effects, which may cause respiratory depression or suppression, particularly in individuals with underlying respiratory conditions such as chronic obstructive pulmonary disease (COPD) or sleep apnea. Caution is required in such cases, and alternative treatment options may need to be considered.
- Liver or Kidney Dysfunction: Skeletal muscle relaxants are primarily metabolized and eliminated from the body through the liver and kidneys. Individuals with impaired liver or kidney function may require dosage adjustments or need to avoid certain muscle relaxants altogether to prevent the accumulation of the medication or its metabolites in the body.
- History of Substance Abuse or Addiction: Some muscle relaxants, particularly benzodiazepines, carry a risk of dependence and addiction. Individuals with a history of substance abuse or addiction may be advised against taking these medications or may require careful monitoring and alternative treatment options.
- Pregnancy and Breastfeeding: The safety of skeletal muscle relaxants during pregnancy and breastfeeding varies depending on the specific medication. Some muscle relaxants may carry risks to the developing fetus or nursing infant. It’s important to discuss the potential risks and benefits with your healthcare professional if you are pregnant, planning to become pregnant, or breastfeeding.
- Interaction with Other Medications: Skeletal muscle relaxants can interact with other medications, including prescription drugs, over-the-counter medications, and herbal supplements. These interactions can affect the effectiveness or increase the risk of side effects of either medication. It’s crucial to inform your healthcare professional about all the medications you are taking to avoid potential drug interactions.
It’s important to remember that this is not an exhaustive list, and individual circumstances can vary. It’s essential to consult with a healthcare professional who can assess your specific condition, medical history, and potential risk factors to determine the suitability of skeletal muscle relaxants for you.
FAQ
Why are muscle relaxants used in the body?
Skeletal muscle relaxants are primarily used to treat: spasticity is another term for muscles that are stiff and rigid due to stroke, multiple sclerosis, or cerebral palsy.
What is the most secure skeletal muscle relaxant?
Metaxalone – Taken as 800 mg tablets 3 to 4 times each day, metaxalone (Skelaxin) makes the least detailed side impacts. Furthermore, it is the least likely of the muscle relaxants to induce sleepiness. It might be more effective for flare-ups of chronic lower back pain than for new pain.
Is gabapentin a sedative?
Gabapentin is an anticonvulsive prescription that was initially considered used to be a muscle relaxer and hostile to fitful medicine, yet later it was found it had the capability of the drug as an anticonvulsive prescription and as an assistant to additional strong anticonvulsants.
Which is the quickest-acting muscle relaxant?
Due to its rapid onset and short duration, succinylcholine has traditionally been the most commonly used muscle relaxant for this purpose. Sadly, it may have serious negative effects.
What is the most grounded normal muscle relaxer?
The most effective natural muscle relaxants and their application These include the foods, supplements, and methods listed below:
Cherries and tart cherry juice. Share on Pinterest Tart cherry juice and cherries may naturally relax muscles. Berries of blue, Protein, Magnesium, curcumin, Pomegranate juice, Arnica, and Capsaicin.
Which muscle relaxant is alright for older?
Baclofen and tizanidine, two muscle relaxants, can be used by older people, subject to kidney and liver function once more. In cases of common spine-related pain that does not respond to treatment, opioids are only used sparingly.
What is a genuine muscle relaxer?
Muscle relaxants, also referred to as skeletal muscle relaxants, are a diverse class of drugs that can relax or alleviate muscle tension. Some, such as baclofen, methocarbamol, and tizanidine, forestall nerve pathways in the mind or spinal string from becoming overexcited.
What’s the most elevated mg for muscle relaxers?
For the tablet form of administration: 10 milligrams (mg) three times a day for adults and children over the age of 15 The biggest sum ought to be something like 60 mg (six 10-mg tablets) a day.





6 Comments