Causalgia (Complex Regional Pain Syndrome Type II):
What is Causalgia?
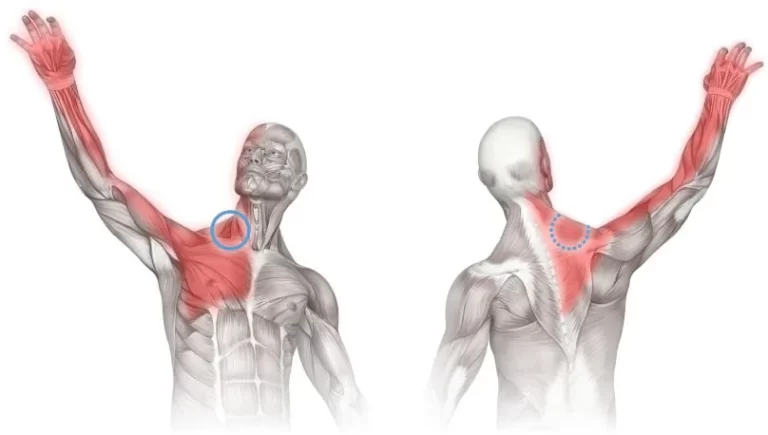
Causalgia is also called complex regional pain syndrome type II or CRPS II. It’s a neurological disease that can create long-lasting, intense pain. CRPS II occurs after an injury or trauma to a peripheral nerve. Peripheral nerves are located from your spine and brain to your extremities. The most typical site of CRPS II pain is in what’s known as the brachial plexus. This is the set of nerves that run from your neck to your arm.
Clinically Relevant Anatomy
CRPS can involve any portion of the body but happens most frequently in the extremities. The wrist is most often involved after distal radial fractures.
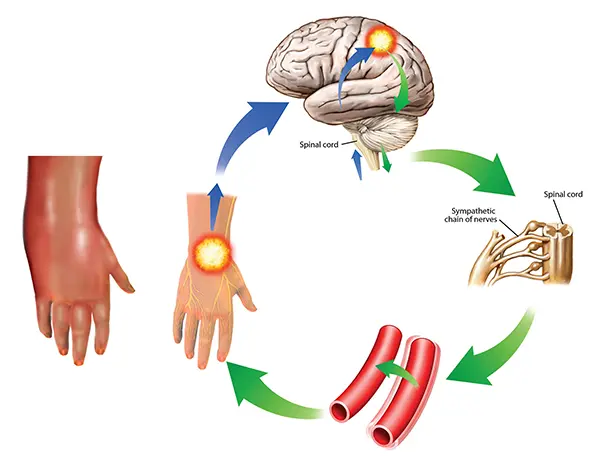
The central and peripheral nervous systems are linked via neural and chemical ways and can have direct command over the autonomic nervous system. It is for this cause that there can be differences in vasomotor and sudomotor reactions without any impairment in the peripheral nervous system. Ache, heat, and swelling are generally not found at the location of an injury and there may be no clear injury. Central sensitization is seen as the main reason for creating CRPS.
Symptoms of causalgia
Unlike CRPS I (previously called reflexive sympathetic dystrophy), CRPS II pain is normally localized to the region around the damaged nerve. If the damage happened to a nerve in your leg, for instance, then pain drops in your leg. Contrarily, with CRPS I, which doesn’t affect an obvious nerve injury, aches from a hurt finger can release throughout your body.
CRPS II can happen wherever there’s peripheral nerve damage. Peripheral nerves conduct from your spine to your extremities, which represents CRPS II is generally found in your:
arms
legs
hands
feet
However, of what peripheral nerve is damaged, symptoms of CRPS II tend to stay the same and involve:
- aching, burning, an excruciating ache that lasts six months or longer and appears unnecessary to the injury that obtained it on
- pins and needles feeling
- hypersensitivity around the site of damage, in which being touched or even wearing clothes can activate sensitivity
- swelling or immobility of the involved limb
- irregular sweating around the involved area
- skin color or temperature differences around the involved region, like skin that looks pale and senses cold and then red in color and warm and back again
Causes of causalgia
At the origin of CRPS II is peripheral nerve injury. That damage can result from a sprain, fracture, or surgery. In fact, according to one examination, 1.8 percent of about 400 elective foot and ankle surgery people created CRPS II after surgery. Other reasons for CRPS II contain:
- soft-tissue trauma, like a burn
- crushing injury, like slamming your finger into a car door
- Diabetes
- Infections like HIV and Lyme condition
- Tumors
- Bone marrow diseases
- Autoimmune disorders like arthritis and other conditions like kidney and liver conditions.
- Vitamin insufficiencies
- Medications or medical techniques like chemotherapy
- Amputation
Nevertheless, it’s still strange why some patients react so dramatically to these circumstances and others don’t.
Patients with CRPS (either I or II) likely have irregularities in the linings of their nerve fibers, assembling them hypersensitive to ache signals. These anomalies can also start an inflammatory reaction and cause differences in blood vessels. This is why so many patients with CRPS II can have swelling and skin bruises at the location of the damage.
Differential Diagnosis
Differential diagnosis contains the direct results of the following situations:
- Bony or soft tissue injury
- Peripheral neuropathy, nerve lesions
- Arthritis
- Infection
- Compartment syndrome
- Arterial insufficiency
- Raynauds Disease
- Lymphatic or venous obstruction
- Thoracic Outlet Syndrome (TOS)
- Gardner-Diamond Syndrome
- Erythromelalgia
- Self-harm or malingering
- Cellulitis
- Undiagnostic fracture
How causalgia is diagnosed
No one test can definitively diagnose CRPS II. Your doctor or physician will conduct a physical examination, document your medical record, and then request tests that may involve:
an X-ray to inspect for broken bones and loss of bone minerals
an MRI to examine soft tissues
thermography to examine skin temperature and blood flow between injured and noninjured limbs
Once other more typical diseases like fibromyalgia are eliminated, your doctor or physician can create a CRPS II diagnosis more confidently.
Infrared Thermography
Infrared thermography (IRT) is an adequate mechanism to find important asymmetry in temperature between both limbs by deciding if the involved side of the body indicates vasomotor dissimilarities in comparison to the further side. It is notified having a sensitivity of 93% and a particularity of 89%. This examination is difficult to get so it is not frequently used for analyzing CRPS.
Sweat Testing
Selecting if the patient sweats abnormally. Q-sweat is a satisfactory tool to estimate sweat production. The sweat specimens should be brought from both sides of the body at the exact time.
Radiographic Testing
Abnormalities in the bone structure of the involved side of the body can evolve visible with the help of X-rays. If the X-ray indicates no sign of osteoporosis, CRPS can be excluded if the person is a grown-up.
Three-Phase Bone Scan
A triple-phase bone scan is the most suitable approach to rule out Type I CPRS. With the help of technetium Tc 99m-labeled bisphosphonates, an accumulation in bone metabolism can be displayed. More increased uptake of the essence means raised bone metabolism and the body region could be involved. The triple-phase bone scan has the most suitable sensitivity, NPV, and PPV compared to MRI and plain film radiographs.
Bone Densitometry
An involved limb frequently displays less bone mineral density and a difference in the content of the bone mineral. During therapy of the Causalgia, the condition of the bone mineral will enhance. So this test can also be used to resolve if the person’s treatment is useful.
Magnetic Resonance Imaging (MRI)
MRIs are helpful to detect periarticular marrow edema, soft tissue bulge, and joint or junction effusions. And in a later phase atrophy and fibrosis of periarticular structures can be seen. But these manifestations are not solely signs of Causalgia.
Sympathetic Blocks
If the person displays vasomotor or sudomotor dysfunction and severe ache, stopping the sympathetic nerves verifies to be a useful technique to estimate if the sympathetic nervous system is causing the ache to stay. This procedure needs local anesthetic or ablation and is successful if at least 50% of the ache is eased.
Treatment options for causalgia
Parallel to CRPS Type 1, there are numerous treatment choices for CRPS Type 2. These treatments travel across various categories; involving drugs, physical therapy, and psychological treatment. Early therapy is the most useful and should begin as soon as a CRPS Type 2 diagnosis is made. Due to the variety of CRPS Type 2 treatment choices, the person’s treatment program may include several additional experts like neurologists and physical therapists. The other treatment choices employed for CRPS Type 2 therapy are given in more detail below:
Physical therapy
Normal, gentle movements can assist to enhance the person’s blood flow so they can recover functionality in the involved limb and have adequate tolerance for aches. Maintaining the limb in activity can assist to control muscle wastage and distortion of bones that may result from prolonged inactivity.
Psychotherapy
Living with a chronic disease such as CRPS Type 2 can bring its toll on the mental fitness of the involved person. This is generally because of the daunting learning that there is no remedy for the severe ache they experience daily. A further cause is a point that the person can no longer do most of the items they were capable of before the onset of CRPS Type 2 due to the ache they sense every time they move their limb. As a consequence, the person tends to feel sad and worried, thus the requirement for psychotherapy to manage these negative emotions.
Medication
A person may have to take several kinds of medications to effectively manage CRPS Type 2 and manage their ache and other symptoms. The different drugs frequently used for CRPS Type 2 treatment involve the following:
Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs like ibuprofen are used in the therapy of acute muscular and bone aches which is why they are helpful in the treatment of the chronic ache of CRPS Type 2. The benefit of these is that some kinds of NSAIDs are available over the counter so they are effortlessly available for patients who require to manage their aches.
Anticonvulsants
The primary role of anticonvulsants is for the therapy of epileptic seizures, but for CRPS Type 2 persons these medications are useful in the therapy of nerve aches.
Topical creams and patches
The ointments and patches suggest ache ease for some persons and can be brought over the counter at some pharmacies. Some instances of topical ointments and patches that can be used to decrease hypersensitivity are capsaicin ointment and lidocaine patches.
Corticosteroids
Corticosteroids have an anti-inflammatory impact and are more useful when used in the early phases of the medical situation.
Bisphosphonates
Bisphosphonates like Neridronate are highly useful in treating nerve aches. So distant, Neridronate is useful in the treatment of CRPS Type 1. There isn’t much information on its help in CRPS Type 2 treatment but so distant it’s the next best item to a cure for CRPS.
Botulinum toxin (botox) injections
Botulinum toxin injections work as sympathetic blocks to manage CRPS Type 2. They suggest a long analgesic impact hence providing long-lasting ache ease, although it’s not endless.
Opioids
For persons who feel a severe ache that can’t be treated with other medications, opioids like codeine and morphine can be more useful in treating aches.
N-methyl-D-aspartate (NMDA) receptor antagonists
This group of medicines is a class of anesthetics that inhibit the N-methyl-d-aspartate receptor which permits the transfer of electric signs between neurons in the brain and spinal column. An instance of N-methyl-D-aspartate (NMDA) receptor antagonists utilized for CRPS Type 2 medicines is ketamine.
If the above drugs don’t assist much in enhancing the patient’s symptoms, some alternative therapies are the next best choice. Some of these are solely used as the last alternative when all else has failed and they stay covered by discussion. These alternative treatments contain:
Sympathetic nerve-blocking
This therapy targets the sympathetic nervous system which is a sequence of nerves joining the spine to the body. As noted before, CRPS Type 2 involves the sympathetic nervous system and concerns the involuntary body functions that the system regulates, like blood flow, sweating, and digestion. The nerve-blocking injection used frequently has an anesthetic impact and blocks the transmission of ache signals, thus providing ache ease.
Spinal cord stimulation
Spinal cord stimulation affects the benefit of low-level electrical signals provided to the spinal cord or to exact nerves to block the transmission of ache signals to the brain. The electrical signals are distributed via an instrument that is planted in the body via a syringe that’s put in the back near the spinal cord. The instrument provides the person full control over their ache, permitting them to shift the electrical current on and off and even change the power of the signals consequently.
Repetitive Transcranial Magnetic Stimulation (rTMS)
This treatment targets brain stimulation and is used to manage sadness and fear. It functions hand-in-hand with CRPS Type 2 medical intervention. An electromagnetic coil is put close to the head, close to the location of the brain that controls mood. This coil gives magnetic pulses to the targeted location hence presenting electrical currents that produce brain cells and decrease depression.
Occasionally other treatments are required to provide maximum convenience for the person and enhance the efficacy of the therapies. Complementary treatments that can be done in extra to all the above treatments contain:
Acupuncture
Relaxation techniques
Chiropractic therapy
Heat and cold therapy
Experimental treatments available for CRPS Type 2 treatment that can be tried contain:
Intravenous immunoglobulin
Amputation
Physiotherapy treatment
Exercise can assist to:
- Decreased pain
- increase mobility
- Control depression
- Help in the management of recurrent pain episodes
- Reduction in fatigue
- Reduce social isolation.
Physical therapy intervention could contain any of the following:
Transcutaneous electrical nerve stimulation (TENS)
Aquatic therapy permits movements to be conducted with reduced weight bearing on the lower extremities.
Mirror therapy
Desensitization
Gradual weight bearing
Gentle Stretching exercise
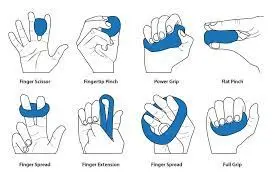
Fine motor control
Acute Phase
Immobilization and contralateral treatment. Intensive dynamic treatment in the acute phase can lead to damage. The focus should be on teaching to expedite healing. Comfort and familiarize. This may or may not involve any detailed concern to CRPS. Observe and normalize earnings.
- The goal is to get the person on the side about why functional motion is now vital, why breaking immobilization is required, and provide the idea that the injury has recovered are fully oriented.
- Avoid overuse of precise activities or manual procedures that may stimulate an increase in ache reaction and guard. Perform more on gross active motion patterns.
- Wean off any slings or enable only smart use.
- Normalizing motion and restoring contact with the hand in practical use are important early on.
Normalize body image
Instruct plans to correct body perception disorder, including looking, touching, and thinking about the involved body region
Mirror therapy
Mirror box therapy began at an early stage and can assist to decrease body image differences. Start by only looking into the mirror until no ache is felt before moving to any active motions. Per progression is ache dependent and can differ in time brought to improvement.
Cognitive visualization to normalize altered dimensions and shape perception of an involved body region
There is some proof to recommend that mirror therapy has the result:
- Decreasing ache intensity and enhancing role in post-stroke CRPS
- A marked progress in ache
- Enhancing function (low-quality proof, yet)
- Graded motor imagery/education is useful. Yet, additional tests are needed GMI plus medical control is more useful than medical management plus physiotherapy GMI may decrease pain and enhance function. Other treatments contain cognitive-behavioral therapy, relaxation, deep breathing activities, and biofeedback.

Splinting
Release of over-immobilizing the hand in early phases of the disease is important to control dependency on irregular motion ways and to correct the idea that the hand is not /no longer damaged and requires it to be treated naturally. Relaxing splinting may still be needed to assist to control ache levels in the early phases but brilliant use is important.
Splinting may be used to set whilst resting to control contracture or allow ease, to enhance a precise range of movement, or to assist with functional benefit.
Later phases of the disease may need night splinting to fix or control contracture. Again weigh up the positive and negative of per method

Compression therapy
lycra gloves may be manipulated to decrease swelling or to supply sensory stimulation. This may be helpful at any phase of rehabilitation. The use of compression gloves must be counteracted by the psychological effect a glove may have on the person.

Range of motion controls contracture and normalizes motion patterns.
Functional motion techniques to enhance motor power and awareness of involved limb part
Early prevention is important as differences can happen very fast. Educate the person on how to self-assess progress and decline.
Control of CRPS-related dystonia is vital in the early and later phases
Strength, dexterity, and functional use
Functional power should be restored using precise functional activity. Create tasks work particularly wherever feasible even in an altered format, Principles of stress loading can be presented to enhance proprioceptive feedback
Pain
This is hard to manage. Medicine should be begun within a few weeks of selected CRPS,
This does not take the primary result. Persons will probably be sent to a pain clinic for assessment. The drug should be resumed for a time after the resolution of symptoms to control reoccurrence.
Physiotherapy instantly for aches may contain acupuncture and TENS glove.

Desensitise hyperaesthesia areas
Self-administered tactile and thermal desensitization to normalize touch perception. Silicone patches should solely be used where very precise scar hypersensitivity is seen not in all-around hyperaesthesia.
Dissent allodynia re-education may be used to decrease the anxiety of physical connection with others in social environments

Lymphatic drainage
Lymphatic drainage can be used to promote the deterioration of edema. Tender sites are suggested to be managed in the following order: more intense before less intense, more proximal and medial before more distally and laterally situated points and the location of the greatest collection of tender places is treated first. When tender places are found in a row, the center is treated first.
Neuromodulation or Invasive Stimulation Techniques
Neuromodulation includes peripheral nerve stimulation with planted electrodes, deep brain stimulation, epidural spinal cord stimulation, and electrotherapy. Electrotherapy contains spinal cord stimulation (SCS), transcutaneous electric nerve stimulation TENS, and non-invasive brain stimulation (redundant transcranial magnetic stimulus). These methods assist to decrease pain, although other tests are needed
Chronic Phase
Later management
Focus may require to go to more formal pacing and planning purposes, sleep hygiene, and leisure talents, Coping talents may require to be handled.
At later rehabilitation phases it may be required to add precise activities to address precise joint or junction or tendon stiffness and prevent contracture product.
Pushing into ache may evolve as required to make progress.
Referral to ache hospitals is very good to provide optimal medical administration
Other Treatments
- Whirlpool bath/ contrast baths
- Vocational and recreational rehabilitation
- Psychological therapies: operant conditioning (OC), cognitive-behavioral therapy (CBT), counseling, pain education, and relaxation methods
- Acupuncture, electroacupuncture
- Tactile sensory discrimination training
- Weight-bearing
- Ultrasound therapy
- Kinesio taping
Surgery
Medical treatment is sometimes inadequate in the treatment of CRPS Type 2. At that point, surgery may be the next best choice and is usually booked for the most intense circumstances. The surgery form of cutting the involved nerves to control aching impulses from getting the brain. Some of the surgical techniques used in CRPS Type 2 are explained briefly down below:
Spinal cord stimulators
Spinal cord stimulation masks ache signs before they are transferred to the brain via the use of a small, pacemaker-like machine that provides electrical vibrations to the spinal cord. This approach has been noticed to be useful in the management of CRPS by enhancing ache and quality of life. The quantity of ache ease with spinal cord stimulation instruments differs per person.
Sympathectomy
Surgical, chemical, or radiofrequency sympathectomy is utilized to interrupt or block the involved tincture of the sympathetic nervous system. Sympathectomy for CRPS therapy can be used as a last alternative in persons with upcoming edema, tissue loss, or recurrent infection. The approach has been noticed to obtain lasting ease to over 80% of persons and ease to 90%. In complement to normal surgical risks like bleeding and infection, sympathectomy has other exact risks like adverse differences in how nerves role.
Amputation
If the above-mentioned therapies have failed, amputation is occasionally believed the next best choice. On average, 50% of persons who opt for this have been noted to have a solution for their ache while the further half form phantom limb aches and/or aches at the area of the amputation. It is suggested that amputation be left as a last alternative, although it should be mentioned that late amputation may not work as well as desired.
Conclusion
While CRPS Type 2 is relatively rare, the few someones diagnosed with this state of medical situation can try the above-mentioned therapies to control their disease. As with most conditions, the sooner therapy starts, the better the opportunities for usefulness. There aren’t a lot of details available with regards to CRPS Type 2 and its therapy on understanding how rare it is. The best approach is to assess the therapies to see what’s performing and what’s not and try any of the available choices.
What is the CRPS Type 2 Prognosis?
Different professionals may be required for adequate treatment of CRPS Type 2 like specialists in orthopedics, ache management, and even psychiatry. The significance of CRPS Type 2 treatments is much enhanced the sooner the condition is analyzed and treated. Early diagnosis and therapy give the person adequate options for a positive result.
FAQ
In which nerve injury does causalgia usually occur?
Causalgia is a periodic ache syndrome linked to partial peripheral nerve damage. The peripheral nervous system contains nerves that stretch from the central nervous system of the brain and spinal cord to help limbs and organs. Extreme issues are known as major causalgia.
What is the causalgia of the lower limb?
Causalgia: Further Name for Complex Regional Pain Syndrome II. Persons who undergo chronic, extreme burning aches in a limb due to damage to a peripheral nerve may have once been suggested that they sorrow from causalgia. Today, the situation is more frequently directed to as Type 2 Complex Regional Pain Syndrome (CRPS II).
What type of pain is causalgia?
Causalgia is a periodic pain syndrome associated with partial peripheral nerve hurts. The peripheral nervous system contains nerves that lengthen from the central nervous system of the brain and spinal cord to help limbs and organs. Extreme points are known as major causalgia.
What is the difference between causalgia and CRPS?
In patients of Type 1 CRPS (CRPS I), ache forms even though there has been no immediate harm to the nerves in the extremity. But causalgia is induced by identifiable damage or trauma to the nerves in the involved extremity. Causalgia involves a small minority of persons(1 out of 100,000) who are analyzed with CRPS.
What are the two types of complex regional pain syndrome?
CRPS is separated into two groups: Type 1: Also known as sympathetic dystrophy, which grows without known nerve injury. Type 2: Also known as causalgia, which is the effect of precise nerve injury.




2 Comments