Diabetes Mellitus
What is Diabetes Mellitus?
Diabetes mellitus, commonly referred to as diabetes, is a chronic metabolic disorder characterized by elevated blood glucose levels (hyperglycemia) resulting from defects in insulin secretion, insulin action, or both.
Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar by facilitating the uptake of glucose into cells for energy.
Defination
A metabolic condition characterized by abnormally high blood glucose levels is diabetes mellitus (DM). Type 1, type 2, gestational diabetes, infant diabetes, maturity-onset diabetes of the young (MODY), and secondary causes resulting from endocrinopathies, steroid use, etc. are among the various types of diabetes mellitus.
Type 1 diabetes mellitus (T1DM) and Type 2 diabetes mellitus (T2DM) are the two primary subtypes of diabetes mellitus (DM). Both types of diabetes are primarily caused by incorrect insulin production and/or action, respectively. While Type 2 diabetes. is expected to affect middle-aged and older adults who have persistent high blood sugar as a result of poor dietary and lifestyle choices, Type 1 diabetes appears to occur in children or teenagers
Causes of Diabetes Mellitus
The two main groups of endocrine cells found in the pancreatic islets of Langerhans are alpha cells, which release glucagon, and beta cells, which produce insulin. The environment of glucose continually affects the amount of hormones produced by beta and alpha cells.
When glucagon and insulin are out of balance, glucose levels become unnecessarily unbalanced. When diabetes mellitus (DM) occurs, insulin either doesn’t function or acts weakly (insulin resistance), raising blood sugar levels.
The most common feature of type 1 diabetes is the autoimmune-mediated loss of beta cells in the pancreas. As a result, beta cells are destroyed, which causes either very little or no insulin.
Type 2 diabetes. has a more insidious beginning in which a functional insulin deficit results from an imbalance between insulin levels and insulin sensitivity. Although it is multifaceted, age and fat are the two main causes of insulin resistance.
One important risk factor for both types is family genetics. Several loci that give risk for diabetic mellitus have been discovered as the human genome is investigated. Polymorphisms involving the major histocompatibility complex (MHC) and human leukocyte antigen (HLA) have been shown to impact the risk for type 1 diabetes.
Genetics and lifestyle play a more complex role in type 2 diabetes. Compared to Type 1 diabetes, Type 2 diabetes. appears to have a stronger genetic profile, according to numerous studies. Most individuals suffering from the condition have at least one parent who has type 2 diabetes.
When one twin in a pair is affected by Type 2 diabetes, there is a 90% chance that the other twin will experience the disease at some point in their lives. At this point, about 50 polymorphisms have been identified as either protective or contributing to the risk of type 2 diabetes.
The proteins that these genes encode have been linked in several pathways that contribute to diabetes mellitus (DM), including insulin production, secretion, and development; amyloid deposition in beta cells; insulin resistance; and defective control of gluconeogenesis.
Genetic loci for the transcription factor 7-like 2 gene (TCF7L2), which raises the risk for type 2 diabetes, have been identified using a genome-wide association study (GWAS). Other loci that affect the development of type 2 diabetes include WFS1, NOTCH2, JAZF1, and KCNQ1.
Diabetes caused by pregnancy is primarily known as gestational diabetes. Although the exact cause of its development is still unknown, some people suspect that HLA antigens—more especially, HLA DR2, 3, and 4 may be involved.
Gestational diabetes is also thought to be related to excessive proinsulin, and some research shows that proinsulin may cause beta-cell stress. Some people think that high levels of hormones such as estrogen, progesterone, cortisol, prolactin, and human placental lactogen may have an impact on peripheral insulin sensitivity and beta-cell activity.
The glucogenic action of endogenous hormones that are excessively released in several endocrinopathies, such as acromegaly, Cushing syndrome, glucagonoma, hyperthyroidism, hyperaldosteronism, and somatostatinomas, has been linked to glucose intolerance and diabetes mellitus. Because of excessive iron deposition in the pancreas and beta cell death, conditions such as idiopathic hemochromatosis are linked to diabetes mellitus.
Epidemiology
Diabetes mellitus affects 1 in 11 persons worldwide, with 90% having T2DM. T1DM begins to rise gradually from newborns and peaks between the ages of 4 and 6 and then again between 10 and 14 years. About 45 percent of the children arrive before they reach 10 years old. In those under 20, the prevalence is roughly 2.3 per 1000. Although the majority of autoimmune disorders are more common in women, there does not appear to be a gender difference in the occurrence of T1DM in children.
Though overweight in teenagers has led to an increase in Type 2 diabetes in younger populations, type 2 diabetes often appears later in life.
According to estimates from the International Diabetes Federation, 1 in 11 individuals worldwide aged 20 to 79 had diabetes in 2015.
Pathophysiology
Hyperglycemia is a possibility in a patient with diabetes mellitus. Since multiple causes can often give rise to the condition, the pathophysiology of diabetes mellitus may be ambiguous. Even by itself, high blood sugar levels can damage the release of insulin and pancreatic beta-cell function. As a result, high blood sugar levels create a vicious loop that impairs metabolic function.
In this setting, blood glucose levels exceeding 180 mg/dL are frequently regarded as hyperglycemic; however, due to the multiplicity of mechanisms involved, a precise cutoff threshold is unknown. Higher blood glucose levels cause the nephron’s glucose transporters to become saturated, which causes osmotic diuresis in patients. Serum glucose levels exceeding 250 mg/dL are likely to cause symptoms of polyuria and polydipsia, while the effect differs.
Excess fatty acids and proinflammatory cytokines cause insulin resistance by impairing glucose transport and speeding up the breakdown of fat. The body reacts to insufficient insulin responsiveness or synthesis by mistakenly raising glucagon levels, which contributes to high blood sugar levels. Although insulin resistance is a part of type 2 diabetes, the disease’s full effect occurs when the patient’s insulin production is insufficient to offset their insulin resistance.
Proteins and lipids are glycated nonenzymatically by chronically elevated glucose levels. The glycation hemoglobin (HbA1c) test can be used to detect how much of this is present. Damage to small blood vessels in the kidney, retina, and peripheral nerves is caused by glucose. Increased glucose levels speed up the procedure.
Symptoms of Diabetes Mellitus
Many people with diabetes can have no symptoms, particularly in the early stages of the condition. However, if blood glucose levels are considerably raised, the symptoms of the two types of diabetes may be extremely similar.
Symptoms of higher blood sugar levels include
- An increase in hunger
- Urination becomes more frequent
- Excessive thirst.
When blood glucose levels go above 160 to 180 mg/dL (8.9 to 10.0 mmol/L), glucose leaks into the urine, when the level of glucose in the urine rises even higher, the kidneys produce more water to help reduce the elevated levels of glucose. People with diabetes urinate in large quantities regularly due to a rise in urine production by the kidneys.
Type 1 diabetes
The symptoms of type 1 diabetes frequently appear suddenly at first. The body may soon develop a complication known as diabetic ketoacidosis, which is a dangerous disease in which the body creates excess acid.
Apart from the customary symptoms of diabetes mellitus, which are increased thirst and urine production, the earliest symptoms of diabetic ketoacidosis also include tiredness, nausea, vomiting, and, in children especially, stomach pain.
As the body tries to balance the acidity of the blood, breathing begins to become deep and quick, and the breath smells like fruity nail polish remover. Diabetic ketoacidosis can occasionally develop extremely fast to a coma and death if left untreated.
Type 2 diabetes
Before being identified, people with type 2 diabetes might not have any symptoms for years. The symptoms could be mild. Initially moderate, increased thirst and urination get worse over weeks or months. People eventually experience great tiredness, possibly blurred eyesight, and possibly dehydration.
Even when type 2 diabetes is left untreated for an extended period, ketoacidosis typically does not occur because persons with the disease make some insulin. Extremely high blood glucose levels—even beyond 1,000 mg/dL [55.5 mmol/L]—occur rarely. Such high levels are frequently a result of an additional source of stress like an infection event or drug usage.
Diagnosis
History and Physical
During the patient’s history, questions about family history, autoimmune diseases, and insulin resistance are important for diagnosing diabetes. It frequently appears asymptomatically, but when symptoms do appear, patients typically present with polyuria, polydipsia, and weight loss.
A physical examination of someone with high blood sugar levels may reveal poor skin turgor (due to dehydration) and a characteristic fruity smell in their breath (in ketosis patients).
Clinicians may observe Kussmaul’s respirations, tiredness, nausea, and vomiting when treating diabetic ketoacidosis (DKA). A funduscopy examination in a diabetic patient may reveal hemorrhages or exudates on the macula. In acute diabetic retinopathy, retinal venules may be blocked.
People with Type 2 diabetes are usually overweight or obese and show symptoms related to insulin resistance, such as acanthosis nigricans, which are hyperpigmented, velvety patches on the skin of the neck, axillary, or inguinal folds.
Patients with a lengthy history of hyperglycemia may experience blurred vision, frequent yeast infections, numbness, or nerve pain. During each appointment, clinicians must ask the patient if they have seen any recent skin changes on their foot. The diabetic foot exam, which involves the monofilament test, should be part of the standard physical exam.
Evaluation
A characteristic history along with increased serum glucose levels (fasting glucose > 126 mg/dL, random glucose > 200 mg/dL, or hemoglobin A1C > 6.5%), with or without antibodies to insulin and glutamic acid decarboxylase (GAD), is typically used to diagnose type 1 diabetes
Early detection of type 2 diabetes can be helped by HbA1c testing and fasting glucose levels. A glucose tolerance test can be used to assess serum response to an oral glucose tolerance test (OGTT) as well as fasting glucose levels if the results are unclear. A glucose level of 140 to 200 mg/dL is seen two hours after an oral glucose tolerance test (post-OGTT), indicating prediabetes, which frequently occurs before type 2 diabetes.
All pregnant patients are screened for gestational diabetes between 24 and 28 weeks of pregnancy, using a 1-hour fasting glucose challenge test. If blood glucose levels reach 140mg/dL, individuals will have a 3-hour fasting glucose challenge test to confirm their diagnosis. A positive 3-hour OGTT test occurs when there is at least one abnormal value higher than or equal to 180, 155, or 140 mg/dL for fasting one-hour, two-hour, and 3-hour plasma glucose concentration, respectively.
Several lab tests are useful in managing chronic diabetes Mellitus. Home glucose testing can reveal trends in high- and low blood sugar The test for HbA1c measures the degree of glycation caused by high blood sugar levels over three months (red blood cell life). Urine albumin testing can detect early signs of diabetic nephropathy.
Because diabetic patients are also predisposed to cardiovascular disease, serum lipid monitoring is recommended at the time of diagnosis. Similarly, because hypothyroidism is more common, some propose monitoring thyroid health by collecting a blood test of thyroid-stimulating hormone once a year.
Treatment of Diabetes Mellitus
Diabetes has a complicated physiology and treatment plan that require numerous interventions for effective disease control. Patient involvement and diabetic education are necessary for management. Patients who can control their diet (restrictions on carbohydrates and total calories), exercise frequently (above 150 minutes per week), and self-monitor their blood sugar levels will fare better.
To avoid unexpected effects, treatment must frequently last a lifetime. Maintaining glucose levels between 90 to 130 mg/dL and a HbA1c of less than 7% is the ideal range. While controlling blood sugar levels is essential, overly strict regulation can result in hypoglycemia, which can have dangerous or even life-threatening outcomes.
The basic principle of treatment for type 1 diabetes is insulin administration through daily injections or an insulin pump, as the disease is largely caused by an insufficient supply of insulin. In the early stages of type 2 diabetes, diet and exercise may be sufficient therapies. Other treatments can focus on improving insulin sensitivity or raising the pancreas’ production of insulin.
Biguanides (metformin), sulfonylureas, meglitinides, thiazolidinediones, alpha-glucosidase inhibitors, glucagonlike-peptide-1 agonist, dipeptidyl peptidase IV inhibitors (DPP-4), selective amylinomimetics, and sodium-glucose transporter-2 (SGLT-2) inhibitors are some of the specific drug subclasses. The first drug used to treat diabetes is metformin, which lowers basal and postprandial plasma glucose.
Patients with type 2 diabetes may also require insulin treatment, particularly if their glucose control is inadequate and their condition has progressed. Bariatric surgery is a possible way to correct glucose levels in patients who are severely overweight. It is advised for people with serious comorbidities and those who have not responded to previous therapies. Liraglutide and semaglutide, GLP-1 agonists, have been associated with better cardiovascular outcomes. The SGLT-2 inhibitors canagliflozin and empagliflozin have also been shown to enhance cardiovascular outcomes, possibly providing renoprotection, and delaying the onset of heart failure.
Since microvascular problems are a feared result of diabetes, routine tests are important. To check for diabetic retinopathy, trained medical professionals should do routine diabetic retinal exams. Patients at risk for amputation with neuropathy can be identified by neurologic examination along with monofilament testing.
Physicians may also advise patients to examine their feet every day to spot any lesions that neuropathy may have missed. To treat neuropathic pain in diabetics, low-dose tricyclic antidepressants, duloxetine, anticonvulsants, topical capsaicin, and painkillers could be required.
Together with the estimated kidney function (GFR a urine microalbumin test can detect early renal effects of diabetes mellitus if there is albuminuria larger than 30 mg/g of creatinine. Angiotensin receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors are the preferred medications to slow the transition from microalbuminuria to macroalbuminuria in patients with Type 1 or Type 2 diabetes mellitus because of their antiproteinuric effects.
Differential Diagnosis
Diabetes Mellitus can also be brought on by Type 2 diabetes, any disease that harms the pancreas, and Type 1 diabetes. The exocrine pancreas can develop several diseases, such as:
- pancreas cancer
- cystic fibrosis
- Prolonged pancreatitis
- hereditary hemochromatosis
The following hormonal disorders have been linked to decreased insulin release:
- Acromegaly
- Cushing syndrome
- Pheochromocytoma
The differential diagnosis of conventional diabetes also includes drug-induced insulin resistance.
Among these medicines are:
- Glucocorticoids
- phenytoin
- estrogen
In the differential diagnosis of diabetes mellitus, other illnesses include:
- Diabetes during pregnancy
- Thyroid conditions
Prognosis
The level of glucose control has a major impact on the prognosis of diabetes mellitus. The likelihood of problems from diabetes mellitus is greatly increased by chronic hyperglycemia.
According to the United Kingdom Prospective Diabetes Study and the Diabetes Control and Problems Trial, those with Type 1 diabetes and Type 2 diabetes, had higher rates of microvascular problems associated with ongoing hyperglycemia.
Patients with a good prognosis who can return to normal glucose levels during the transition from pre-diabetes to frank diabetes had the potential to slow the course of the disease.
Complications related to Diabetic Mellitus
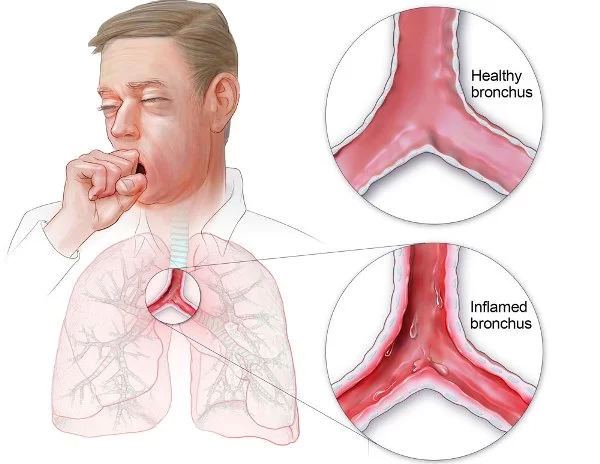
The frequency of long-term problems is rising as a result of diabetes mellitus patients’ longer survival times. Vascular problems, which can affect capillaries, tiny or major arteries, are the most frequent type of complications. Atherosclerosis, also known as atherosclerotic vascular disease, is typically the first symptom of large-vessel disease.
Although it may start earlier and progress more quickly in diabetic patients than in non-diabetic people, atherosclerosis does not differ in diabetic patients from non-diabetic patients. It affects the major arteries that give blood to the legs (the iliac and femoral arteries), the cerebral arteries, and the coronary arteries.
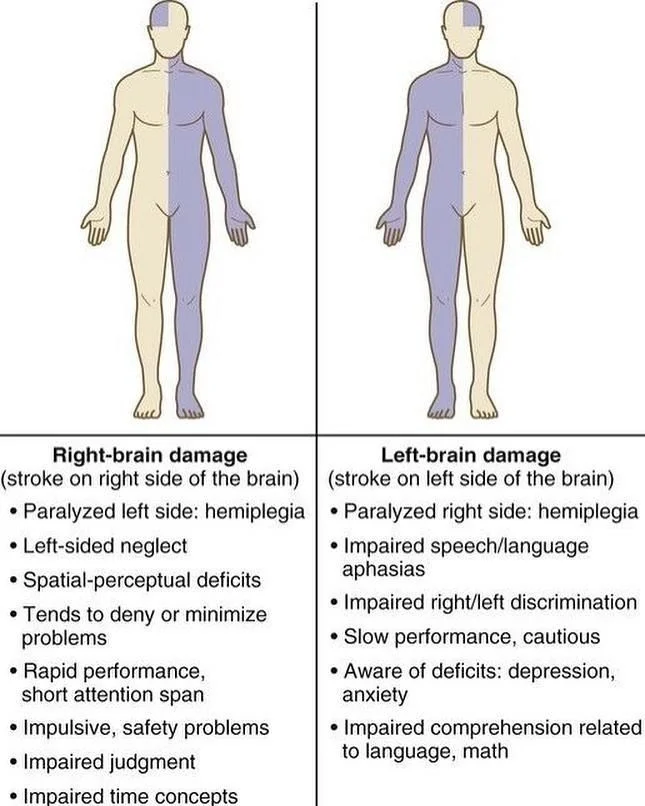
Therefore, people with diabetes are more likely to experience stroke, nonfatal and fatal myocardial infarction (heart attack), ulcers, and gangrene of the feet, which frequently require amputation.
Thickening of the walls of small arteries and capillaries causes small-artery disease (microangiopathy), which makes them initially permeable (leaky) to fluids and thereafter more susceptible to blockage (thrombosis or embolism).
Diabetes is the most frequent cause of end-stage renal disease and blindness because of these changes, which are largely seen in the retina (diabetic retinopathy) and kidneys (diabetic nephropathy). Hypertension and hyperlipidemia (high serum lipid levels), which are common among diabetic individuals, worsen vascular problems.
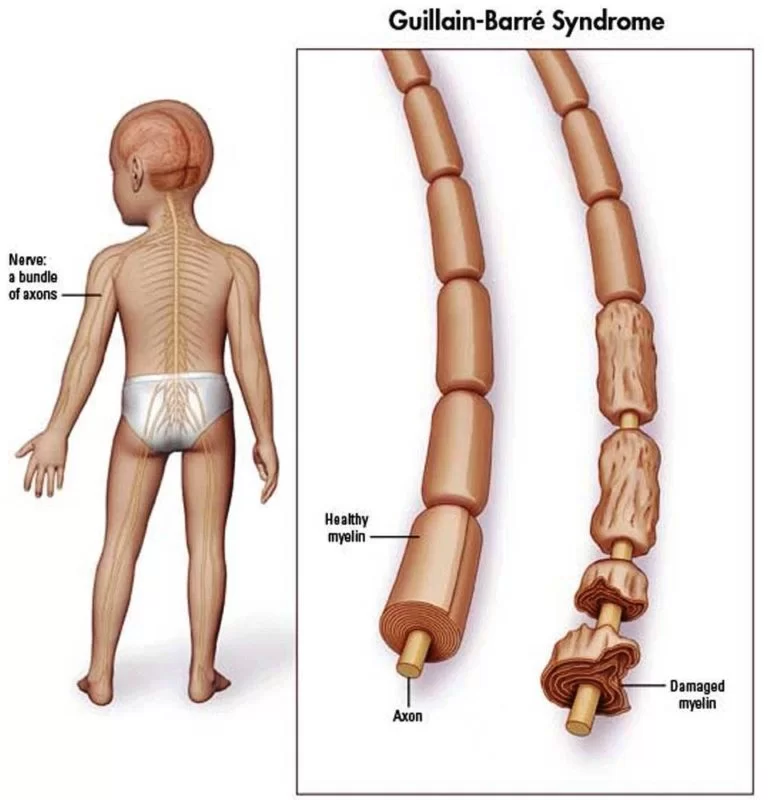
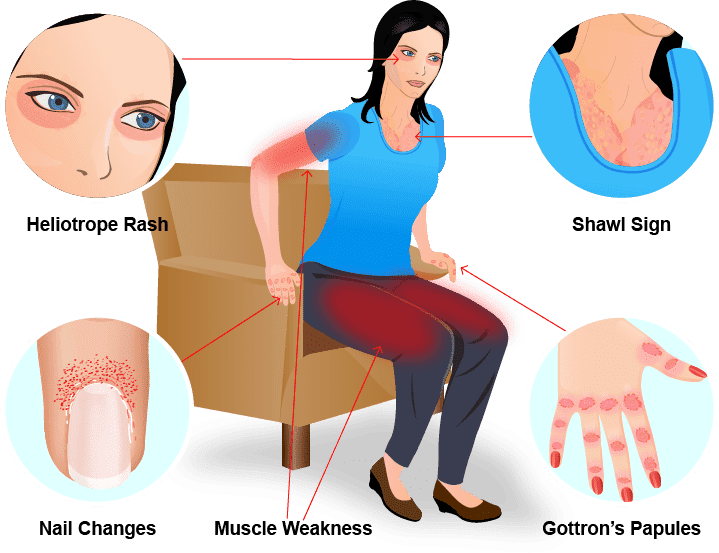
Diabetic neuropathy and cataract development are two other nonvascular complications associated with diabetes. Symmetric polyneuropathy is the most common kind of neuropathy. This results in aberrant sensation (tingling or numbness) or lack of sensation, as well as loss of vibratory and positional senses.
Thickening of the walls of small arteries and capillaries causes small-artery disease (microangiopathy), which makes them initially permeable (leaky) to fluids and thereafter more susceptible to blockage (thrombosis or embolism). Diabetes is the most frequent cause of end-stage renal disease and blindness because of these changes, which are largely seen in the retina (diabetic retinopathy) and kidneys (diabetic nephropathy). Hypertension and hyperlipidemia (high serum lipid levels), which are common among diabetic individuals, worsen vascular problems.
Diabetic neuropathy and cataract development are two other nonvascular complications associated with diabetes. Symmetric polyneuropathy is the most common kind of neuropathy. This results in abnormal sensation (sensation of tingling or numbness) or loss of sensation, as well as weakening of the hands, foot, and lower legs muscles as well as loss of positional and vibratory awareness.
Some people suffer from single-nerve neuropathy, which is characterized by loss of function in one or both eyes, impairing vision, or in the forearm muscles, resulting in wrist drop. Additionally, they can have autonomic neuropathy, which can cause erectile dysfunction, gastric retention, postural hypotension (fainting when sitting or standing), and urine bladder malfunction. These problems could be brought on by diseases of the tiny blood capillaries in these tissues, glycosylation of the neurological or ocular tissues, or an accumulation of osmotically active glucose metabolites in these tissues.
Controlling hyperglycemia can delay or stop the onset or progression of the small-vessel complications associated with diabetes, including diabetic retinopathy, diabetic nephropathy, and diabetic neuropathy.
It is unclear if managing hyperglycemia has a comparable impact on managing large-vessel problems. By managing high blood pressure, or hypertension, the start and progression of the vascular problems associated with diabetes can be postponed. Many antihypertensive medications aim to precisely block the effects of the peptide angiotensin II, which increases blood vessel constriction to raise blood pressure.
Inhibitors of the angiotensin-converting enzyme (ACE inhibitors): these medications turn inactive angiotensin I into active angiotensin II; inhibitors of the angiotensin receptor: these medications stop angiotensin II from causing blood vessels to constrict. In people with diabetes, quitting smoking and reducing serum lipid concentrations can also assist in slowing the progression of vascular disease.
Patient Education
It is important for medical professionals to actively educate patients with diabetes mellitus. Patients who believe that lifestyle modifications should only be made temporarily may be misinformed; to effectively control their diabetes, lifelong lifestyle modifications may be required. Individualized education is more beneficial than group education for individuals with poorly managed diabetes mellitus, according to randomized, controlled research. Healthcare workers who are not physicians, such as nurses and pharmacists, frequently have more time for specialized education and have received substantial training in diabetes education.
Pearls and Other Issues
The development of type 2 diabetes may be strongly affected by amino acid metabolism. According to studies, people with hyperglycemia had four times as much isoleucine, phenylalanine, and tyrosine. These amino acids were shown to be raised to 12 years before the disease’s beginning by the researchers.
The function of these metabolites in the development, screening, and management of metabolic syndrome (MetS), a cardiometabolic cluster that predisposes patients to type 2 diabetes and cardiovascular disease, has been further clarified by recent investigations.
Research has indicated that choline, L-carnitine, and trimethylamine-N-oxide are linked to inflammatory pathways and raise the possibility of metabolic dysfunction in individuals who are at risk of developing MetS, meaning they fit the criteria for the condition but do not have cardiovascular disease or type 2 diabetes. Particularly low lysine levels have been linked to higher blood glucose and inflammation.
Hence, consuming more lysine in the diet may enhance its anti-inflammatory properties. Phosphodiethylcholine 34:2, PC (34:2), GABA, and d-pyroglutamic acid (PGA) were found to be significantly elevated in developing MetS and to have a favorable correlation with a few inflammatory markers in a recent study. These results support the hypothesis that metabolites play a part in the pro-inflammatory state linked to diabetes and the early development of type 2 diabetes.
Results of Healthcare Teams
Patients with diabetes are frequently first diagnosed with the disease by primary care medical professionals. Because diabetes mellitus is a complicated disease, managing it calls for an interdisciplinary team approach.
Monitoring the effectiveness of therapies and making sure that patients are properly followed up on can be greatly helped by nursing professionals and physician assistants. To help patients learn about proper lifestyle modifications and at-home glucose management, nutritionists and diabetes educators can also offer consultations.
The healthcare team may also include nephrologists, podiatrists, neurologists, and ophthalmologists to make sure that patients with DM receive the necessary tests to avoid life-threatening microvascular complications. When patients do not respond to basic therapy, endocrinologists may be consulted.
Naturally, pharmacists are essential in assessing suitable drug delivery and preventing polypharmacy in diabetic patients, who frequently take several medications for the underlying condition and its side effects. They can guarantee appropriate dosage and suggest the most effective regimens to attain glycemic control, as well as inform the patient about the drugs and the course of the disease.
Individualized education produced better glucose control outcomes for patients with suboptimally managed diabetes than group education, according to Sperl-Hillen et al. Better behavioral and psychological results were also experienced by these patients.
FAQs
What is called diabetes mellitus
A collection of diseases commonly referred to as diabetes mellitus affects the body’s ability to use glucose or blood sugar. The cells that form the muscles and tissues depend on glucose as a major energy source. It also provides the majority of the brain’s energy.
What causes diabetes mellitus?
The mechanism that protects the body against infection, the immune system, targets and kills the pancreatic beta cells that produce insulin, which results in type 1 diabetes. Researchers believe that viruses and other environmental variables that may cause the disease are the primary causes of type 1 diabetes.
What are diabetes mellitus type 1 and 2?
Type 1 and type 2 diabetes Mellitus have different causes: Because the body’s immune system targets the insulin-producing islet cells in the pancreas, diabetes type 1 results in the pancreas producing no insulin. When you have type 2 diabetes, your body develops resistance to insulin and your pancreas produces less insulin than it once did.
What is the prevention of diabetes mellitus?
People should aim to achieve and maintain a healthy body weight to help prevent type 2 diabetes and its complications. Maintain a daily physical activity level by engaging in at least 30 minutes of moderate exercise. Have a balanced diet and stay away from sugar and saturated fat.
What are the main management of diabetes mellitus?
This involves monitoring blood sugar levels, controlling diet and exercise, managing weight and stress, keeping an eye on oral drugs, and, if necessary, using insulin pumps or injections.
Which hormone causes diabetes mellitus?
Diabetes mellitus is a disorder in which the body either produces insufficient amounts of the hormone insulin or uses the insulin it produces improperly, leading to high blood sugar levels.
References
- Sapra, A. (2023, June 21). Diabetes. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK551501/
- Brutsaert, E. F. (2023, December 6). Diabetes Mellitus (DM). MSD Manual Consumer Version. https://www.msdmanuals.com/en-in/home/hormonal-and-metabolic-disorders/diabetes-mellitus-dm-and-disorders-of-blood-sugar-metabolism/diabetes-mellitus-dm
- Diabetes mellitus | Definition, Types, Symptoms, & Treatment. (2024, January 18). Encyclopedia Britannica. https://www.britannica.com/science/diabetes-mellitus




2 Comments