Dermatomyositis
What is Dermatomyositis?
Dermatomyositis is a rare condition that generates muscle weakness and rashes on your skin. It’s a condition of myopathy. It can also induce extreme symptoms that involve your capability to breathe and swallow.
Dermatomyositis is a condition of polymyositis that involves your skin in addition to your muscles.
See your provider or doctor right away if you feel any symptoms of dermatomyositis. Some patients bring months to develop, but dermatomyositis can grow fast. The sooner you start therapy, the more probable it is you can avoid having extreme complications.
In rare circumstances, dermatomyositis can be fatal, particularly in the first year after symptoms begin. It can also improve your risk of developing specific types of cancer.
Types
Adult dermatomyositis generally happens in a patient aged 40 – 50 years. There may even be a more regular relationship between dermatomyositis and underlying cancers.
Juvenile dermatomyositis is a state of dermatomyositis that involves kids. Doctors or physicians generally diagnose it in kids aged 5 – 15 years, and it is more familiar among white kids.
The symptoms associated with youth dermatomyositis are the exact as those of grown-up dermatomyositis, but the beginning is more sudden, and the disease frequently presents with skin changes before muscle weakness.
Overall blood vessel inflammation, known as vasculitis, and calcinosis large calcium deposits under the skin happen more often in kids than in grown-ups. Those involved may also create a tiptoe gait secondary to ankle immobility.
Yet, unlike in the grown-up form, kids with the disease are not at risk of cancer.
Dermatomyositis sine myositis, which doctors even call amyopathic dermatomyositis, is another state of dermatomyositis. It presents with specific skin lesions of dermatomyositis but without the associated muscle irregularities.
What are the symptoms of dermatomyositis?
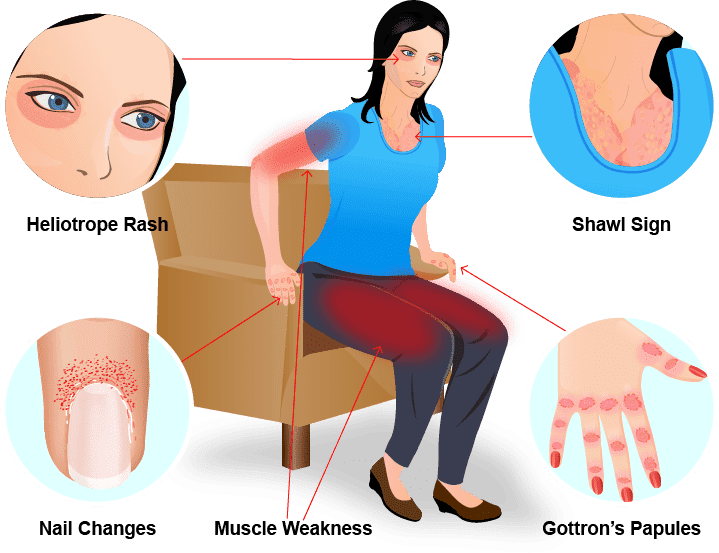
The most familiar symptoms of dermatomyositis are muscle weakness and a rash on your skin.
Some patients notice muscle weakness and a rash at the same time. You might have one symptom for weeks, months, or actual years without further.
Muscle weakness might make it difficult for you to do familiar movements, involving:
- Sitting upright.
- Reaching up from a seated position (such as standing up from a chair or couch).
- Climbing stairs.
- Getting up after lying down.
- Washing your hair.
Dermatomyositis may generate a rash on your skin (particularly on regions of your body disclosed to the sun). Regions with a rash will be bruised and might be swollen. The most familiar sites contain:
- Eyelids and near your eyes.
- Chest and the front of your shoulders (occasionally referred to as a v-sign rash).
- Neck and the back of patient’s shoulders (a shawl sign rash).
- Scalp.
Further symptoms of dermatomyositis contain:
Discoloration and bumps (occasionally referred to as Gottron papules) on your hands, particularly near your knuckles.
Calcium deposits beneath your skin, in your muscles, or your connective tissue.
Bulges on your knees or elbows.
Rough cuticles and noticeable blood vessels on your fingernail folds.
Joint pain.
Some patients (particularly children) analyzed with dermatomyositis grow out of it and never have symptoms again. Yet, 80% of patients are chronic (they come back over time) and generate lifelong symptoms.
What causes dermatomyositis?
The reason for dermatomyositis stays unknown, but specialists think that a mixture of factors plays a role, involving:
genetic
environmental
immune system
Genetic factors
Patients with special human leukocyte antigen (HLA) varieties are at a higher risk of the disease.
Immune factors
HLAs are proteins that play a part in the body’s immune system.
Patients with dermatomyositis indicate an abnormal immune response, whereby the body’s immune system strikes small blood vessels, generating inflammatory changes in the:
- muscles
- skin
- blood vessels
Environmental factors
Physicians observe this state more often in women with disclosure to high-frequency UV radiation.
Specialists have also indicated that specific viruses could activate the disease. These contain:
- parvovirus
- enterovirus
- Coxsackie B virus
- echovirus
- HIV
- Medications
Certain medications can also activate dermatomyositis. These contain:
- anticancer medicines
- antibiotics
- Nonsteroidal anti-inflammatory medications (NSAIDs)
Silicone breast implants or collagen insertions may also activate or aggravate the state.
Risk factors
Anyone can create dermatomyositis. Yet, it’s most familiar in grown-ups between the ages of 40 and 60 and kids between the ages of 5 and 15.
The condition involves females twice as frequently as males. It involves more Black Americans than white Americans.
Related conditions
Dermatomyositis can improve a person’s risk of other diseases:
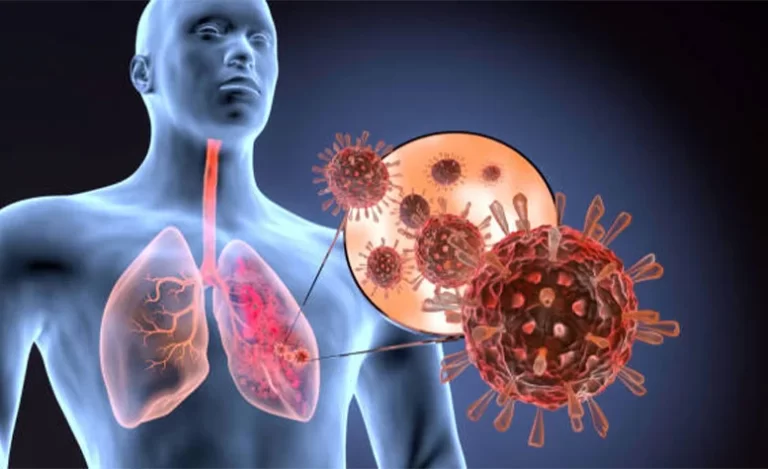
Lung disease
One-third of a patient with dermatomyositis have an interstitial lung condition, which includes inflammation and scar tissue in the lungs. A patient with respiratory muscle weakness may also create aspiration pneumonia.
Heart disease
Weakness and inflammation of the heart muscle can direct to:
- myocarditis
- congestive heart failure
- coronary artery illness
- Connective tissue disorders
Dermatomyositis can happen together with further connective tissue conditions, like:
- rheumatoid arthritis
- systemic lupus erythematosus
- scleroderma
- Raynauds disorder
This disease induces the sudden contraction of blood vessels in the hands and toes.
The consequent interruption of blood flow can conduct to:
- numbness
- tingling
- discoloration of digits
- Cancer
Many patients with dermatomyositis also have an underlying malignancy.
Malignancies happen in 24% of patients with grown-up dermatomyositis. This risk is most increased during the first 5 years following diagnosis.
Differential Diagnosis
- CREST Syndrome
- Parapsoriasis
- Graft Versus Host Disease
- Pityriasis Rubra Pilaris
- Lichen Myxedematosus
- Polymorphous Light Eruption
- Lichen Planus
- Psoriasis, Plaque
- Lupus Erythematosus, Acute
- Rosacea
- Lupus Erythematosus, Discoid
- Sarcoidosis
- Lupus Erythematosus, Subacute Cutaneous
- Tinea Corporis
- Morphea
- Urticaria, Chronic
- Multicentric Reticulohistiocytosis
How is dermatomyositis diagnosed?
Dermatomyositis is generally analyzed with blood examinations and biopsies of your skin and muscles.
Your provider or doctor will examine your blood for:
Raised amounts of precise muscle enzymes mean something is harming them.
Autoantibodies (cells that display your immune system is responding to something it sees as dangerous).
You’ll also require a skin biopsy of any hives. Your doctor might even biopsy your muscles to verify the inflammation inside them.
You might require one of a few imaging examinations. Your doctor will use these to assess your nerves, muscles, lungs, and further organs. These examinations can assist them to decide if your symptoms are generated by dermatomyositis or another issue. The most familiar imaging examinations used to diagnose dermatomyositis contain:
- Magnetic resonance imaging (MRI).
- Chest X-rays.
- In some circumstances, your doctor may order electromyography (EMG). This examination estimates electrical activity in reaction to muscle or nerve stimulation.
- muscle and skin biopsy
- barium swallow
cancer screening, which may include:
- colonoscopy
- Pap smear
- mammography
How is dermatomyositis treated?
Dermatomyositis treatments contain:
Corticosteroids: Corticosteroids will reduce the inflammation in your muscles.
Physical therapy: Physical therapy (and activity in general) can assist reconstruct harm in your muscles. The more powerful your muscles are, the better prepared they are to handle any harm from dermatomyositis.
Immunosuppressant medicines: Immunosuppressants prevent your immune system from harming nutritious cells and tissues. They can delay any harm your body’s protection is generating in your muscles.
Intravenous immunoglobulin (IVIg): IVIg is an infusion of additional immunoglobulin, a naturally happening part of your blood’s plasma. IVIg therapies can perform alongside immunosuppressants, or as an alternate therapy.
Calcium channel blockers: These medications extract calcium deposits and decrease the outcomes they may generate on the body.
Calcification surgery: Surgical methods can extract calcium deposits that are infected or aching.
Speech therapy: If you have muscle weakness in or near your throat, speech treatment can assist you to boost the muscles in your throat that assist you to swallow.
Which therapies you require relies on where you’re having symptoms, and how intense they are. Speak to your doctor about what to hope for and when you’ll require specific therapies.
Dietetic assessment. After the period of dermatomyositis, chewing and swallowing can evolve harder. A registered dietitian can guide you on how to ready easy-to-eat foods.
Sunscreens. Covering your skin from sun exposure by using sunscreen and wearing defensive clothing and hats is essential for controlling the rash of dermatomyositis.
Physiotherapy treatment
Other nonmedicinal management strategies may contain:
- adding more protein to the diet
- a soft food diet for a patient with dysphagia
- avoidance of or safety from the sun
- sleeping on a raised surface
- not consuming before bedtime
- general rest
Persons with mild conditions should be motivated to commit to active exercise schedules. Range of motion activities assists in controlling contractures. Persons with esophageal dysfunction may need to raise the head off the bed, thickening of meals, and even feed via gastric pipes when suggested.
The focus of Treatment should contain:
Strengthening to control atrophy once inflammation is prevented
Range of motion activities to control contractures
Passive stretching and splinting
Possible complications of dermatomyositis
The muscle weakness and skin issues connected with dermatomyositis can generate several issues. Some familiar difficulties are:
- skin ulcers
- gastric ulcers
- problem in breathing
- lung infections
- difficulties in swallowing
- malnutrition
- weight loss
Dermatomyositis can also be associated with diseases like:
- Raynauds phenomenon
- myocarditis
- interstitial lung condition
- further connective tissue conditions
- raised risk of developing cancers
Prognosis
It is essential to be observed by a healthcare doctor when you have dermatomyositis. The extreme disease can lead to disability and can occasionally outcome in death.
Symptoms may go out fully in some patients, like kids.
The disease may be fatal in grown-ups due to:
- Extreme muscle weakness
- Malnutrition
- Pneumonia
- Lung failure
The main reasons for death with this disease are cancer and lung condition.
Patients with lung conditions with the anti-MDA-5 antibody have a poor prognosis despite the present therapy.
FAQ
How serious is dermatomyositis?
Dermatomyositis is a severe condition that in infrequent issues can be fatal. It’s essential to get analyzed and start therapy as early as feasible. While there is no treatment for dermatomyositis, symptoms can frequently be controlled with long-term (occasionally life-long) drugs and physical therapy
What does dermatomyositis look like?
A reddish or purplish rash and scaly, bumpy skin are familiar in dermatomyositis. Inflammation of the fat lying only beneath the skin, known as panniculitis, also can happen, generating tenderness and feeling such as small bumps. The muscles of the upper arms, shoulders, hips, thighs, and neck show the most weakness.
Is dermatomyositis the same as lupus?
Dermatomyositis and autoimmune conditions such as lupus may have overlapping characteristics, yet, the rashes look very varied. A dermatomyositis rash has a purple-red shade that generally seems on your eyelids and joints such as the elbows, knuckles, knees, and toes.
Can dermatomyositis be cured?
There’s no treatment for dermatomyositis, but the duration of symptom progress can happen. Therapy can assist clear the skin rash and assist you to recover muscle strength and function.
Can you recover from dermatomyositis?
There’s no treatment for dermatomyositis, but therapy can enhance your skin and your muscle power and role.