Enteropathic Arthritis
What is Enteropathic Arthritis?
Enteropathic arthropathy, or enteropathic arthritis, is an umbrella term used to define different patterns of inflammatory arthritis which may be associated with a range of gastrointestinal (GI) pathologies. Its constituent states are classified as a piece of the seronegative spondyloarthropathies. Its different associated conditions are outlined below.
Spondyloarthritis and peripheral arthritis due to inflammatory bowel disease (IBD), eg. Crohn’s condition and ulcerative colitis. Varieties of arthritis associated with different GI pathologies involve Whipple’s condition, coeliac condition, and collagenous colitis, and following intestinal bypass surgery.
Pathophysiology
This is badly understood in enteropathic arthritis. Irregular permeability of the bowel to bacterial antigens, which then situate in articular tissues and lead to an inflammatory reaction, is one probable mechanism. Genetic susceptibility (especially HLA-B27 positivity) and immunological demodulation may also play a function. Cross-reactivity between articular tissue bacterial antigens and self-antigens may be the underlying immunological mechanism. HLA-B27 positivity may play its function by permitting bacterial peptide antigens to be shown to CD8+ cells, causing a cellular immune cascade. Intestinal bacterial hypergrowth is thought to be essential where the condition evolves after intestinal bypass surgery.
Enteropathic arthritis epidemiology
Rheumatic manifestations are the most regular extra-intestinal results of inflammatory bowel disease with a majority between 17% and 39%. Inflammatory bowel disease is also associated, less often, with other rheumatic conditions like Sjogren’s syndrome, rheumatoid arthritis, Takayasu’s arteritis, and fibromyalgia.
The joint or junction involvement kept in inflammatory bowel disease is generally classified into axial (involving sacroiliitis with or without spondylitis) and peripheral. Axial involvement is seen to be current in 2-16% of persons with inflammatory bowel disease. Peripheral joint or junction involvement has been documented in a broad range (0.4-34.6%) of persons with inflammatory bowel disease – IBD. It mainly affects the joints or junctions of the lower limbs. Females show more often a peripheral joint or junction involvement, whereas males tend to have an axial involvement.
Joint or junction involvement is the most familiar extra-intestinal presentation in kids with inflammatory bowel disease – IBD and may include 16-33% of persons at diagnosis or during follow-up.
Enteropathic arthritis commonly involves about 2-3% of all persons with Shigella spp., Salmonella spp., and Campylobacter spp. infections. Arthritis in persons who have undergone intestinal bypass surgery is relatively familiar.
Risk factors for enteropathic arthritis
HLA-B27 positivity is extremely associated with axial (spondylitis) states of the condition in inflammatory bowel disease – IBD, but not the peripheral form; enteropathic arthritis is also extremely associated with HLA-B27 positivity.
Probable risk factors for arthritis in persons with inflammatory bowel disease – IBD include active bowel disease, appendectomy, family history of IBD, cigarette smoking, and the presence of further extra-intestinal manifestations, like erythema nodosum or pyoderma gangrenosum.
Enteropathic arthritis symptoms
Joint or junction symptoms may present before, simultaneously, or after the diagnosis of inflammatory bowel disease – IBD. Symptoms contain:
Axial arthritis (spondylitis and sacroiliitis) associated with inflammatory bowel disease – IBD:
- The disease may precede any GI symptoms and be active despite adequate control of the bowel condition.
- There is a gradual start of low back aches radiating down the back of the legs.
- Symptoms tend to be severe in the morning.
- Long time sitting or standing can obtain the symptoms.
- Moderate motion tends to enhance the symptoms.
- Arthritis tends to be chronic and long-standing.
Peripheral arthritis of inflammatory bowel disease (IBD):
The disease is generally associated with gastrointestinal – GI symptoms but may bring some time to emerge after the beginning of bowel issues.
It is more probable to involve sufferers of Crohn’s condition rather than ulcerative colitis.
There is an asymmetric, oligoarticular arthritis that mainly involves the lower limbs.
The arthritis is generally transient and migratory but may involve progressively more joints or junctions in some patients.
Enthesopathy of IBD:
This tends to induce extremely localized aches in the heel where the insertion of the Achilles tendon is involved; condition of the patellar tendon causes ache on the tibial tuberosity or on the patella itself; the insertion of further tendons or different fascial sites can be inflamed causing, for instance, buttock ache or ache in the sole (plantar fasciitis).
Extra-articular manifestations of IBD:
Intestinal symptoms can involve diarrhea, abdominal ache, cramping, weight loss, and the path of blood or mucus per rectum.
There are dermatological associations with pyoderma gangrenosum involving ulcerative colitis patients, and erythema nodosum being seen with Crohn’s condition.
The mouth may be involved by recurrent, regular, aching aphthous ulcers.
The eye may be aching and red with blurred vision due to anterior uveitis.
Fever may be associated with inflammatory bowel disease – IBD, a chronic low-grade fever that may be a representation of secondary amyloidosis in Crohn’s disorder.
Reactive arthritis following intestinal infection:
This generally displays as an acute asymmetrical oligoarthritis with a predilection for the knee joints and ankle joints.
It may happen several weeks or months after the initial episode of enteritis.
Arthritis due to intestinal bypass surgery performed to correct morbid obesity:
Polyarthritis and an associated dermatitis may appear and are considered to be due to bacterial overgrowth happening in the bypassed area of the bowel, leading to the formation of pathological immune complexes; if the process is reversed then the symptoms settle.
Whipple’s disease arthritis:
This happens most generally in middle-aged males.
As well as the specific gastrointestinal – GI symptoms, there is a migratory polyarthritis that can precede gastrointestinally – GI symptoms by months to years.
Coeliac disease arthritis:
This is a relatively infrequent feature of the disease.
It tends to present as symmetrical arthritis of the hips, lumbar spine, knee joints, and shoulders and may be the presenting part of the condition before typical coeliac symptoms become obvious.
Arthritis generally fixes when the gut symptoms react to a gluten-free diet.
Collagenous colitis:
This is an irregular illness of unknown cause where there is a linear deposition of collagen under the epithelium of the colon.
It induces chronic watery diarrhea and abdominal ache.
Approximately 10% of those with the disease have peripheral arthritis of the hands and wrists joints that is responsive to non-steroidal anti-inflammatory drugs (NSAIDs).
The disease seems to be benign and self-limiting in the prevalence of patients but may cause long-term chronic disorder in a minority.
Signs
- Inspect the temperature to examine for proof of fever.
- Examine the eyes for proof of anterior uveitis.
- Examine the mouth to notice any ulceration or additional oral manifestations of inflammatory bowel disease – IBD.
- Inspect the skin for rashes, especially pyoderma gangrenosum and erythema nodosum.
- The joints or junctions should be carefully inspected to verify the presence of inflammation and to define the symmetry and severity of arthritis.
- The spine requires careful examination of its range of movement, and palpation for tenderness over the sacroiliac joints or junctions.
- Periarticular structures should be palpated to examine for proof of enthesopathy.
- Palpate the heel and soles of the feet to notice tenderness and swelling due to plantar fasciitis or Achilles tendonitis.
- Abdominal inspection is required to see any tenderness or suggest an alternative reason for intestinal symptoms.
Differential diagnosis of enteropathic arthritis
- Any reason for peripheral polyarthritis?
- Any reason for spondyloarthritis?
- Rheumatoid arthritis.
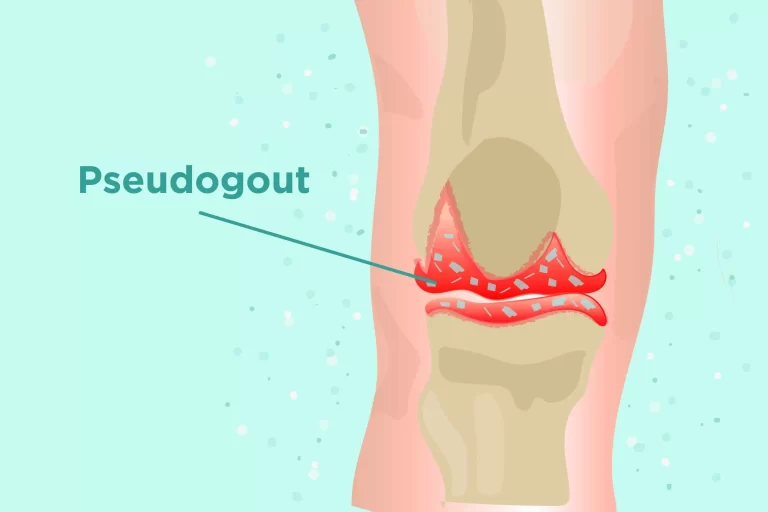
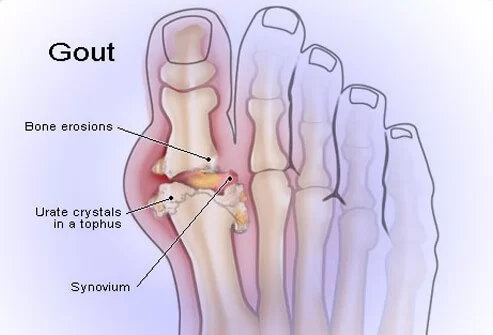
- Gout.
- Sarcoidosis.
- Gonococcal arthritis.
- Behcet’s disease.
- Lyme disease.
- Septic arthritis.
Investigations
Stool microscopy and culture where the etiology of any bowel condition is uncertain.
Sigmoidoscopy/colonoscopy/upper gastrointestinal – GI endoscopy may be required.
FBC to notice iron-deficiency anemia, leukocytosis, or thrombocythaemia associated with inflammatory bowel disease – IBD or other gastrointestinal – GI diseases.
ESR/CRP is generally elevated.
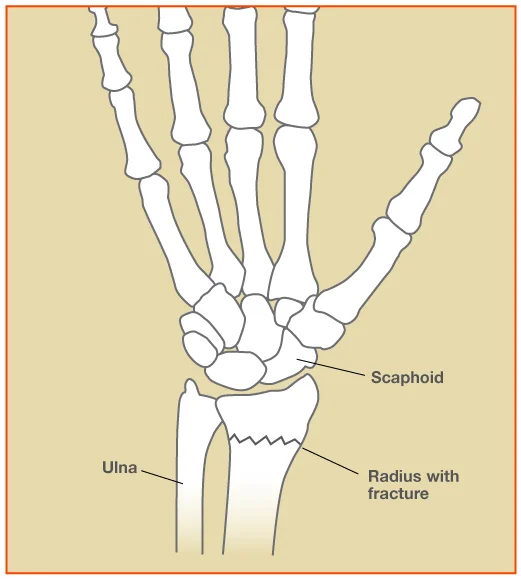
X-ray of involved joints or junctions (especially the spine/sacroiliac joints or junctions/calcaneum).
Synovial fluid aspiration and examination (displays mononuclear inflammatory cells and is culture-negative without crystals).
Consider autoimmune screen and anti-endomysial antibodies if there is fear of any other inflammatory disease/coeliac condition.
Enteropathic arthritis treatment
Monotherapy with local corticosteroid injections should be evaluated for non-progressive monoarthritis.
Standard disease-modifying antirheumatic drugs (DMARDs), like leflunomide, methotrexate, or sulfasalazine, can be used for persons with peripheral oligoarthritis, polyarthritis, or persistent or advanced monoarthritis associated with peripheral spondyloarthritis.
If a traditional DMARD accepted at the max tolerated dose for at least three months does not supply sufficient ease from symptoms, a switch to, or the addition of, further standard DMARD can be regarded.
An NSAID can be used as an adjunct to normal DMARDs or biological DMARDs to control symptoms. If NSAIDs do not supply sufficient ease from symptoms, evaluate corticosteroid injections or short-term oral corticosteroid treatment as an adjunct to normal DMARDs or biological DMARDs to control symptoms.
If an extra-articular condition is sufficiently maintained by an existing standard DMARD but peripheral spondyloarthritis is not, consider adding another traditional DMARD.
Non-drug
Keeping moderate exercise and spinal mobility with physiotherapy and activities is essential, especially for axial forms of the condition.
Modification of the diet, established on the underlying gastrointestinal – GI disease, may assist to relieve gut-related symptoms.
Extra-articular condition, especially those involving the eyes, needs early recognition and referral to professional services for management and monitoring.
When ulcerative colitis needs a colectomy; it has been shown to thereafter resolve peripheral joint or junction conditions but not axial arthritis.
Medical treatment
- NSAIDs may be utilized to manage acute joint or junction inflammation but must be given with care as they may aggravate gastrointestinal symptoms.
- Consider NSAIDs as an adjunct to standard DMARDs or biological DMARDs to control symptoms. If NSAIDs do not supply sufficient ease from symptoms, consider steroid injections (local or intramuscular) or short-term oral steroid treatment as an adjunct to normal DMARDs or biological DMARDs to control symptoms.
- Managing the underlying gastrointestinal – GI disease may enhance arthritis but this is frequently not the issue for axial arthritis associated with inflammatory bowel disease – IBD.
- Intra-articular and systemic corticosteroids are good for the peripheral arthritis of inflammatory bowel disease – IBD but have little impact on axial involvement.
- Sulfasalazine is widely utilized and is useful in treating both gastrointestinal GI and rheumatological symptoms in inflammatory bowel disease IBD, it should be provided under specialist oversight.
- Methotrexate, pamidronate, azathioprine, and ciclosporin have all been used as disease-modifying medications with variable victory, under specialist oversight.
- Tumour necrosis factor (TNF) antagonists are increasingly being offered to be useful agents in the management of inflammatory arthritis and bowel disease in IBD. They seem to be very useful against enthesopathy and axial conditions, which have traditionally been very difficult to manage. They are costly and can have important side effects; their use should be managed in professional clinics, preferably as a component of a clinical audit and ongoing approach development program. NICE advice on their use in inflammatory bowel disease – IBD and arthropathies is now available.
- Treatment or prophylaxis of osteoporosis using calcium, bisphosphonates, and vitamin D may be required.
Physiotherapy treatment
It’s necessary to do a mixture of activities, involving:
Stretching exercises
Strengthening exercises
Fitness exercises
Balance exercises
Stretching exercises
Stretching activities are occasionally called range-of-movement or flexibility activities. These include bending and straightening your joints or junctions as much as is satisfied to maintain them flexible and decrease the risk of any failure of mobility.
It’s effortless to avoid flexing and straightening your joints or junctions through their full range of motion during the day, especially when you have an ache. But not moving our joints or junctions completely can cause them to become more rigid and painful over time. They can be done as a warm-up before beginning further activities too.
A physiotherapist might be capable to give you some exact stretching activities. Further instances involve yoga and tai chi.
When doing stretching activities, you should try to move your joints or junctions as far as you comfortably can, until you sense a stretch in the muscles around the joint or junction. Try to maintain the motion slowly and control it.
Strengthening exercises
Strengthening activities assist to maintain the muscles around your joint or junction strong and secure. Owning strong muscles assists to maintain joints or junctions stable and can decrease pain in the joints or junctions and the tissues around them.
Modifications to our muscles can occur very fast you might see that you sense weaker or wobbly even after a few days of rest if you’ve been sick with a cold or flu.
To boost your muscles, you just require to move against some form of opposition. Even items like standing up from a chair will mean you’re boosting your leg muscles because you’re performing opposite to gravity.
Start strengthening activities gradually and build up how much you do gently. Begin with a low number of repeats of extra strengthening activities and add to this over a period. Your muscles should sense exhausted and like they have done some work after the activities.
You should aim to do some strengthening activities at least two days a week.
If your joints or junctions are hot or swollen because of your situation, it’s sometimes a useful concept to focus on stretching activities and avoid strengthening activities until they calm down.
Fitness exercises
Fitness activities are essential for everyone to stay fit. They’re sometimes called aerobic activities. This type of activity involves things like swimming, cycling, and doing activity classes.
Doing wellness or aerobic activities can assist to enhance the strength, balance, and range of motion of your joints or junctions, the health of your heart and lungs, and enhance your freedom.
Any activity that gets you breathing faster, or your heart beating faster benefits to enhance the way your heart and lungs function. Over a period, your energy levels, mood, and sleep can also enhance.
Balance exercises
It’s essential to do activities to enhance your balance two days a week, especially as we get more senior. This will assist decrease the risk of falls, which in turn decreases the risks of weakness and falls, which can have more difficulties as we age.
There are precise balance activities that can assist, but items like playing bowls, accomplishing tai chi, or dancing either at classes or near your home enhance balance also. If practicing your balance at the house, make confident the space near you is obvious of anything that could trip you up.
Different activities to try
There are many various kinds of exercise you can try, that will assist to enhance or support your general health and fitness. Try not to let the truth that there may not be further someone with arthritis doing these activities, as many of these exercises can be efficiently adjusted to fit you.
If you’re performing with a private trainer or fitness tutor, it’s a good thought to tell them about your situation and any problems you have before you begin. They should be capable to recommend changes to assist you to exercise safely and get the most use from an exercise.
Swimming and water-based exercises
Swimming performs the whole body but doesn’t include placing less weight via your joints or junctions so it’s an excellent way to work your muscles without placing pressure on your joints or junctions if they’re painful.
Most pools cater to a person with various requirements and capabilities, so if you’re new to swimming or are concerned about obtaining in and out of the pool, talk to somebody at your local pool as they may be capable to assist.
Being engaged in water isn’t only limited to swimming. It’s probable to do some activities for your situation, with the asset of the water helping ease pain in your joints or junctions, and even walking in the pool will function your body. There are also water-based aerobics courses, which include doing activities as part of a wellness class, in the water around waist height.
Good Boost uses technology to make water or land-based activity programs for a patient with arthritis or related diseases.

Walking
Walking briskly, even if solely for a short length of time, can assist enhance your lung and heart fitness, as well as helping your bones, joints, or junctions and muscles. You can also try adding periods of speed walking or walking uphill to contest yourself more.
Recall that any walking you do generally counts as physical exercise, but you can try going on roads around your local region, like walking around the park.

Running or jogging
Running or jogging can occasionally be challenging on your joints or junctions, but it also has great advantages for your wellness and can decrease sadness and fear. Try doing some strengthening activities for your legs before you begin.
Cycling
Cycling is a good activity to function your lower body and is low impact so shouldn’t cause more aches to your joints or junctions. It also brings you breathing faster and your heart beating quickly so is suitable for your heart and lungs.
To improve the intensity of your cycling, or to meet other people in a group class, you could try turning. This a low-impact wellness class done on exercise bikes. Your local gym may propose classes. You can also operate an exercise bike in a gym or obtain one for your house.
Some people see that doing physical exercise in a group can assist them to remain motivated. It can assist you to meet other people with a similar level of wellness to you and creating friends in your class can assist make the activity more satisfying.
Fitness classes contain aerobics and dance classes, but these don’t forever have to be high impact. Step aerobics and dance classes like Zumba can be appropriate for various levels of fitness.
Yoga
Yoga contains posture and breathing activities that can assist with your general wellness and range of motion, as well as enhance your mood. Its also been established to assist with back aches.
It involves gradual, gentle motions which can be easier for a person with joint or junction pain and will assist to enhance your muscle power and balance. It’s a good concept to find an educator who can assist you adjust some motions for your situation, particularly if you have had any joint or junctions replacements in the past.
Tai chi
Tai chi includes gradual, controlled motions and assists with your range of motion. It’s a great path for a patient with arthritis or joint or junction pain to enhance their muscle strength and balance too, without placing too much pressure on the joints or junctions.
Pilates
Pilates concentrates on balancing the body and enhancing your posture and can enhance how you feel. The balance exercises in Pilates, and tai chi above, are extremely useful as we get more senior as they can decrease the risk of falls.
Chair-based exercises
If you’re just beginning out with an activity, and you struggle with walking or have an ache in your legs, it can be a good concept, to begin with, some soft seated activities.
When you’re doing the activities, make sure to:
Select a chair of the right height, so you can sit with your knees flexed at a right angle and your feet flat on the bottom.
Avoid a chair with arms, as this could limit your motion during the activities.
Select an unmoving chair that doesn’t have wheels.
Gym
Gyms have lots of various tools you can use involving activity bikes and treadmills. So, if you’re feared about going outside to do these exercises, you can practice walking, cycling, or jogging indoors.
You’ll generally have an induction with a wellness tutor or private trainer when you enter a gym. If you have any problems, you can question them for guidance on training with your state.
Hot and cold packs
Cold can assist to ease pain and swelling. Heat can assist to decrease immobility. Use for no more extended than 20 minutes at a time.
A warm compress or paraffin wax hand bath can help involved joints or junctions. Using heat on the hand heats the synovial fluid that lubricates joints or junctions, reducing immobility, and enhancing flexibility.
Hydrotherapy
It operates water to manage arthritis. Specialized activities are conducted inside the water with a temperature range of 33-36 C . Physiotherapists advise the persons with typical activities like aerobics, stretching, and strengthening activities.
Complications
- Side-effects and toxicity induced by drug treatment.
- Complications of inflammatory bowel disease – IBD.
- Ocular difficulties due to uveitis.
- Secondary amyloidosis of Crohn’s condition.
- Loss of mobility and improving disablement in extreme possibilities of axial arthritis (irregular).
Enteropathic arthritis prevention
This is dependent very much on the exact underlying reason. Inflammatory bowel disease – IBD-related arthritis tends to maintain the more harmful long-term prediction, especially where there is severe axial involvement. The use of TNF-alpha antagonists is showing new hope in managing severe issues. The bulk of patients are amenable to useful treatment and keep an active and self-dependent lifestyle.
Prognosis
Disability can be avoided in those with axial arthritis, by the supervision of an activity program to maintain spinal mobility. There are no understood strategies to control inflammatory bowel disease – IBD or enteropathic arthropathy.
FAQ
How long does enteropathic arthritis last?
According to the Spondylitis Association of America, the duration and severity of enteropathic arthritis differ from patient to patient. While condition flares in enteropathic arthritis tend to be self-limiting and decrease after six weeks, repetition is familiar.
Does enteropathic arthritis go away?
Nowadays, there is no understood cure for enteropathic arthritis but there are drugs and treatments available to control the symptoms of both arthritis and bowel components of the condition.
Is Enteropathic arthritis reactive arthritis?
Enteropathic Arthritis belongs to a family of conditions known as seronegative spondyloarthropathies that involve psoriatic arthritis, ankylosing spondylitis, and reactive arthritis. Some with Enteropathic Arthritis feel a flare of joint or junction pain near the exact time that their bowel condition flares.
Is enteropathic arthritis symmetrical?
It tends to show as symmetrical arthritis of the hips, lumbar spine, knees, and shoulders and may be the presenting part of the disease before specific coeliac symptoms become evident. Arthritis generally determines when the gut symptoms react to a gluten-free diet.
What does Enteropathic arthritis feel like?
The symptoms of axial EA contain morning immobility, lower back pain, and pain after ample sitting or standing. Lower back ache is particularly familiar in a younger patient with axial EA. Early symptoms of peripheral EA involve joint or junction pain. Unlike osteoarthritis, it won’t cause deformation or weakening of your joints or junctions.