Muscle Tension Dysphonia (MTD)
Introduction
MTD, or muscle tension dysphonia, is a prevalent vocal problem. It happens when the voice box’s surrounding muscles are so tense that speaking impairs the voice box’s functionality. MTD is more common in individuals between the ages of 40 and 50, particularly in women.
- A generic term for an imbalance in the breathing patterns and muscle coordination required to produce voice is “muscle tension dysphonia.”
- Primary MTD refers to the imbalance that is shown in the absence of any anatomical defect, whereas secondary MTD is observed when an anatomical abnormality is present.
- Maintaining a suitable balance of tension between the voice muscles is essential for pleasant, effective speech and singing.
- Some muscles can withstand the amount of labor we put them through since they were meant to be the main actors in voiceovers. These include the muscles that govern pitch variation, vocal fold closure, and resonance balancing in the upper airway above the larynx.
- They also include the muscles of the vocal folds themselves.
- Other, less efficient muscles around the larynx are called upon to “help out” if these muscles become too tight or underutilized.
- The system eventually wears out and the voice starts to exhibit audible symptoms since these recruited muscles were not typically intended to be used for speaking.
- It might be difficult to generate, and discomfort or even pain could set in, especially if you talk loudly or against background noise.
- This condition is commonly known as muscle tension dysphonia or MTD.
- MTD often causes these vocal problems without causing any physical harm.
- On the other hand, if this method of speaking is continued consistently over time, MTD may occasionally result in physical changes. Typically, the alterations begin with mild thickening of the vocal folds, frequently accompanied by dryness and general irritation of the larynx.
- If the harmful vocal habits are maintained for a long enough period of time, the swelling may worsen to the point where the vocal folds stiffen and fibrous tissue grows in reaction to the repeated damage.
- Therefore, it’s critical that any hoarseness be examined by a laryngologist as soon as possible in order to rule out more serious causes and stop any physical changes from occurring.
- Voice problems resulting from frequent voice usage have been referred to by many different names and categories in the past, but the most popular term now is Muscle Tension Dysphonia.
- Other terms you could see include “Muscle Misuse Dysphonia,” “Muscle Imbalance Dysphonia,” “Vocal Hyperfunction,” and “Functional Dysphonia.”
- They are all linked to improper laryngeal muscle usage during vocalization, which is what unites them all.
- MTD can apply to vocal postures when there appears to be too little muscular effort in the vocal folds, generating weakness and bending, even though it is typically linked with constriction and excessive muscle effort (hyperfunction).
- In these situations, the overuse of force is coming from other, less functional muscles in and around the larynx.
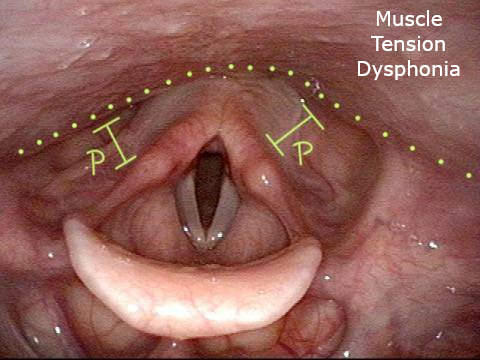
- Physicians frequently categorize MTD instances according to recognizable vocal posture characteristics.
- For instance, in “MTD with lateral compression,” the fake vocal folds and larynx’s side walls appear to be drawn inward toward the midline, while the vocal folds themselves appear long and stretched.
- It should be noted that in this image, the genuine vocal fold margins are not perfectly straight and instead appear “bowed.”
- In severe cases of this vocal posture, the fake vocal folds may even block the vision of the genuine vocal folds (also called “dysphonia ventricular is plicae” in the medical literature).
- Postero-anterior [PA] constriction is another way the larynx may narrow from the rear to the front, causing the arytenoid cartilages, which support the posterior or back ends of the vocal folds, to look dragged forward and obscure part or all of the vocal folds.
- Alternatively, the cuneiform cartilages can tilt backward due to anteroposterior [AP] constriction, which is the appearance of the epiglottis (or its base) at the front of the larynx being forced rearward and hiding the front/mid region of the vocal folds.
- To add to the complexity, laryngeal disease can either cause or be the cause of MTD development.
- For instance, if there is a little scar, sulcus, or venture on the vocal fold, or as compensation for a weak or paralyzed vocal fold, false fold constriction and lateral compression commonly occur.
- Therefore, before a diagnosis of MTD is established, it is crucial to thoroughly check the larynx and rule out any structural abnormalities.
- This posture was originally described as “muscular tension dysphonia,” however it was later renamed “laryngeal isometric disorder.”
- With all the terminology used in voice clinics, literature, and medical letters, it is understandable why patients may feel quite perplexed about their diagnosis especially when they are presented with a copy of the letter that their laryngologist submitted to their general practitioner (GP).
- From the perspective of the patient, it is crucial to keep in mind that all of these labels essentially mean the same thing: that the way the laryngeal muscles are utilized is what causes hoarseness rather than any illness or injury to the voice.
- Even though every person uses a distinct pattern, the voice clinic staff can recognize the issue, explain it, and set up the course of action that will most likely fix it problem.
What is muscle tension dysphonia?
- Excessive tension in the muscles around the voice box can cause a change in the sensation or sound of your voice, known as muscular tension dysphonia.
- The vocal folds and other laryngeal auxiliary muscles may be included in this.
- One type of dysphonia known as “functional dysphonia” is muscular tension dysphonia, in which a pattern of muscle usage arises due to irritation, laryngitis, or even stress, among other situations.
- The extreme strain or squeezing that comes with using one’s voice causes changes in voice quality even though the underlying reason may disappear.
The two types of muscle tension dysphonia
There are two types of dysphonia caused by muscle tension:
- When speaking, primary motor dystrophy (MTD) occurs when the neck muscles tense up significantly without any outward symptoms of a voice box or larynx problem.
- When there is an obvious indication that anything is amiss, secondary motor deficit (MTD) happens as a result of other muscles compensating to create speech. As a result of this, these muscles are overused, even though speaking doesn’t normally require them.
- If treatment is not received, MTD will probably get worse over time.
- An inability to generate voice and sore muscles might result from persistently high levels of muscular tension.
- Nodules or cysts may grow on the vocal fold in extremely uncommon and severe instances of MTD.
- If the individual learns to handle the underlying cause of the issue, such as stress or excessive vocalization, mild cases of MTD can be resolved.
What are the symptoms of muscle tension dysphonia?
The following are the most typical signs of muscular tension dysphonia:
- The voice that sounds rough, hoarse, gravelly, or raspy.
- The voice that sounds weak, breathy, airy, or is only a whisper.
- The voice that sounds strained, pressed, squeezed, tight, or tense.
- The voice that suddenly cuts out, breaks off, changes pitch, or fades away.
- The voice that “gives out” or becomes weaker the longer the voice is used.
- An excessively high or low pitch.
- Singing notes that were once easy becomes difficult.
- Speaking or singing can cause pain or stress in the throat.
- feeling as though your throat is worn out when you sing or talk.
How is muscle tension dysphonia diagnosed?
- The following procedure is used by a speech-language pathologist, sometimes referred to as a speech therapist, to diagnose MTD:
- Getting the patient’s medical history, including information on the onset and course of the voice issue as well as the patient’s current voice care practices
- Performing a thorough vocal evaluation that includes a larynx, head, and neck examination
- Assessing the speaker’s speech patterns, volume, and frequency of speech—basically, the way their voice sounds
- As part of the diagnosing procedure, a video-laryngostroboscopy what a mouthful! may also be suggested.
- This is an illustration of how sound is produced by the vibration of your vocal folds. It assists in locating any lesions, muscular tension, paralysis, stiffness, and aberrant motions.
- An otolaryngologist, an ENT physician, or a certified speech-language pathologist can do a video-laryngostroboscopy.
- Via your nose, a tiny camera linked to an endoscope and a tiny tube is introduced. The camera records slow-motion video of your larynx and voice folds.
- It just takes a minute or two to complete the test and to make the procedure more pleasant, you could be given a nasal spray.
Muscle Tension Dysphonia Treatment
- To minimize vocal strain and increase vocal efficiency, voice therapy with a speech-language pathologist is the mainstay of treatment for muscular tension dysphonia.
- In addition to voice therapy, you could be urged to investigate additional therapies that help you release stress, such as physical therapy, psychotherapy, acupuncture, or massage.
- In order to assist in lessening the pattern of muscular tension, voice treatment usually entails numerous sessions.
How does Muscle Tension Dysphonia present with symptoms?
- The symptoms of MTD are numerous and might differ across persons as well as within the same person.
- They can also come and go, such that occasionally the voice is fine and then the soreness and hoarseness come back for no apparent cause.
- Changes in voice quality are one indication to be aware of, especially at the end of the day or after prolonged voice use.
- Maybe the voice will begin to sound:
- Rough, hoarse, or develop a raspy quality
- weak, quiet, and breathing; it fades towards the end of phrases.
- Intermittent with voice ‘breaks’ where the sound cuts out briefly or where the voice is slow to start vibrating
- Pitch instability or extremes in pitch elevation or descent
- When speaking or singing, certain sensations may change, such as:
- Fatigue, hurting, or pain, particularly after prolonged or loud speaking or singing in front of others
- Dryness or scratchiness
- a perception that speaking requires effort and labour
- Vocal stamina may alter to the point that we are unable to sing or talk for as long without experiencing one or more of the symptoms listed above.
- This might be something little, like slight voice fatigue at the end of a hectic day, or it could be something serious, with symptoms appearing after just 10 minutes of speaking.
How is a diagnosis of muscle tension dysphonia made?
- The only way to diagnose MTD is with a laryngeal examination.
- In a voice clinic, an ENT surgeon or laryngologist and a speech-language pathologist (SLT) would ideally collaborate to observe the larynx during voice production in order to determine the underlying reasons for your voice issue.
- To find out whether there are any additional health issues or lifestyle choices that might be causing or exacerbating the MTD, a thorough medical history will be gathered.
- Prior to beginning voice treatment, it is critical to identify and address any contributing issues.
- In order to keep track of the course of treatment, they will also analyze the voice’s production and record its tone.
Why does muscular tension dysphonia occur?
The formation of an MTD is often influenced by many variables. The most typical ones consist of:
- Long-term patterns of ineffective voice use
- Abrupt alterations in voice quality brought on by vocal overuse, an infection, or psychological strain Remedy for an underlying issue with the vocal folds, such as paresis, a cyst, or vocal muscle exhaustion
- ‘Guarding’ in reaction to irritations such as acid reflux
- a mix of some or all of the elements listed above
How does one cure muscle tension dysphonia?
- A SLT with expertise in voice problems often treats MTD in the absence of any other abnormalities in the vocal folds, depending on the diagnosis.
- Depending on how long the issue has existed and how well the patient responds to treatment, the course of treatment might take as little as a few sessions or several months.
- Reducing excessive or misplaced laryngeal tension is the aim of voice treatment, which aims to restore the proper function of the vocal muscles.
- The ENT surgeon will explain and go over the potential medicinal and surgical treatment options if MTD is the main factor causing damage to the vocal fold, or if it has formed as a stand-in for a voice or health issue.
What does Voice Therapy involve?
- Your SLT will work with you to examine how you use your voice and pinpoint any problematic vocal habits or lifestyle choices that may be aggravating your voice condition.
- To assist you in discovering a more efficient method to generate your voice whether speaking or singing, your therapist will employ a variety of techniques.
- These might consist of:
- Working on your posture
- Enhancing your breathing technique to help your voice
- methods of relaxation to lessen overall stress in the neck and shoulders, which is a contributing factor to voice tension
- certain vocal exercises intended to shift the workload to the right vocal muscles
- Laryngeal massage to ease laryngeal muscle and throat strain
What steps can I take to lessen my chances of developing muscle tension dysphonia?
- By taking excellent care of your voice, you may lessen the likelihood that MTD will develop or at least lessen its symptoms.
- You should especially avoid doing the following:
- Yelling and screaming
- Speaking/singing excessively loudly, especially against noise
- Speaking/singing outside your own comfortable pitch range
- Vocal muscle tension or tightness during speaking or singing
- Speaking of singing while having trouble breathing or not getting enough oxygen
- Speaking with a hard glottal attack
- Excessive coughing and throat-clearing
- Whispering or trying to protect the voice
Origins of Dysphonia Due to Muscle Tension
- In addition to acid reflux, upper respiratory infections, increased stress or anxiety, or even demanding vocal work can all cause muscle tension dysphonia.
- Additionally, vocal fold paresis/paralysis, vocal fold atrophy, or benign vocal fold lesions may manifest as a compensatory condition for this voice disorder.
Symptoms
- A strained quality is a common characteristic of muscle tension dysphonia.
- Patients who use their voices for lengthy periods of time during the day may experience vocal fatigue and a sense that it takes effort to generate their voices.
- The voice may sound erratic raspy or harsh.
- Vocalizing occasionally might cause pain in the neck or throat. Patients with more severe conditions are unable to speak louder than a whisper.
Diagnosis
- The Voice and Swallowing Center’s voice care staff has the extensive knowledge and expertise required to identify this vocal problem. You will be examined by one of our laryngologists on your first appointment, and you will probably also see one of our voice pathologists again.
- Modern diagnostic procedures are used to identify the underlying cause of your voice problem and create a personalized treatment strategy.
- After a detailed discussion of your medical history and symptoms, you should anticipate undergoing the following assessments:
- Video Laryngostroboscopy: With the use of a tiny camera that is placed through the mouth or nose, our experts can evaluate the condition and functionality of your larynx, or voice box, as well as check for any compression of the muscles that surround the vocal folds when you are voicing.
- Perceptual, Acoustic, and Aerodynamic Voice Evaluation: The voice pathologist completes this thorough evaluation of several voice characteristics.
Non-Surgical Treatment for Muscle Tension Dysphonia
- The most effective treatment for muscular tension dysphonia is voice therapy.
- By using voice therapy procedures, patients may generate their voices more effectively and with better breathing and vocal coordination. Additional methods might involve approaches to reducing stress, such as stretches for the head and neck and massages to the muscles behind the larynx, known as circumlaryngeal massages.
- Treatment for the underlying voice disease may be required if muscular tension dysphonia is caused by another laryngeal issue.
How is muscle tension dysphonia diagnosed?
- The following procedure is used by a speech-language pathologist, sometimes referred to as a speech therapist, to diagnose MTD:
- Getting the patient’s medical history, including information on the onset and course of the voice issue as well as the patient’s current voice care practices
- doing a thorough vocal evaluation that includes a larynx, head, and neck examination
- evaluating the speaker’s speech patterns, volume, and frequency of speech—basically, how they sound.
- As part of the diagnosing procedure, a video-laryngostroboscopy what a mouthful! may also be suggested.
- This is an illustration of how sound is produced by the vibration of your vocal folds.
- It assists in locating any lesions, muscular tension, paralysis, stiffness, and aberrant motions.
- An otolaryngologist, an ENT physician, or a certified speech-language pathologist can do a video-laryngostroboscopy.
- Via your nose, a tiny camera linked to an endoscope and a tiny tube is introduced.
- The camera records slow-motion video of your larynx and voice folds.
- The exam only takes one or two minutes, and you may receive an anesthetic nose spray to make the experience more comfortable.
How to treat muscle tension dysphonia
- For MTD patients, voice therapy with a qualified speech-language pathologist is typically advised. Voice therapy teaches you how to:
- Relax your throat muscles
- Boost your breath support to speak more clearly.
- When speaking, make use of the proper oral resonance—the air passing through your nose and mouth.
- Your speech therapist will teach you voice and breathing exercises as part of your treatment.
- By completing these exercises, you’ll be able to determine the ideal pitch and loudness to talk with, as well as lessen throat strain.
- The primary goal is to talk with the least amount of voice strain.
- Your speech therapist could suggest myofascial release and laryngeal massage during speech therapy.
- This involves gently extending and massaging any tense areas in the head, neck, and chest. Following these procedures, many persons experience improvement from pain and throat strain.
- To further ease the muscles, your speech therapist will teach you how to perform these massages on your own.
- Although MTD can be excruciating and infuriating, there is a workable cure.
- A speech-language pathologist can help you restore the health of your vocal system with the appropriate exercises and relaxation methods.
- Get an assessment from a speech therapist if you think you might have MTD.
Common Causes of MTD
Overuse of the voice: Tension and discomfort in the muscles might result from shouting, speaking strained, or using the voice chords excessively.
Emotional Stress: The health of our voice is directly related to our emotional state. Tension in the laryngeal muscles can cause stress, worry, and emotional upheaval, which can affect our voice.
Lifestyle Practices: MTD can be exacerbated by bad vocal habits, such as speaking too loudly, in pitch, or with inefficient use of the voice.
Underlying Health Issues: Irritation and muscle tension can be caused by ailments such as respiratory infections, allergies, or acid reflux.
Symptoms of MTD
Hoarseness: Your voice can become raspy and hoarse, losing its clarity.
Vocal Fatigue: You may experience vocal exhaustion from even brief interactions.
Pain and Discomfort: Singing or speaking aloud can make your neck or throat hurt.
Restrained Voice: You might think that you’re straining too hard to make a sound.
Voice Changes: You could find it difficult to maintain consistency with your pitch.
Conclusions
The pathological condition known as MTD is characterized by an excessive tension of the (para)laryngeal muscle, which can result in a disordered voice due to a variety of etiological reasons. The range of etiological causes encompasses everything from vocal abuse and misuse to psychological and personality problems.
It also includes compensatory vocal behaviors in cases of upper airway infections, lesions, and laryngopharyngeal reflux. It is necessary to treat MTD in a multidisciplinary environment where a laryngologist and a speech-language pathologist may work closely together.
FAQ
What causes muscle tension dysphonia?
Anxiety and stress are linked to primary MTD. Recent studies have demonstrated that the voice box’s controlling muscles contract during stressful times. Vocal control system incoordination can result from extended periods of tense muscles in the voice box.
Can you recover from muscle tension dysphonia?
In certain instances, minor MTD may go away if the underlying cause—such as stress or excessive voice use—goes away. Severe instances, however, are likely to worsen over time due to the ongoing increased muscular tension, which can cause aching muscles and the inability to create voice.
Is MTD permanent?
It is possible that MTD will not go away on its own, even if the underlying cause is treated. For the treatment of habitual muscular tension, voice therapy could be required. An analogy for this would be modifying one’s posture to put less weight on a damaged ankle in order to compensate for it.
How do you stop muscle tension dysphonia?
We provide a variety of therapies to address muscular tension dysphonia (MTD): The most often-used kind of treatment for MTD is voice therapy. It might involve massage and resonant voice methods. Injections of Botox: In order to halt voice box spasms, voice treatment and Botox are occasionally combined.
Who treats MTD?
A speech-language pathologist will do vocal evaluations and voice therapy sessions as part of the treatment plan for MTD. Every other week, voice therapy sessions last one hour and involve exercises that target resonance and airflow to relieve tension in the voice box.
References
- BRITISH VOICE ASSOCIATION : Muscle Tension Dysphonia (MTD). (n.d.). https://britishvoiceassociation.org.uk/voicecare_muscle-tension-dysphonia.htm
- Muscle Tension Dysphonia. (2023, February 24). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/muscle-tension-dysphonia
- Ccc-Slp, A. C. M. (2022, May 13). What Is Muscle Tension Dysphonia, and How Is It Treated? Expressable. https://www.expressable.com/learning-center/voice/what-is-muscle-tension-dysphonia-and-how-is-it-treated
- Gupta, R. (2023, December 20). Muscle Tension Dysphonia: Causes and Effective Treatment Options — Center for Vocal Health | ENT & Laryngology. Center for Vocal Health | ENT & Laryngology. https://www.centerforvocalhealth.com/vocal-health-and-care/exploring-muscle-tension-dysphonia-causes-symptoms-and-treatment-options