Frey’s syndrome
What is Frey’s syndrome?
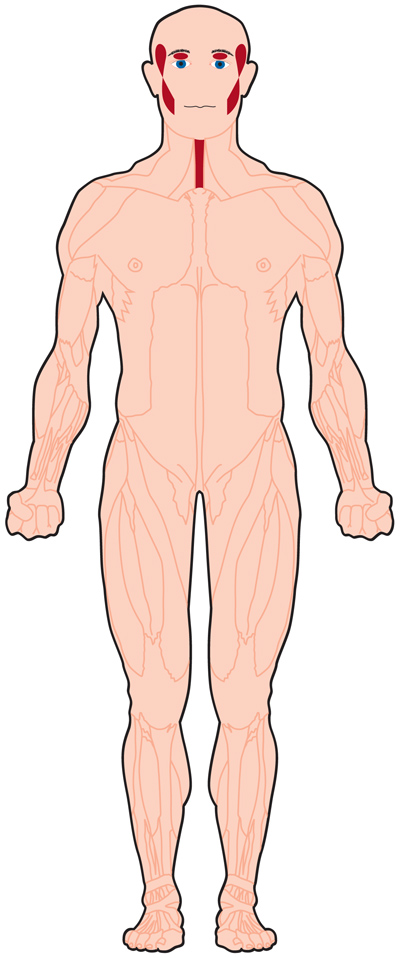
Frey’s Syndrome (FS) is the phenomenon secondary to gustatory stimulus, exemplified by flushing and sweating of parotid, frontal, and sub-mandibular sites resulting in trauma to the parotid or another major salivary gland (eg. sub-mandibular or sub-lingual) frequently either after a parotidectomy or excision of the sub-mandibular gland. In other words, Frey’s syndrome – FS is characterized by excessive sweating of the upper lip, the forehead, the peri-oral region, or the sternum after gustatory stimuli. Other areas can be involved in Frey’s syndrome – FS. These contain the:
Occipital region
Cervical region
Ear region
Temporal hair region
Epidemiology
The published incidence of Frey syndrome after parotidectomy ranges from 4% to 96%. The wide spectrum of rates noted in the literature reflects great heterogeneity of symptom reporting, severity, and diagnosis.
The incidence of Frey syndrome approaches 80% in parotidectomy people based on the Minors starch-iodine test but varies from 30% to 60% based on subjective peoples reports, showing that there is probably a population of asymptomatic Frey syndrome patients or patients with non-bothersome symptoms.
There do not seem to be age or gender predilections for the development of Frey syndrome.
Freys syndrome symptoms
The symptoms of Frey syndrome can contain sweating, flushing, neuralgia, burning, and itching. The symptoms of Frey syndrome generally develop within the first year after surgery in the region near the parotid glands. In some patients, Frey syndrome may not evolve until several years after surgery. The typical symptom of Frey’s syndrome is gustatory sweating, which is extreme sweating on the forehead, cheek, and near the ears shortly after eating specific foods, especially foods that produce a strong salivary response like spicy, sour, or salty foods. Typically, the symptoms are mild but can result in discomfort as well as social stress and avoidance.
Further symptoms that may be associated with Frey’s syndrome contain flushing and warmth in the involved regions. This is infrequently an essential complaint.
While further symptoms have been associated with Frey’s syndrome, they are likely unrelated. Pain is occasionally defined, but it is probably more related to the surgery than even to Frey syndrome. The typical area involved, the size of the region, and the degree of sweating and flushing differ greatly among involved individuals. In some people, symptoms may be mild and involved individuals may not be bothered by the symptoms. In other patients, like those that experience profuse sweating, involved individuals may need therapy.
Causes of Frey’s syndrome
Anything that hurts the auriculotemporal nerve can result in Frey syndrome, containing the following:
- Parotid gland surgery (biggest cause)
- Blunt trauma to the cheek
- Neck surgery
- Chronic infection of the parotid region
- Mandibular fracture
- Fracture of the temporomandibular junction or joint
- Surgery to the temporomandibular junction or joint
- Removal of the submandibular glands
- Removal of the thyroid gland
- Thoracic sympathectomy (a surgery done to maintain sweating)
- Birth trauma or damage following forceps delivery (in infants)
- In the 1940s, parotid gland surgery was popularized in the United Kingdom to manage a broad variety of diseases, both cancerous and noncancerous.
Gustatory sweating along with several further adverse effects, including reduced facial sensation, facial nerve injury, hematoma, salivary fistula, and keloids were generally observed among patients who obtained parotid gland surgery.
Of note, a patient who has their entire parotid gland removed is more possible to experience Frey syndrome than those who have only part of the parotid gland removed.
Frey syndrome can also be noticed with the further following neurological disorders:
- Facial herpes zoster
- Chorda tympani injury
- Cluster headache
- Diabetic neuropathy
- Encephalitis
- Syringomyelia
- Tumor in the cervical sympathetic trunk
- Most patients who experience gustatory sweating aren’t bothered by it only between 10 and 15 percent of a patient who experiences it seek medical alert. Also, after parotid surgery, only 10 percent of people report symptoms.
Yet, on further questioning, 30 to 50 percent of people will recognize symptoms of gustatory sweating. Frey syndrome generally occurs between 1 and 12 months after surgery.
Frey syndrome can occur in a patient at any age. However, it is irregular in infants and children who only really ever experience injury to the parotid region after a forceps delivery, and injury from forceps delivery is irregular.
In kids, food allergy can be misunderstood as Frey syndrome. Nevertheless, the symptoms of food allergy appear after the ingestion of food not during chewing.
Diagnosis
The easiest method to diagnose Frey syndrome includes the application of iodinated starch (indicator) powder to the face. This method is known as the Minor test.
The patient is then provided lemon sweets or some further sweet food to stimulate sweating. Involved regions where sweat droplets form turn blue-black. The droplets can be easily brushed away from the face so that the test may be replicated.
This test can also be utilized to test for Frey syndrome in a patient without symptoms (eg, asymptomatic people).
Although this test is valid, it will not show the severity of the situation. Similarly, this test brings the potential risk of inhalation of the starch powder. This examination should be administered on dry skin, and shouldn’t be used on a patient who perspires heavily.
Another more costly and involved diagnostic test to decide whether a patient has Frey syndrome includes a biosensing process that utilizes enzymatic electrodes that notice L-lactate levels on the skin.
A more rudimentary examination for Frey syndrome includes the application of one-ply tissue paper to the face to study for sweating after the people is stimulated with sweet food.
Finally, infrared medical thermography can be utilized to visualize Frey syndrome. This diagnostic examination needs the temperature and humidity in the room to be continued.
First, after stimulation, a hot spot is observed that corresponds to the dilation of subcutaneous blood vessels. Second, a cold spot is observed that represents gustatory sweating. These differences are harder to visualize in a patient with darker skin.
Treatment of Frey’s syndrome
Medical treatment
In most patients, Frey syndrome goes out on its own within at most 5 years. Patients with mild symptoms should be soothed that the situation will pass on its own without therapy.
In those who are extremely impacted by the disease, gustatory sweating is generally the most distressing symptom and prompts a patient to seek aid.
- Botox
- Antiperspirants
- Topical Anticholinergics
Topical anticholinergics used to treat Frey syndrome contain:
- Scopolamine
- Glycopyrrolate
- Diphemnanilmethylsulfate
- This medication is used as a roll-on solution or cream and enhances symptoms for almost 3 days.
Side effects of topical anticholinergics contain:
- Dry mouth
- Blurred vision
- itchy eyes
- Urinary retention
- Increased heart rate
- Allergies
- Also, anticholinergics should not be used in a patient with diabetes mellitus, glaucoma, obstructive uropathy, thyroid disease, as well as a renal, hepatic, cardiovascular or central nervous condition.
Surgical Options
Third, surgery has been unsuccessfully tried to attenuate the symptoms of Frey syndrome. These surgeries contain:
- Cervical sympathectomy
- Tympanic neurectomy
- Sternocleidomastoidtransfer transfer
- Dermis-fat grafts
- Further, different materials and interposition barriers have been used to manage gustatory sweating.
Understandably, a most patient who develops gustatory sweating secondary to surgery is reluctant to accept more surgery to manage this disease.
Physiotherapy treatment in Frey’s syndrome
Purpose: Changing the physical and mechanical properties of the scar by controlling the scar maturation cycle. Even promoting tissue strength and gliding by controlling adhesions.
Scar massage: During the proliferative phase massage has a useful role in collagen synthesis, as it controls adhesions and supports collagen synthesis. Also, this mechanical pressure when applied to the intermolecular bonds assists in realigning collagen.
Splinting: Splinting can be utilized at all phases of wound healing, to immobilize at the earlier phases and with the aid of passive or active stretches to modify collagen alignment. Static and dynamic splinting can change the viscoelastic properties of tissues therefore it can elongate and stretch tissues over time.
Silicon gel: Silicone gel via sheeting and elastomers is said to have a hydrating impact on the scar. It assists to soften and elongate a scar by improving the pressure, temperature, and in turn blood flow to the scar.
Ultrasound therapy: The known impact of ultrasound is to facilitate recovery in the inflammatory and proliferative phases. It facilitated the synthesis of growth elements that in turn improved the strength and elasticity of the collagen fibers formed
Laser: Laser inhibits collagen and enhances keloid and hypertrophic scarring. It enhances pruritus but has no impact on the cosmoses of the scar.
Extracorporeal shock wave therapy (ESWT): Extracorporeal shock wave therapy (ESWT) is a noninvasive therapy that affects scar remodeling via fibroblast regulation. According to the Patient and Observer Scar Assessment Scale (POSAS), ESWT demonstrated favorable results in hypertrophic scars in a study that supplied data to support further studies into the use of ESWT for the therapy of hypertrophic scars.
Pressure Therapy: When used for edema control and cosmoses in a matter of keloid and hypertrophic scars. These garments inhibit collagen synthesis in a remodeling scare via an unknown mechanism. Pressure treatment can decrease scar height and erythema when used for 23 hours per day for 12 hours. This should be used at 20 to 30 mmHg and substituted every 2 to 3 months. This decreases abnormal pigmentation and accelerates scar maturation
Prognosis
Frey syndrome is a benign disease and manages not progress once established. Asymptomatic people are rarely treated and are analyzed only for academic goals. Most people who present with symptoms can be managed effectively with conservative medical administration, involving topical anticholinergics, antiperspirants, and botulinum toxin. Those with severe or refractory patients can be managed with surgery.
In kids, spontaneous symptom relapse happens in 69% of unilateral presentations. The bilateral form is generally unrelated to postnatal trauma and decides during the first year of life in 58% of people.
FAQ
Which nerve is involved in Frey’s syndrome?
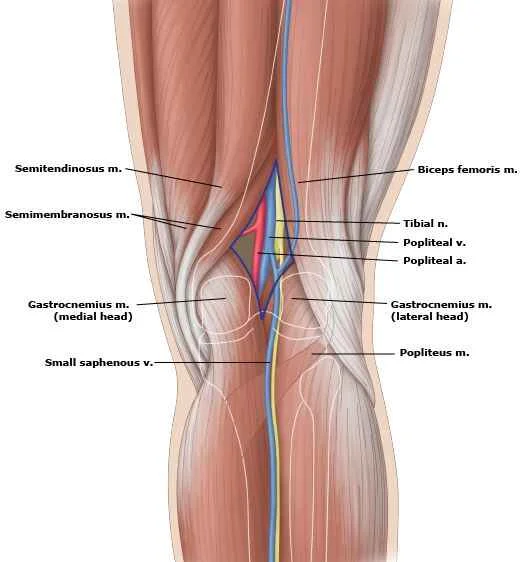
Frey syndrome generally happens in grown-ups with auriculotemporal nerve injury due to surgical manipulation or trauma in the parotid area.
When does Frey’s syndrome occur?
The disease most frequently happens as a complication of the surgical removal of a parotid gland (parotidectomy). The percentage of people who develop Frey syndrome after a parotidectomy is controversial and notified calculations to range from 30-50 percent.
How do you prevent Frey syndrome?
The most useful way to avoid Frey’s Syndrome is to minimize surgical trauma. The only way to do this is to have minimally invasive surgery. Minimally invasive surgery only includes the parotid gland. It does not expand into the temple and neck, the cheek, as traditional parotid surgery does.
Can Frey syndrome be cured?
Frey’s Syndrome is due to injury of the auriculotemporal nerve and leads to sweating and flushing of the face associated with eating or guessing about food. This injury commonly occurs during surgical methods of the parotid gland. Permanent therapy is available in the state of reconstructive surgery.
How do you reduce the effects of Frey?
Frey’s syndrome is primarily managed with Botox injections, which are useful but must be replicated every 4 to 6 months. A person can also apply antiperspirant to the skin, which can decrease perspiration but does not decrease flushing on the skin. Many peoples have such mild symptoms that they decide to do nothing.