Gout on Foot
What is Gout on Foot?
The foot and ankle are common places of deposit of monosodium urate( MSU) chargers, as indicated by the clinical abstract presented by cases with gout, which aren’t limited to the acute inflammation of the big toe. Gout may be a painful form of arthritis.
When your body has extra acid, sharp crystals may form within the joints, causing episodes of swelling and pain called gout attacks. Gout is treatable with drugs and changes in diet and lifestyle Gout may be a disease that can move through several stages:
- Hyperuricemia is when you have elevated levels of urate in your blood and crystals are forming in the joint, but you are doing not have symptoms.
- Gout flares, once you have an attack of intense pain and swelling in your joints.
- Interval or inter-critical gout is the time between gout attacks when you do not have any symptoms.
- Tophi may be a late stage of gout when crystals build up in the skin or other areas of the body. counting on their location, tophi can permanently damage your joints and other internal organs like the kidneys. Proper treatment can prevent the event of tophi.
How to Identify Gout?
the pain can be so severe that they can not tolerate the weight of a mask. The symptoms are generally at their worst within 6 – 12 hours. The affected joint, or big toe, will recover in 1 – 2 weeks.
The following are suggestions that a person is passing a gout attack in the big toe and foot
intense joint ache on the big toe or foot
rapid onset
swelling and redness ( red color appearance ) or abrasion
tenderness when palpating the foot
difficulty shifting
Who is affected by gout?
Gout can affect anyone. it always occurs earlier in men than women. It generally occurs after menopause in women. Men are often three times more likely than females to urge it because they have had higher levels of uric acid most of their lives. Women reach these acid levels after menopause.
People are more likely to urge gout if they have:
- Overweight/obesity.
- Congestive coronary failure.
- Diabetes.
- Family history of gout.
- Hypertension (high blood pressure).
- Kidney disease.
You are also more probably to develop gout if you:
- Consume a diet high in animal proteins.
- Consume a big amount of alcohol.
- Are on water pills (diuretics).
How does a doctor diagnose gout?
If you’ve got sudden or severe pain in a joint, you ought to talk to your primary care provider (PCP). Your Primary Care Provider may send you to a rheumatologist, a doctor who focuses on gout and other kinds of arthritis.
- Healthcare providers consider many things when confirming gout:
- Symptoms: The provider will ask you to explain your symptoms, how often they happen and the way long they last.
- Physical examination: Your provider will examine the affected joint(s) to see for swelling, redness, and heat.
- Blood work: A test can measure the quantity of uric acid in your blood.
- Imaging tests: you’ll have pictures taken of the affected joint(s) with X-rays, an ultrasound, or an MRI.
- Aspiration: The provider may use a needle to tug fluid from the joint. employing a microscope, a team member can search for uric acid crystals (confirming gout) or a special problem (such as bacteria with infection or another type of crystal).
Diagnosing gout when no crystal identification is feasible
Ideally, 6 of 10 features are going to be present the following:
- Inflammation reaches a maximum at some point (rapid acceleration of inflammation).
- Having a history of a comparable episode of inflammation
- Attack of arthritis during a single joint.
- Redness over an involved joint (gout is very inflammatory)
- Involvement of the bottom of the big toe on one side (the most common site for gout)
- Involvement of the joints at the center of the foot
- Uric acid elevation on blood testing
- X-ray findings of swelling of joints which isn’t symmetrical
- Junction fluid is tested for infection and is negative.
- X-ray shows the identification of changes in gout, including cysts in bone and erosions.
how to treat gout on foot?
Medications
Your healthcare provider may prescribe certain drugs to treat gout.
Some drugs help control symptoms:
- NSAIDs can reduce pain and swelling. Some people with renal disorders, stomach ulcers, and other health problems are unable to require NSAIDs.
- Colchicine can reduce inflammation and pain if you’re taking it within 24 hours of a gout attack. It’s given orally.
- Corticosteroids can relieve pain and swelling. you’re taking steroids by mouth or with an injection.
Drugs that help lower levels of acid in your body to prevent or reduce future episodes of gout attacks:
- Allopurinol is taken as a pill.
- Febuxostat is taken as a pill.
- Pegloticase is given as an intravenous (in the vein IV ) infusion.
- Probenecid is taken as a pill.
Physiotherapy Treatment
Benefits of Exercise
Physical movement is beneficial for a variety of reasons:
- Aid and manage weight loss
- Increase range of motion
- Strengthen your joints
- Promotes bone strength
- Speed up the recovery process
- Feel more energized
- Help control blood glucose
- Reduces risk for a heart condition
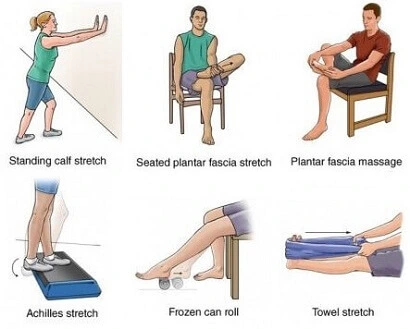
- Achilles tendon and plantar fascia stretch
Loop a handkerchief around the ball of your foot and pull your toes towards your body, keeping your knee straight. Hold for 30 seconds. Repeat 3 times on each foot.
2. Plantar fascia stretch
Sit down, take a rest, and put the arch of your foot on a round object, like a tin of beans. Roll your foot on the tin altogether directions for a few minutes. Repeat this exercise is done twice each day.
3. Sitting plantar fascia stretch
Sit down and cross one foot over another knee. Grab the bottom of your toes and pull them back towards your body, until you are feeling a comfortable stretch.
Hold for 15-20 seconds. Repeat this 3 times.
4. Calf Stretch
Stand facing a wall, together with your hands flat against it.
Keeping your heels flat on the ground and back straight, slowly lean into the wall—as though you’re doing a pushup against the wall. You can start standing very near the wall; then gradually move a little further away to get a better stretch.
Hold for some seconds; then relax and repeat.
5. Toe Salutes
Resting flat feet on the ground in a sitting position.
Lift your great toe, while keeping the opposite four toes on the floor. Hold for some seconds; then relax and repeat.
Lift your four toes together, while keeping the large toe on the floor. Hold for some seconds; then relax and repeat.

6. Toe Splaying
Resting flat feet on the ground in a sitting position.
Spread all of your toes apart as far as comfortable. Hold for some seconds; then relax and repeat.

7. Toe Squeezing
Place foam toe dividers between your toes (such as pedicure toe dividers).
Squeeze your toes together for some seconds; then relax and repeat.
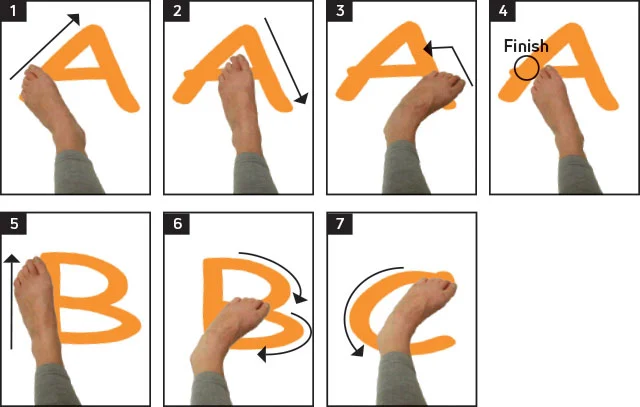
8. Ankle Alphabet
Sit down in order that your feet don’t touch the floor.
Use your foot to write down each letter of the alphabet in the air, leading together with your big toe. Keep the motions small, foot and ankle only use.
9. Towel Curls
Resting flat feet on the ground in a sitting position.
Place a little towel on the ground in front of you.
Grab the middle of the towel with your toes and scrunch your toes, curling the towel toward you. Relax, then repeat.
10. Towel pickup
Sit down with a towel on the ground in front of you. Keeping your heel on the bottom, devour the towel by scrunching it between your toes. Repeat 10 to twenty times. As you improve, add a little weight, like a tin of beans, to the towel.

11. Toe Extension
Sit on a chair, together with your feet resting on the floor.
Pick one foot and place it on the opposite thigh. Hold on to your foot with one hand.
Grab your toes with the opposite hand and bend them toward your ankle and hold for a few seconds; then back toward your heel and hold for a few seconds. Keep your movement gentle and smooth.
Repeat.

12. Standing heel raise
Using a counter or chair for support, get up on your tiptoes, together with your knees straight. Slowly lower your feet and backtrack. Repeat this 10 times.
13. Ankle out
Make a loop out of a bit of an elastic fitness band, and hold it in situ, either with the leg of a table or chair or together with your other foot. Place one foot in the loop. Keeping your heel fixed on the bottom, turn your toes outwards against the resistance of the band. Bring your foot back to the first position slowly. Increasing the repetition up to tolerance and repeating this 10 times, and doing the set 3 times a day.
14. Basic balance
Using a static object such as a kitchen edge for support, balance on one foot. Build up how long you are doing this for, aiming for one minute. Try to do this 3 times, and repeat the set twice each day.
Take any opportunities to practice standing on one leg – building it into your daily activities will facilitate your improvement.
When you feel confident with this basic balance exercise, you’ll make it harder by standing on a cushion or pillow. Build up the quantity you do slowly.
When you can easily balance on a pillow, and if you’re feeling confident, return to standing on the floor and repeat the basic balance exercise with your eyes closed.
15. Walking within the sand
This is best for strengthening your toes, feet, and calves. It is often tiring, so roll in the hay for 5 to 10 minutes at first, then increase the time as tolerated.
Walk barefoot in a place covered with sand, like a beach or sandbox.
16. Cold compress
Cold therapy can help to alleviate inflamed heel tissue. One option is to use a cloth-covered ice pack for your heel. you’ll also apply a cold compression pack to assist keep the ice pack in place. These are bought at many drugstores as gel packs or cold foot wraps. they’re kept in the freezer and then wrapped around the foot and ankle. Leave the wrap only for ten minutes at a time, then take it out. Repetition of the cold wrap application on an hourly basis while you’re awake. A different option is to roll your foot over a cold or frozen water bottle.
17. Shoes and orthotics
Comfortable and well-fitting shoes can reduce the quantity of pressure on the heel spur. This pressure can cause pain and discomfort. Here’s what to look for when choosing a shoe for comfort:
- Firm heel support: the rear “counter” of the shoe should be firm in order to assist the heel and stop your foot from rolling inward or outward.
- Moderate flexibility: A shoe shouldn’t be very easy to flex because it’s collapsible. However, the shoe should have a gradual bend that has some hardening when your foot is flexed or bent.
- Slightly elevated heel: A heel insert or shoe that features a slightly elevated heel (no more than 1 inch high) can help take pressure off your painful heel. You can also have custom orthotics (molded shoe inserts) made that will be put into your shoe. These orthotics are custom-designed to stop your foot from rolling and supply extra heel support. they’re made with a prescription from your podiatrist.
18. Cryoultrasound
Cryoultrasound therapy combines the appliance of electromagnetic energy and cold therapy to decrease aches. The machine seems like a large wand that is moved over the foot and ankle. Research has found that Cryoultrasound therapy is an efficient treatment solution trusted Source for people with plantar fasciitis who even have heel spurs. Podiatrists and physical therapists often give this therapy.
Surgery
Tophi removal surgery
Tophi can become painful and inflamed. they will even break open and drain or get infected. Your healthcare provider might recommend that they be surgically removed.
Joint fusion surgery
If advanced gout has permanently damaged a junction, your doctor might recommend that smaller junctions be fused together. This surgery can help increase joint stability and relieve pain.
Joint replacement surgery
To relieve aches and maintain movement, your doctor might recommend replacing a junction damaged by tophaceous gout with a man-made joint. The most familiar joint that is replaced due to damage from gout is the knee.
Takeaway
If you’re diagnosed with gout, take your drugs as prescribed by your doctor and make the lifestyle changes they recommend. These steps can assist to prevent your gout from advancing and requiring surgery.
Can I prevent gout?
You can make certain lifestyle changes to assist to prevent gout:
- Drink a lot of water to help your kidneys function better and avoid dehydration.
- Exercise regularly. Having overweight/obese increases acid in your body and puts more stress on your joints.
- Do your best to restrict the purines in your body, since these chemicals can aggravate acid buildup.
Foods and beverages containing high purine levels include:
- Alcohol.
- Red meat and organ meats.
- Shellfish.
- Gravy.
- Beverages and foods are high in fructose (fruit sugar).
- Protein from animal sources. All protein from animal flesh can potentially cause elevated uric acid levels.
Certain medications can cause elevated uric acid levels. These medications include:
Diuretics are also referred to as “water pills.”
Immunosuppressants, or drugs wont to slow the immune system (common in organ transplants, for example).
Gout home remedies
Some home remedies may help lower acid levels and prevent gout attacks. the subsequent foods and drinks have been suggested for gout:
- tart cherries
- magnesium
- ginger
- diluted apple vinegar
- celery
- nettle tea
- dandelion
- milk thistle seeds
FAQ
Is gout painful?
Yes, gout is often painful. In fact, pain within the big toe is often one of the first symptoms people report. The pain is amid more typical arthritis symptoms, like swelling and warmth in the joints. Gout pain can vary in severity. Pain within the big toe can be very intense at first. After the acute attack, it’s going to subside to a dull ache. The pain, also as swelling and other symptoms, are the result of the body launching a defense (by the immune system) against uric acid crystals in the joints. This attack results in the release of chemicals called cytokines, which promote painful inflammation.
A gout is a form of arthritis?
Gout may be a painful type of arthritis that develops when uric acid builds up in the body, resulting in the formation of uric acid crystals in the joints. The big toe is a common site affected by gout, but it also can affect other joints including the knees, ankles, heels, or toes. Affected joints are painful, red, swollen, and warm.
Uric acid is eliminated from the body through urine.
Uric acid is generally carried in the bloodstream and excreted in the urine. Uric acid is a product formed when substances known as purines are broken down. Purines are a piece of normal human tissues and are contained in numerous foods. If the kidneys don’t reach out enough uric acid from the body, blood levels of acid increase (known as hyperuricemia). Hyperuricemia can also be caused by the intake of foods rich in purines like liver, anchovies, dried beans, and gravies. Although hyperuricemia isn’t dangerous for the body, it sometimes results in the formation of uric acid crystals and the development of gout.
What are the three 3 complications of gout?
Complications of gout include junction damage, kidney damage, and bone loss. This excess acid causes syringe-shaped crystals to form around the junction,
leading to inflammation in and around the joints
During an acute gout attack what should I do and what drugs should I be taking?
Change your diet plan. Avoid the intake of red meats, shellfish, beer, wine, and salt. First, pain relievers like acetaminophen/Tylenol or other more potent analgesics are used to manage aches. Secondly, anti-inflammatory agents like nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and corticosteroids are wont to decrease joint inflammation.