Indomethacin
Introduction of Drug
Indometacin, also known as indomethacin, is a nonsteroidal anti-inflammatory drug commonly utilized as a prescription medication to relieve fever, pain, stiffness, and swelling from inflammation. It works by inhibiting the production of prostaglandins, endogenous signaling molecules learned to cause these symptoms.
- Boiling point: 499.4 °C
- Formula: C19H16ClNO4
- CASE ID: 53-86-1
- ChEMBL Id: 6
- ChemSpider ID: 3584
- IUPHAR ID: 1909
- Pronunciation: /ɪndoʊˈmɛtəsɪn/
Brand names
- Indocin®
- Tivorbex®
Ingredients
- Each tablet for oral administration contains 25 mg or 50 mg of indomethacin and the following fixed ingredients: lactose monohydrate, sodium lauryl sulfate, sodium starch glycolate, colloidal silicon dioxide, and magnesium stearate.
- Indomethacin Capsules, USP for oral administration are provided in two dosage strengths which include either 25 mg or 50 mg of indomethacin. Indomethacin is a non-steroidal anti-inflammatory indole product designated chemically as 1 (4 chlorobenzenes) 5 methoxy 2 methyl 1H indole 3 acetic acids.
- Indomethacin, USP is virtually insoluble in water and sparingly soluble in alcohol. It has a pKa of 4.5 and is stable in neutral or negligibly acidic media and decomposes in strong alkali.
- Each capsule for oral administration contains 25 mg or 50 mg of indomethacin and the following inactive ingredients: lactose monohydrate, sodium lauryl sulfate, sodium starch glycolate, colloidal silicon dioxide, and magnesium stearate. The hard gelatin cover consists of gelatin, titanium dioxide USP, FD & C Blue 1, D & C Yellow 10. The tablets are printed with ebony ink containing black iron oxide E172 dye.
Clinical Pharmacology of Drug
- Indomethacin is a non-steroidal anti-inflammatory drug (NSAID) that indicates antipyretic and analgesic properties. It is the method of action, like that of other anti-inflammatory drugs, is not comprehended. However, its therapeutic activity is not due to pituitary-adrenal stimulation.
- Indomethacin is a powerful inhibitor of prostaglandin synthesis in vitro. Concentrations are reached during treatment which has been demonstrated to have an impact in vivo as well. Prostaglandins sensitize afferent nerves and potentiate the movement of bradykinin inducing pain in animal models. Moreover, prostaglandins are comprehended to be among the mediators of inflammation. Since indomethacin is an inhibitor of prostaglandin synthesis, it is the method of action may also be due to a decrease in prostaglandins in peripheral tissues.
- Indomethacin is an effective anti-inflammatory agent, suitable for long-term benefit in rheumatoid arthritis, ankylosing spondylitis, and osteoarthritis. Indomethacin affords the alleviation of symptoms; it does not change the progressive course of the underlying disease.
- Indomethacin suppresses inflammation in rheumatoid arthritis as indicated by the relief of pain, and reduction of fever, swelling, and tenderness. Improvement in patients treated with indomethacin for rheumatoid arthritis has been demonstrated by a reduction in joint swelling, average number of joints involved, and morning stiffness; by improved mobility as demonstrated by a reduction in walking time; and by improved functional capability as demonstrated by an increase in grip strength. Indomethacin may also allow the deduction of steroid dosage in patients receiving steroids for the more powerful forms of rheumatoid arthritis. In such examples, the steroid dosage should be reduced slowly and the patients followed very near for any possible adverse effects.
- Indomethacin has been noted to diminish basal and CO2-stimulated cerebral blood flow in healthful volunteers following acute oral and intravenous administration. In one investigation, after one week of treatment with orally assisted indomethacin, this effect on basal cerebral blood flow disappeared. The clinical importance of this effect has not been proven. Indomethacin capsules have been found effective in relieving pain and reducing the fever, swelling, redness, and tenderness of acute gouty arthritis.
- Following single verbal doses of indomethacin capsules 25 mg or 50 mg, indomethacin is readily absorbed, achieving peak plasma concentrations of about 1 and 2 mcg/mL, respectively, at about 2 hours. Orally administered indomethacin tablets are virtually 100% bioavailable, with 90% of the dose absorbed within 4 hours. A single 50 mg dose of indomethacin oral suspension was found to be bioequivalent to a 50 mg indomethacin pill when each was administered with foodstuffs.
- Indomethacin is removed via renal excretion, metabolism, and/or biliary excretion. Indomethacin undergoes observable enterohepatic circulation. The mean half-life of indomethacin is evaluated to be about 4.5 hours. With a specific therapeutic regimen of 25 mg or 50 mg t.i.d., the steady-state plasma concentrations of indomethacin are standard of 1.4 times those observing the first dose.
- Indomethacin exists in the plasma as the parent drug and its desmethyl, des benzoyl, and desmethyl-des benzoyl metabolites, all in the unconjugated form. About 60 % of an oral dosage is recovered in urine as a drug and/or metabolites (26 % as indomethacin and its glucuronide), and 33 % is recuperated in feces (1.5 % as indomethacin).
- About 99% of indomethacin is bound to protein in plasma over the representative range of therapeutic plasma concentrations. Indomethacin has been found to cross the blood-brain border and the placenta.
Indications and usage
Carefully consider the potential advantages and risks of indomethacin capsules and other treatment options before choosing to operate indomethacin. Use the lower effective dose for the shortest duration consistent with particular patient treatment goals.
Indomethacin Capsule, USP has been discovered effective in active stages of the following:
- Moderate to extreme rheumatoid arthritis including acute flares of chronic disease.
- Moderate to severe ankylosing spondylitis.
- Moderate to severe osteoarthritis.
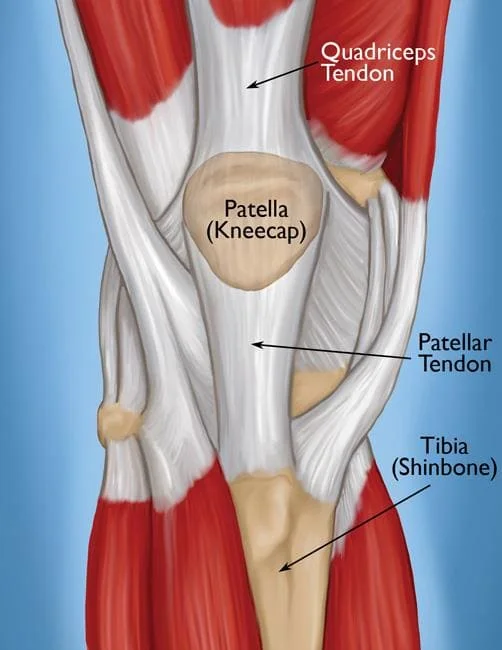
- Acute painful shoulder (bursitis and/or tendinitis).
- Acute gouty arthritis
Contraindications
Indomethacin Capsule, USP is contraindicated in patients with comprehended hypersensitivity to indomethacin or the excipients. Indomethacin Capsule, USP should not be given to patients who have undergone asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic or anaphylactoid reactions to non-steroidal anti-inflammatory drugs have been reported in such patients. Indomethacin Capsule, USP is contraindicated for the therapy of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery
Why is this medication prescribed?
Indomethacin is utilized to reduce moderate to severe pain, tenderness, swelling, and stiffness induced by osteoarthritis (arthritis forced by a breakdown of the lining of the joints), rheumatoid arthritis (arthritis caused by swelling of the lining of the joints), and ankylosing spondylitis (arthritis that mostly affects the spine). Indomethacin is also utilized to treat pain in the shoulder induced by bursitis (inflammation of a fluid-filled sac in the shoulder joint) and tendinitis (inflammation of the tissue that attaches muscle to bone). Indomethacin immediate-release capsules and suspension (liquid) are also utilized to treat acute gouty arthritis (attacks of severe joint pain and swelling caused by a build-up of certain importance in the joints). Indomethacin is in a variety of medications called NSAIDs. It works by stopping the body’s production of a meaning that causes pain, fever, and inflammation.
How should this medicine be used?
Indomethacin arrives as a capsule, an extended-release (long-acting) tablet, and a suspension to take by mouth. Indomethacin capsules and liquid usually are abode two to four times a day. Extended-release capsules are usually taken one or two periods a day. Indomethacin capsules, extended-release capsules, and suspension should be handled with food, instantly after meals, or with antacids. Take indomethacin at about the same times every day. Follow the suggestions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not comprehend. Accept indomethacin exactly as directed. Do not take additional or smaller of it or take it more often than prescribed by your doctor. Consume the extended-release capsules whole; do not separate, chew, or crush them. Vibrate the suspension agreeably before each use to mix the medication evenly.
Your doctor may also adjust the dose of your medication during your treatment. In some cases, your doctor may begin you on a low dose of indomethacin and gradually improve your dose, not more often than once a week. In other cases, your doctor may initiate you on an average dose of indomethacin and reduce your dose once your symptoms are controlled. Follow these suggestions carefully and ask your doctor or pharmacist if you have any questions.
Warnings of signs
Cardiovascular Effects
- Cardiovascular Thrombotic Events – Clinical difficulties of several COX-2 selective and nonselective NSAIDs of up to 3 years duration have shown an improved risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can also be fatal. All NSAIDs, both COX-2 selective and nonselective, may also have a comparable risk. Patients with known CV disease or risk factors for CV disease can also be at more significant risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose must be used for the fastest duration possible. Physicians and patients should stay awake for the development of such events, actually in the absence of previous CV symptoms. Patients should be advised about the signs and/or symptoms of serious CV events and the measures to take if they occur.
- There is no consistent proof that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic occasions associated with NSAID use. The concurrent use of aspirin and an NSAID does improve the risk of serious GI events. Two large, controlled, clinical trials of a COX-2 particular NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery discovered an increased incidence of myocardial infarction and stroke.
Hypertension
NSAIDs, including indomethacin, may also lead to the onset of new hypertension or the worsening of preexisting hypertension, either of which may contribute to the improved incidence of cardiovascular events. Patients taking thiazides or loop diuretics may also have impaired responses to these therapies when taking NSAIDs. the Non-steroidal anti-inflammatory drug, including indomethacin, should be employed with caution in patients with hypertension. Blood pressure (BP) should be monitored near during the initiation of NSAID treatment and throughout therapy.
Congestive Heart Failure and Edema
Fluid retention and edema have been observed in a few patients accepting NSAIDs. Indomethacin should be used with alert in patients with fluid retention or heart failure. In a study of patients with extreme heart failure and hyponatremia, indomethacin was associated with significant damage to circulatory hemodynamics, probably due to the inhibition of prostaglandin-dependent compensatory mechanisms.
Gastrointestinal Effects
- Risk of Ulceration, Bleeding, and Perforation – NSAIDs, including indomethacin, can cause serious gastrointestinal (GI) adverse occasions including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which may also be fatal. These extreme adverse circumstances can also occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a profound upper GI adverse event on NSAID therapy is symptomatic. Upper GI ulcers, gross bleeding, or perforation generated by NSAIDs occur in approximately 1% of patients feasted for 3 to 6 months, and in about 2 to 4% of patients treated for one year. These movements continue with a longer duration of service, increasing the likelihood of developing a serious GI event at some time during therapy. However, even short-term therapy is not without danger.
- Rarely, in patients bringing indomethacin, intestinal ulceration has been associated with stenosis and obstruction. Gastrointestinal bleeding without obvious ulcer appearance and perforation of preexisting sigmoid lesions (diverticulum, carcinoma, etc.) has happened. Increased abdominal pain in ulcerative colitis patients or the outcome of ulcerative colitis and regional ileitis have been reported to happen rarely.
- NSAIDs should be prescribed with extreme alert in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior record of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than the 10-fold heightened risk of developing a GI bleed compared to patients with neither of these risk factors. Other factors that raise the risk for GI bleeding in patients treated with NSAIDs possess concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and inadequate general health status. Most automatic information of fatal Gastrointestinal events is in elderly or debilitated patients and therefore, special care should be taken in treating this individual.
- To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lower effective dose should be utilized for the shortest possible duration. Patients and physicians should remain awake for signs and symptoms of gastrointestinal ulceration and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is supposed. This should contain discontinuation of the NSAID until a severe gastrointestinal adverse event is ruled out. For high-risk patients, alternate treatments that do not affect NSAIDs should be considered.
Renal Effects
Long-term management of NSAIDs has resulted in renal papillary necrosis and another renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory function in the maintenance of renal perfusion. In these patients, administration of a non-steroidal anti-inflammatory drug may also cause a dose-dependent decrease in prostaglandin formation and, secondarily, in renal blood flow, which may also precipitate over renal decompensation. Patients at greatest risk of this response are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, patients with volume depletion, and the aged. Discontinuation of Nonsteroidal anti-inflammatory drugs therapy is usually followed by recovery to the pretreatment situation.
Increases in serum potassium concentration, including hyperkalemia, have been registered with the use of indomethacin, actually in some patients without renal impairment. In patients with normal renal function, these results have been attributed to a hyporeninemic-hypoaldosteronism state.
Advanced Renal Disease
No knowledge is available from controlled clinical studies regarding the use of indomethacin in patients with advanced renal disease. Thus, treatment with indomethacin is not suggested in these patients with advanced renal disease. If indomethacin therapy must be initiated, close monitoring of the patient’s renal process is advisable.
Anaphylactic / Anaphylactoid Reactions
As with different NSAIDs, anaphylactic or anaphylactoid reactions may also occur in patients without known prior disclosure of indomethacin. Indomethacin should not be given to patients with the aspirin trio. This symptom complex generally happens in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit extreme, potentially fatal bronchospasm after taking aspirin or additional NSAIDs. Emergency assistance should be sought in cases where an anaphylactic or anaphylactoid response occurs.
Skin Reactions
Nonsteroidal anti-inflammatory drugs, including indomethacin, can also cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may happen without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first impression of skin rash or any other sign of hypersensitivity.
Pregnancy
In belated pregnancy, as with other NSAIDs, indomethacin should be bypassed because it may cause premature closure of the ductus arteriosus.
Ocular Effects
Corneal deposits and retinal disturbances, including those of the macula, have been marked in some patients who had received prolonged therapy with indomethacin. The prescribing physician should be aware of the possible association between the changes noted and indomethacin. It is advisable to stop therapy if such changes are observed. Blurred vision may also be a significant symptom and warrants a thorough ophthalmological examination. Since these modifications may be asymptomatic, ophthalmologic examination at periodic intervals is seductive in patients where therapy is prolonged.
Central Nervous System Effects
Indomethacin may also aggravate depression or other psychiatric disturbances, epilepsy, and parkinsonism, and should be used with significant caution in patients with these conditions. If severe CNS adverse reactions form, indomethacin should be discontinued.
Indomethacin may induce drowsiness; therefore, patients should be cautioned about engaging in activities demanding mental alertness and motor coordination, such as driving a car. Indomethacin may also induce headaches. Headache which continues despite dosage reduction demands cessation of therapy with indomethacin.
Mechanism of action
- Indometacin is a nonspecific and reversible inhibitor of the cyclo-oxygenase (COX) enzyme and/or prostaglandin G/H synthase. There are two recognized isoforms of COX: COX-1 is universally present in most body tissues and is involved in the synthesis of prostaglandins and thromboxane A2, while COX-2 is expressed in reaction to injury or inflammation. Constitutively expressed, the COX-1 enzyme is implicated in gastric mucosal protection, platelet, and kidney function by catalyzing the conversion of arachidonic acid to prostaglandin (PG) G2 and PGG2 to PGH2. COX-2 is constitutively expressed and positively inducible by inflammatory stimuli. It is discovered in the central nervous system, kidneys, uterus, and other organs. COX-2 also catalyzes the transformation of arachidonic acid to PGG2 and PGG2 to PGH2.
- In the COX-2-mediated pathway, PGH2 is converted to PGE2 and PGI2 (also known as prostacyclin). PGE2 is involved in mediating inflammation, ache, and fever. Decreasing levels of PGE2 leads to decreased inflammatory reactions. Indometacin is known to inhibit both isoforms of COX, however, with more excellent selectivity for COX-1, which accounts for its raised adverse gastric effects relative to other NSAIDs. It attaches to the enzyme’s active site and prevents the interaction between the enzyme and its substrate, arachidonic acid. Indometacin, unlike other NSAIDs, also inhibits phospholipase A2, the enzyme responsible for terminating arachidonic acid from phospholipids. The analgesic, antipyretic, and anti-inflammatory results of indomethacin and adverse reactions associated with the drug result from reduced prostaglandin synthesis. Its antipyretic effects may be due to action on the hypothalamus, resulting in enhanced peripheral blood flow, vasodilation, and subsequent heat dissipation.
- The exact mechanism of action of indomethacin in effecting the closure of a patent ductus arteriosus is not fully understood; yet, it is thought to be through inhibition of prostaglandin synthesis. At birth, the ductus arteriosus is generally closed as the tension of the oxygen increases significantly after birth. Patent ductus arteriosus in premature infants is associated with congenital heart malformations where PGE1 moderates an opposite effect to that of oxygen. PGE1 dilates the ductus arteriosus through smooth muscle relaxation and controls the closure of the ductus arteriosus. By inhibiting the synthesis of prostaglandins, indometacin announces the closure of the ductus arteriosus.
- Indometacin has been described as possessing anticancer and antiviral properties via the activation of protein kinase R (PKR) and/or downstream phosphorylation of eIF2α, inhibiting protein synthesis.
Absorption
- Indometacin offers an unbent pharmacokinetics shape where the plasma concentrations and/or area under the curve (AUC) are dose-proportional, whereas half-life (T1/2) and plasma and renal clearance are dose-dependent. Indometacin is readily and/or rapidly absorbed from the gastrointestinal tract. The bioavailability is virtually 100% following oral administration and about 90% of the dose is absorbed within 4 hours. The bioavailability is about 80 to 90% following rectal administration.
- The peak plasma concentrations pursuing a single oral dose were achieved between 0.9 ± 0.4 and 1.5 ± 0.8 hours in fasting possibilities. Despite large intersubject variation as agreeably utilizing the same preparation, peak plasma concentrations are dose-proportional and averaged 1.54 ± 0.76 μg/mL, 2.65 ± 1.03 μg/mL, and 4.92 ± 1.88 μg/mL following 25 mg, 50 mg, and 75 mg single doses in fasting matters, respectively. With a characteristic therapeutic regimen of 25 or 50 mg t.i.d., the steady-state plasma concentrations of indomethacin are standard of 1.4 times those pursuing the foremost dose.
Volume of distribution
The volume of distribution varied from 0.34 to 1.57 L/kg following oral, intravenous, or rectal administration of single and multiple doses of indomethacin in healthy individuals. Indometacin is disseminated into the synovial fluid and is extensively attached to tissues. It has been identified in human breast milk and/or the placenta. Although indomethacin has been shown to cross the blood-brain barrier (BBB), its comprehensive plasma protein binding allows only a small fraction of free or unbound indometacin to diffuse across the blood-brain barrier.
Protein binding
Indometacin is a weak organic acid that is 90 to 99% bound to protein in plasma over the expected range of therapeutic plasma concentrations. Like other NSAIDs, indomethacin is bound to plasma albumin but it does not attach to red blood cells.
Metabolism
Indometacin experiences hepatic metabolism involving glucuronidation, O-desmethylation, and N-deacylation. O-desmethyl-indomethacin, N-deschlorobenzoyl-indomethacin, and O-desmethyl-N-deschlorobenzoyl-indomethacin metabolites and their glucuronides are primarily passive and have no pharmacological activity. Unconjugated metabolites are also exposed in the plasma. It is increased bioavailability indicates that indometacin is improbable to be subject to first-pass metabolism.
Route of elimination
Indometacin is eliminated through renal excretion, metabolism, and biliary excretion. It is also subject to enter the enterohepatic circulation through the excretion of its glucuronide metabolites into bile pursued by resorption of indometacin after hydrolysis. The breadth of involvement in the enterohepatic circulation ranges from 27 to 115%.
Approximately 60 percent of a verbal dosage is recovered in urine as a drug and metabolites (26 percent as indomethacin and its glucuronide), and/or 33 percent in the feces (1.5 percent as indomethacin).
Half-life
Indometacin personality from the plasma is noted to be biphasic, with a half-life of 1 hour during the initial stage and 2.6 to 11.2 hours during the second phase. Interindividual and intraindividual variations are feasible due to the extensive and sporadic nature of the enterohepatic recycling and biliary discharge of the drug.
The mean half-life of oral indomethacin is calculated to be about 4.5 hours. The disposition of intravenous indomethacin in preterm neonates was shown to run across premature infants. In neonates older than 7 days, the mean plasma half-life of intravenous indomethacin was about 20 hours, ranging from 15 hours in infants weighing more than 1000 g and 21 hours in infants considering less than 1000 g.
Clearance
In a clinical pharmacokinetic study, the plasma discharge of indometacin was conveyed to range from 1 to 2.5 mL/kg/min following oral administration.
Precautions of Drug
General Precautions
Indomethacin cannot be expected to substitute for corticosteroids or to feast corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may also conduct to disease exacerbation. Patients on lengthy corticosteroid therapy should have their therapy tapered gradually if a decision is made to stop corticosteroids.
The pharmacological action of indomethacin in reducing fever and inflammation may also diminish the utility of these diagnostic signs in seeing complications of presumed noninfectious, painful conditions.
Hepatic Effects
Borderline heights of one or more liver tests may appear in up to 15% of patients taking NSAIDs, including indomethacin. These laboratory abnormalities may move, may remain unchanged, or may be transient with continuing therapy. Notable peaks of ALT or AST (about three or more times the upper limit of normal) have been reported in approximately 1% of patients with clinical problems with NSAIDs. In addition, rare cases of extreme hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis, and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs indicating liver dysfunction, or in whom an abnormal liver test value has occurred, should be considered for evidence of the development of a more severe hepatic reaction while on therapy with indomethacin. If clinical signs and symptoms compatible with liver disease develop, or if systemic manifestations surface (e.g., eosinophilia, rash, etc.), indomethacin should be discontinued.
Hematological Effects
Anemia is sometimes seen in patients acquiring NSAIDs, including indomethacin. This may also be due to fluid retention, occult or gross Gastrointestinal blood loss, or an incompletely expressed effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including indomethacin, should have their hemoglobin or hematocrit prevented if they exhibit any signs or symptoms of anemia.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in a few patients. Unlike aspirin, their effect on platelet function is quantitatively smaller, of shorter duration, and reversible. Patients receiving indomethacin who can also be adversely affected by alterations in platelet function, such as those with coagulation conditions or patients acquiring anticoagulants, should be carefully monitored.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The benefit of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross-reactivity, including bronchospasm, between aspirin and other non-steroidal anti-inflammatory drugs, has been documented in such aspirin-sensitive patients, indomethacin should not be administered to patients with this form of aspirin sensitivity and should be used with cautiousness in patients with preexisting asthma.
Information for Patients
Patients should be informed of the following details before initiating therapy with an NSAID and periodically during continuous therapy. Patients should also be motivated to read the NSAID Medication Guide that attends each prescription dispensed.
- Indomethacin, like other NSAIDs, may also cause serious CV side effects, such as MI or stroke, which may also result in hospitalization and even death. Although severe CV occasions can also occur without warning symptoms, patients should be alert for the signs and symptoms of chest pain, shortness of breath, weakness, and slurring of speech, and should request medical advice when observing any indicative signs or symptoms. Patients should be apprised of the extent of this follow-up
- Indomethacin, like other Nonsteroidal anti-inflammatory drugs, can also cause gastrointestinal discomfort and, rarely, serious gastrointestinal side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious Gastrointestinal tract ulcerations and bleeding can occur without warning symptoms, patients should be awake for the signs and symptoms of ulcerations and bleeding and should ask for medical advice when attending to any signifying signs or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the significance of this follow-up.
- Indomethacin, like other NSAIDs, can cause severe skin adverse effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalizations and even death. Although severe skin reactions may happen without warning, patients should be awake for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and should ask for medical advice when attending to any indicative signs or symptoms. Patients should be advised to stop the drug instantly if they develop any rash and contact their physicians as soon as possible.
- Patients should promptly inform their signs or symptoms of unexplained weight gain or edema to their physicians.
- Patients should be informed of the notice signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and “flu-like” symptoms). Patients should be instructed to stop treatment and seek immediate medical therapy if these occur.
- Patients should be informed of the signs of an anaphylactic or anaphylactoid response (e.g. problem breathing, swelling of the face and/or throat). If these happen, patients should be instructed to seek immediate emergency assistance.
- In late pregnancy, as with other NSAIDs, indomethacin should be bypassed because it may cause premature closure of the ductus arteriosus.
Drug Interactions
ACE Inhibitors and Angiotensin II Antagonists
The statement indicates that NSAIDs may also diminish the antihypertensive effect of ACE inhibitors and angiotensin II antagonists. Indomethacin can decrease the antihypertensive effects of captopril and losartan. These interactions should be considered in patients taking NSAIDs concomitantly with ACE inhibitors and/or angiotensin II antagonists. In a few patients with compromised renal function, the coadministration of an NSAID and an ACE inhibitor or an angiotensin II antagonist can also result in additional deterioration of renal function, including potential acute renal defeat, which is usually reversible.
Aspirin
When indomethacin is administered with aspirin, its protein binding is reduced, although the release of free indomethacin is not altered. The clinical significance of this interchange is not known.
The utilization of indomethacin in conjunction with aspirin or additional salicylates is not recommended. Controlled clinical examination has shown that the integrated benefit of indomethacin and aspirin does not beget any greater therapeutic effect than the use of indomethacin independently. In a clinical study of the combined benefit of indomethacin and aspirin, the incidence of gastrointestinal side effects was significantly increased with combined therapy.
In a breakdown in normal volunteers, it was found that chronic concurrent administration of 3.6 g of aspirin per day reduces indomethacin blood levels by approximately 20%.
Beta-Adrenoceptor Blocking Agents
Blunting of the antihypertensive effect of beta-adrenoceptor blocking agents by non-steroidal anti-inflammatory medications including indomethacin has been reported. Therefore, when using these blocking agents to treat hypertension, patients should be observed to confirm that the desired therapeutic effect has been obtained.
Cyclosporin
Administration of non-steroidal anti-inflammatory drugs concomitantly with cyclosporine has been associated with an expansion in cyclosporine-induced toxicity, possibly due to reduced synthesis of renal prostacyclin. NSAIDs should be employed with caution in patients taking cyclosporine, and renal function should be carefully monitored.
Diflunisal
In normal volunteers welcoming indomethacin, the administration of diflunisal reduced renal clearance and significantly increased the plasma levels of indomethacin. In a few patients, combined usage of indomethacin and diflunisal has been associated with fatal gastrointestinal hemorrhage. Therefore, diflunisal and indomethacin should not be utilized concomitantly.
Digoxin
Indomethacin delivered concomitantly with digoxin has been reported to improve the serum concentration and prolong the half-life of digoxin. Therefore, when indomethacin and digoxin are utilized concomitantly, serum digoxin levels should be closely monitored.
Diuretics
In a few patients, the administration of indomethacin can also diminish the diuretic, natriuretic, and antihypertensive effects of loop, potassium-sparing, and/or thiazide diuretics. This response has been attributed to the inhibition of renal prostaglandin synthesis. Indomethacin decreases basal plasma renin activity (PRA), as well as those elevations of PRA caused by furosemide administration, or salt or volume depletion. These facts should be considered when considering plasma renin activity in hypertensive patients.
It has been reported that the addition of triamterene to a supervision schedule of indomethacin resulted in reversible acute renal failure in two of four wholesome volunteers. Indomethacin and/or triamterene should not be administered concurrently.
Indomethacin and potassium-sparing diuretics may also be associated with improved serum potassium levels. The possible developments of indomethacin and potassium-sparing diuretics on potassium kinetics and renal function should be considered when these agents are administered together. Most of the overhead effects involving diuretics have been attributed, at least in part, to mechanisms regarding the inhibition of prostaglandin synthesis by indomethacin. During concomitant therapy with NSAIDs, the patient should be monitored near for signs of renal failure), as well as to assure diuretic efficacy.
Lithium
Indomethacin capsules 50 mg t.i.d. produced a clinically appropriate elevation of plasma lithium and a reduction in renal lithium consent in psychiatric patients and normal subjects with steady-state plasma lithium attention. This development has been attributed to the inhibition of prostaglandin synthesis. As a consequence, when nonsteroidal anti-inflammatory drugs and lithium are given concomitantly, the patient should be carefully scrutinized for signs of lithium toxicity. (Read brochures for lithium preparations before use of such concomitant therapy.) In expansion, the frequency of monitoring serum lithium concentration should be increased at the outset of such combination drug therapy.
Methotrexate
Nonsteroidal anti-inflammatory pills have been reported to inhibit methotrexate accumulation in rabbit kidney slices competitively. This may also suggest that they could enhance the toxicity of methotrexate. Caution should be used when nonsteroidal anti-inflammatory drugs are dispersed concomitantly with methotrexate.
NSAIDs
The concomitant use of indomethacin with other NSAIDs is not recommended due to the improved possibility of gastrointestinal toxicity, with little or no accumulation in efficacy.
Oral anticoagulants
Clinical investigations have shown that indomethacin does not influence the hypoprothrombinemia anticoagulants to create. Yet, when any additional drug, including indomethacin, is added to the therapy of patients on anticoagulant therapy, the patients should be observed for alterations of the prothrombin time. In post-marketing experience, bleeding has been documented in patients on concomitant treatment with anticoagulants and indomethacin. Carefulness should be employed when indomethacin and anticoagulants are administered concomitantly. The results of warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs concurrently have a higher risk of serious GI bleeding than users of either medication alone.
Probenecid
When indomethacin is given to patients acquiring probenecid, the plasma levels of indomethacin are likely to be improved. Therefore, a more down total daily dosage of indomethacin may also produce a satisfactory therapeutic effect. When increases in the amount of indomethacin are made, they should be made carefully and in remote increments.
Drug & or Laboratory Test Interactions
False-negative products in the dexamethasone suppression test (DST) in patients being treated with indomethacin contain been reported. Thus, the results of the DST should be interpreted with a warning in these patients.
Laboratory Tests – Because serious GI tract ulcerations and bleeding can also happen without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term therapy with nonsteroidal anti-inflammatory drugs should have their CBC and chemistry profile checked periodically. If clinical signs and symptoms compatible with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if irregular liver tests persist or worsen, indomethacin should be discontinued.
Carcinogenesis & Mutagenesis & Impairment Of Fertility
In an 81-week chronic oral toxicity analysis in the rat at doses up to 1 mg/kg/day, indomethacin had no tumorigenic effect. Indomethacin produced no neoplastic or hyperplastic changes related to therapy in carcinogenic studies in the rat (dosing period 73 to 110 weeks) and the mouse (dosing period 62 to 88 weeks) at quantities up to 1.5 mg/kg/day. Indomethacin did not have any mutagenic development in vitro bacterial tests (Ames test and E. coli with or without metabolic activation) and a series of in vivo tests including the host-mediated assay, sex-linked recessive lethal in Drosophila, and the micronucleus test in mice. Indomethacin at dosage levels up to 0.5 mg/kg/day did not affect fertility in mice in a two-generation reproduction study or a two-litter reproduction study in rats.
pregnancy
Teratogenic Effects. Pregnancy Category C – Teratogenic analyses were conducted in mice and rats at dosages of 0.5, 1, 2, and 4 mg/kg/day. Except for retarded fetal ossification at 4 mg/kg/day deemed secondary to the decreased average fetal weights, no growth in fetal malformations was observed as compared with control groups. Other investigations in mice reported in the literature using higher doses (5 to 15 mg/kg/day) have expressed maternal toxicity and death, increased fetal resorptions, and fetal malformations. Comparable investigations in rodents utilizing high doses of aspirin have shown similar maternal and fetal effects. However, animal reproduction analyses are not always predictive of human response. There are no sufficient and well-controlled investigations on pregnant women. Indomethacin should be engaged during pregnancy only if the potential benefit explains the potential threat to the fetus.
Nonteratogenic Effects
Because of the learned effects of non-steroidal anti-inflammatory drugs on the fetal cardiovascular system (closure of ductus arteriosus), use during pregnancy (particularly late pregnancy) should be avoided.
The known effects of indomethacin and other drugs of this category on the human fetus during the third trimester of pregnancy contain constriction of the ductus arteriosus prenatally, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus postnatally which may also be resistant to medical management; myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or failure, renal injury or dysgenesis which can also result in prolonged or permanent renal failure, oligohydramnios, gastrointestinal bleeding or perforation, and increased risk of necrotizing enterocolitis.
In rats and mice, 4 mg/kg/day given during the last 3 days of gestation caused a reduction in maternal weight gain and some maternal and fetal deaths. An enhanced incidence of neuronal necrosis in the diencephalon in the live-born fetuses was noted. At 2 mg/kg/day, no accumulation in neuronal necrosis was observed as compared to the control groups. Administration of 0.5 or 4 mg/kg/day during the first 3 days of life did not cause an expansion in neuronal necrosis at either dose level.
Labor & Delivery
In rat investigations with NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, an improved incidence of dystocia, delayed parturition, and reduced pup survival occurred. The effects of indomethacin on labor and delivery in pregnant women are unfamiliar.
Nursing Mothers – Indomethacin is excreted in the milk of lactating mommies. Indomethacin is not recommended for service in nursing mothers.
Pediatric Use – Safety and effectiveness in pediatric patients 14 years to years and younger have not been established.
Indomethacin should not be specified for pediatric patients 14 years of age and younger unless toxicity or lack of effectiveness associated with other drugs warrants the risk. In experience with more than 900 pediatric patients documented in the literature or to the manufacturer who was treated with indomethacin capsules, side effects in pediatric patients were identical to those reported in adults. Experience in pediatric patients has been confined to the service of indomethacin capsules.
If a determination is made to use indomethacin for pediatric patients 2 years of age or more aged, such patients should be monitored closely and periodic assessment of liver function is recommended. There have been problems of hepatotoxicity reported in pediatric patients with juvenile rheumatoid arthritis, including fatalities. If indomethacin treatment is instituted, a recommended starting dose is 1 to 2 mg/kg/day given in divided doses. Maximum daily dosage should not surpass 3 mg/kg/day or 150 to 200 mg/day, whichever is less. Limited data are available to support the benefit of a maximum daily dosage of 4 mg/kg/day or 150 to 200 mg/day, whichever is smaller. As symptoms subside, the total daily dosage should be reduced to the most inferior level required to control symptoms, or the drug should be discontinued.
Geriatric Use
As with any Nonsteroidal anti-inflammatory drugs, caution should be exercised in treating the elderly (65 years and older) since advancing age appears to increase the possibility of adverse reactions. Elderly patients seem to tolerate ulceration and/or bleeding less well than other individuals and many spontaneous reports of fatal gastrointestinal events are in this population. Indomethacin may also confuse or, rarely, psychosis; physicians should remain alert to the possibility of such adverse effects in the elderly.
This drug is known to be substantially eliminated by the kidney and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because geriatric patients are more likely to have decreased renal function, care should be taken in dose selection and it may be helpful to observe renal function.
Adverse Reactions to Drug
The adverse reactions for indomethacin capsules documented in the following table have been arranged into two classes: (1) incidence more splendid than 1%; and (2) incidence more undersized than 1%. The incidence for group (1) was obtained from 33 double-blind collected clinical trials registered in the literature (1,092 patients). The incidence for group (2) was based on notification from clinical difficulties, in the literature, and on voluntary reports since marketing. The possibility of a causal relationship lives between indomethacin and these adverse reactions, some of which have been reported only rarely. Incidences greater than 1%
- Gastrointestinal – nausea1 with or without vomiting, dyspepsia1 (including indigestion, heartburn, and epigastric pain), diarrhea, abdominal distress or pain, constipation
- Central nervous system – headache (11.7%), dizziness1, vertigo, somnolence, depression, and fatigue (including malaise and listlessness)
- Special sense – tinnitus
- Cardiovascular – none
- Metabolic – none
- Integumentary – none
- Hematologic – none
- Hypersensitivity – none
- Genitourinary – none
- Miscellaneous – none
Reactions happening in 3% to 9% of patients regaled with indomethacin. (Those reactions occurring in less than 3% of the patients are unmarked.) Incidence less than 1%
GASTROINTESTINAL
- anorexia, bloating (includes distention)
- flatulence, peptic ulcer
- gastroenteritis, rectal bleeding, proctitis
- single and/or multiple ulcerations, including perforation and hemorrhage of the esophagus, stomach, duodenum, or small and large intestines
- intestinal ulceration associated with stenosis and obstacle gastrointestinal bleeding without obvious ulcer formation and perforation of preexisting sigmoid lesions (diverticulum, carcinoma, etc.) development of ulcerative colitis and provincial ileitis
- ulcerative stomatitis
- toxic hepatitis and jaundice (A few fatal cases have been reported)
- intestinal strictures (diaphragms)
CENTRAL NERVOUS SYSTEM
- anxiety (includes nervousness), muscle weakness
- involuntary muscle movements
- insomnia, muzziness
- psychic disturbances including psychotic episodes
- mental confusion
- drowsiness
- light-headedness
- syncope
- paresthesia
- aggravation of epilepsy and parkinsonism
- depersonalization
- coma
- peripheral neuropathy
- convulsions
- dysarthria
SPECIAL SENSES
- ocular-corneal deposits and retinal disorders, including those of the macula, have been reported in a few patients on prolonged therapy with indomethacin
- blurred vision
- diplopia
- hearing disturbances, deafness
CARDIOVASCULAR
- congestive heart failure
- hypertension
- hypotension
- tachycardia
- chest pain
- arrhythmia; palpitations
METABOLIC
- edema
- weight gain
- fluid retention
- flushing or sweating
- hyperglycemia
- glycosuria
- hyperkalemia
INTEGUMENTARY
- pruritus
- rash; urticaria
- petechiae or ecchymosis
- exfoliative dermatitis
- erythema nodosum
- loss of hair
- Stevens-Johnson Syndrome
- erythema multiforme
- toxic epidermal necrolysis
HEMATOLOGIC
- leukopenia
- bone marrow depression
- anemia secondary to apparent or occult gastrointestinal bleeding
- aplastic anemia
- hemolytic anemia
- agranulocytosis
- thrombocytopenic purpura
- disseminated intravascular coagulation
HYPERSENSITIVITY
- acute anaphylaxis
- acute respiratory distress
- the rapid drop in blood pressure resembling a shock-like state
- angioedema
- dyspnea
- asthma
- purpura
- angiitis
- pulmonary edema
- fever
GENITOURINARY
- hematuria
- vaginal bleeding
- proteinuria, nephrotic syndrome, interstitial nephritis
- BUN elevation
- renal insufficiency, including renal failure
MISCELLANEOUS
- epistaxis
- breast changes, including enlargement and tenderness, or gynecomastia
Causal Relationship Unknown
Other reactions have been registered but occurred under circumstances where a causal relationship could not be established. Although, in these seldom reported events, the possibility cannot be excluded. Thus, these observations are being listed to serve as alerting details to physicians:
Cardiovascular: thrombophlebitis
Hematologic: Although there have been several commentaries on leukemia, the supporting information is weak.
Genitourinary: urinary frequency
An occasional occurrence of fulminant necrotizing fasciitis, particularly in association with Group A β-hemolytic streptococcus, has been described in persons regaled with non-steroidal anti-inflammatory agents, including indomethacin, sometimes with fatal consequences.
Dosage and Administration
- Carefully assess the potential benefits and risks of indomethacin and other treatment alternatives before deciding to use indomethacin. Use the lowest efficacious dose for the shortest duration consistent with individual patient therapy goals.
- After watching the response to initial therapy with indomethacin, the dose, and frequency should be adjusted to suit an individual patient’s requirements.
- Indomethacin is obtainable in 25 mg and 50 mg capsules.
- Adverse reactions seem to connect with the size of the dose of indomethacin in most patients but not all. Therefore, every effort should be made to resolve the smallest effective dosage for the individual patient.
Pediatric Use – Indomethacin ordinarily should not be defined for pediatric patients 14 years of age and under.
Adult Use
Dosage Advice for Active Stages of the Following:
Moderate to extreme rheumatoid arthritis including acute flares of a chronic condition; moderate to severe ankylosing spondylitis; and moderate to severe osteoarthritis.
- Suggested Dosage: Indomethacin capsules 25 mg b.i.d. or t.i.d. If this is well tolerated, raise the daily dosage by 25 mg or by 50 mg, if needed by continuing symptoms, at weekly intervals until a satisfactory answer is obtained or until a total everyday dose of 150 mg to 200 mg is reached. Doses above this amount normally do not increase the effectiveness of the drug.
- In patients who have persistent nighttime pain and/or morning stiffness, the giving of a large amount, up to a maximum of 100 mg, of the total daily dose at bedtime may also help afford relief. The total daily dose should not transcend 200 mg. In acute outbursts of chronic rheumatoid arthritis, increasing the dosage by 25 mg or, if needed, by 50 mg daily may also be necessary.
- If minor adverse outcomes materialize as the dosage is increased, decrease the dosage rapidly to a tolerated dose and observe the patient closely.
- If severe adverse reactions occur, STOP THE DRUG. After the acute stage of the disease is under control, an endeavor to reduce the daily dose should be made repeatedly until the patient is receiving the smallest effective amount or the drug is discontinued.
- Careful teachings to, and observations of, the individual patient are important to the prevention of serious, irreversible, including fatal, adverse reactions.
- As advancing years seem to increase the possibility of adverse responses, indomethacin should be used with greater care in the aged.
Acute painful shoulder (bursitis and tendinitis).
- Initial Dose: 75 mg to 150 mg every day in 3 or 4 divided doses. The drug should be discontinued after the signs and symptoms of hives have been controlled for several days. The standard practice of therapy is 7 to 14 days
Acute gouty arthritis.
- Suggested Dosage: Indomethacin capsules 50 mg t.i.d. until the pain is tolerable. The dose should then be rapidly reduced to a comprehensive cessation of the drug. Definite alleviation of pain has been reported within 2 to 4 hours. Tenderness and heat usually subside in 24 to 36 hours, and swelling slowly disappears in 3 to 5 days.
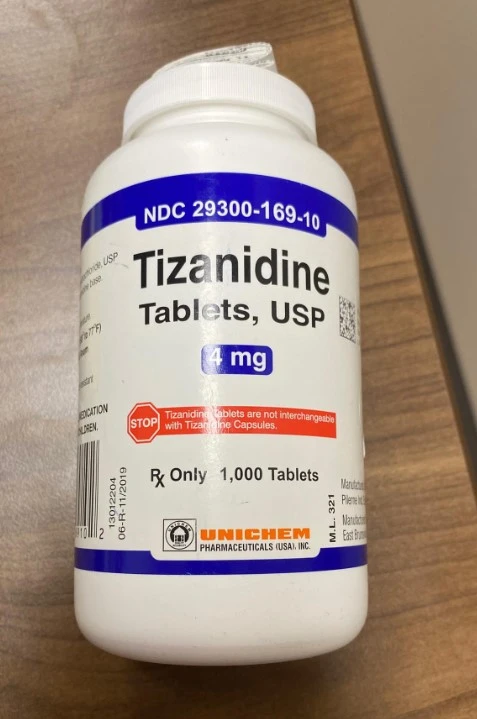
How supplied
Indomethacin Tablets, USP are available containing either 25 mg or 50 mg of Indomethacin, USP. The 25 mg capsules are size ‘3’ hard gelatin capsules, with an opaque light green cap imprinted with ‘H’ and opaque light green body imprinted with ‘103’, containing white to off-white powder.
- Bottles of 30 capsules NDC 65977-5042-0
- Bottles of 100 capsules NDC 65977-5042-1
- Bottles of 500 capsules NDC 65977-5042-2
- Bottles of 1000 capsules NDC 65977-5042-3
The 50 mg capsules are size ‘1’ hard gelatin capsules, with opaque light green caps imprinted with ‘H’ and opaque light green body imprinted with ‘104’, containing white to off-white powder.
- Bottles of 30 capsules NDC 65977-5043-0
- Bottles of 100 capsules NDC 65977-5043-1
- Bottles of 500 capsules NDC 65977-5043-2
- Bottles of 1000 capsules NDC 65977-5043-3
- Store at 20° to 25°C (68° to 77°F) [see USP Maintained Room Temperature].
- Protect from light.
- Dispense in a tight, light-resistant receptacle as defined in the USP operating a child-resistant closure.
- PHARMACIST: Dispense a Medication Guide with each prescription.
- SPL med guide
INDOMETHACIN CAPSULES USP
Medication Guide for Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). (See the end of this Medication Directory for a list of prescription NSAID medicines.)
What is the most important information I should know about prescriptions called Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAID medicines may also improve the chance of a heart attack and/or stroke which can also lead to death. This chance increases:
- with longer usage of NSAID medicines
- In someone who has heart disease
NSAID medications should never be utilized right before or after a heart surgery called a “coronary artery bypass graft (CABG).” NSAID medicines can also cause ulcers and bleeding in the stomach and intestines at any time during therapy.
Ulcers and bleeding:
- can happen without warning symptoms
- may cause death
The chance of an individual getting an ulcer or bleeding increases with:
- carrying medicines called “corticosteroids” and “anticoagulants”
- longer use
- smoking
- drinking alcohol
- older age
- having poor health
NSAID medicines should only be used:
- exactly as prescribed
- at the lowest dose feasible for your treatment
- for the shortest time needed
What are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAID medicines are used to feast pain and redness, swelling, and heat (inflammation) from medical conditions such as:
- different types of arthritis
- menstrual cramps and other kinds of short-term pain
Who should not accept a Non-Steroidal Anti-Inflammatory Drug (NSAID)?
Do not take an NSAID medicine:
- if you had an asthma attack, hives, or other allergic reaction to aspirin or any other NSAID medicine
- for aches right before or after heart bypass surgery
Tell your healthcare provider:
- about all of your medical requirements.
- about all of the medications you take. NSAIDs and some other medicines may also interact with each other and cause serious side effects. Keep a list of your medications to show to your healthcare provider and pharmacist.
- if you are pregnant. NSAID medicines should not be used by pregnant women delinquent in their pregnancy.
- if you are breastfeeding. Talk to your doctor.
What are the potential side effects of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)?
serious side effects include:
- heart attack
- stroke
- high blood pressure
- heart failure from body swelling (liquid Retension)
- kidney problems including kidney failure
- bleeding and ulcers in the stomach and/or intestine
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
- liver problems including liver failure
- asthma attacks in individuals who have asthma
Other side effects include:
- stomach pain
- constipation
- diarrhea
- gas
- heartburn
- nausea
- vomiting
- dizziness
Get emergency assistance right away if you have any of the following symptoms:
- shortness of breath or difficulty breathing
- chest pain
- weakness in one portion or side of your body
- slurred speech
- swelling of the face and/or throat
Control your NSAID medicine and call your healthcare provider right away if you have any of the following symptoms:
- nausea
- more tired or weaker than expected
- itching
- your skin and/or eyes look yellow
- stomach
- flu-like symptoms
- vomit blood
- there is blood in your bowel motion or it is black and sticky like
- unusual weight gain
- skin inflammation or blisters with fever
- swelling of the arms and legs, hands and/or feet
These are not all the side effects of NSAID medicines. Talk with your healthcare provider and/or pharmacist for more details about NSAID medicines. Contact your doctor for medical recommendations about side effects. You may report side products to FDA.
Other information about Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) – Aspirin is an NSAID medicine but it does not improve the chance of a heart attack. Aspirin may also cause bleeding in the brain, stomach, and intestines. Aspirin can also induce ulcers in the stomach and intestines. Some of these NSAID medications are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before utilizing over-the-counter NSAIDs for more than 10 days.
NSAID medicines that require a prescription – Generic Name
Celecoxib, Diclofenac, Diflunisal, Etodolac, Fenoprofen, Flurbiprofen, Ibuprofen, Indomethacin, Ketoprofen, Ketorolac, Mefenamic Acid, Meloxicam, Nabumeton, Naproxen, Oxaprozin, Piroxicam, Sulindac, Tolmetin
Trade name: Celebrex, Cataflam, Voltaren, Arthrotec (combined with misoprostol, Dolobid, Lodine, Lodine XL, Nalfon, Nalfon 200, Ansaid, Motrin, Tab-Profen, Vicoprofen*(mixed with hydrocodone), Combunox (mixed with oxycodone), Indocin, Indocin SR, Indo-Lemmon, Indomethaga, Oruvail, Toradol, Ponstel, Mobic, Relafen, Naprosyn, Anaprox, Anaprox DS, EC-Naprosyn, Naprelan, Naprapac (packaged with lansoprazole), Daypro, Feldene, Clinoril, Tolectin, Tolectin DS, Tolectin 600
Vicoprofen includes the same dose of ibuprofen as over-the-counter (OTC) NSAIDs and is usually employed for less than 10 days to treat pain. The OTC NSAIDS label warns that long-term continuous use may improve the risk of heart attack or stroke. This Medication Manual has been approved by the U.S. Food and Drug Administration.
Overdosage
The subsequent symptoms may also be observed following overdosage: nausea, vomiting, extreme headache, dizziness, mental confusion, disorientation, and/or lethargy. There have been statements of paresthesias, numbness, and convulsions.
Therapy is symptomatic and/or supportive. The stomach should be emptied as fast as possible if the ingestion is recent. If vomiting has not happened spontaneously, the patient should be induced to vomit with syrup of ipecac. If the patient is incapable to vomit, gastric lavage should be performed. Once the stomach has been emptied, 25 g or 50 g of activated charcoal can also be given. Depending on the condition of the patient, near medical observation and nursing care can be required. The patient should be followed for several daytimes because gastrointestinal ulceration and hemorrhage have been reported as adverse responses to indomethacin. The usage of antacids may be helpful. The oral LD50 of indomethacin in mice and rats (based on a 14-day mortality reaction) was 50 and 12 mg/kg, respectively.
What should I know regarding the storage and disposal of this medication?
Hold this medication in the receptacle it came in, tightly closed, and out of reach of children. Store it at room temperature and/or out from extra heat and moisture (not in the bathroom).
It is most important to maintain all medicine out of sight and reach of children as many containers (such as weekly pill minders and/or those for eye drops, creams, patches, and inhalers) are not child-resistant and young children can also open them easily. To save young youngsters from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of sight and contact.
Unnecessary medications should be disposed of in special ways to ensure that pets, children, and other individuals cannot consume them. yet, you should not flush this medicine down the toilet. Instead, the best way to dispose of your medication is via a medicine take-back program. Talk to your pharmacist or reach your local garbage or recycling department to learn about take-back programs in your community.
FAQ
What should I avoid while taking indomethacin?
Avoid alcohol. Heavy drinking can also increase your risk of stomach bleeding. Avoid taking the aspirin unless your doctor tells you to. Ask a doctor or pharmacist before utilizing other medicines for pain, fever, swelling, or cold/flu symptoms. They may also contain ingredients comparable to indomethacin (such as aspirin, ibuprofen, ketoprofen, or naproxen).
What is the major side effect of indomethacin?
Serious side effects of Indocin may also include heart attack, stroke, skin changes (paleness, blisters, rash, and hives), weight gain, swelling, shortness of breath, tachycardia, unusual bleeding (including GI bleeding), jaundice, stomach pain, and pain with urination, bloody urine, blurry vision, and/or back ache.
Is indomethacin a good painkiller?
Indomethacin is a nonsteroidal anti-inflammatory drug with the potent antipyretic, analgesic, and anti-inflammatory activity that has been effectively used in the management of mild-to-moderate pain since the mid-1960s.
Can indomethacin damage kidneys?
Our cases deliver clinical support for this hypothesis and illustrate the fact that indomethacin, by interfering with this protective mechanism, can also lead to acute intrinsic renal failure.
Is it safe to take indomethacin daily?
For secure and practical usage of this drug, do not take more of it, do not take it more often, and do not take it for a longer time than your doctor ordered. Taking too much of this medicine may also improve the chance of unwanted effects.
Is indomethacin stronger than diclofenac?
In all measured parameters, there was no significant distinction between the two groups of indomethacin and diclofenac. Several studies about the efficacy of different drugs affecting pain relief after cesarean section have been performed.
Is indomethacin blood thinner?
Individuals taking oral blood thinners or anticoagulants, for instance, warfarin (Coumadin), should avoid indomethacin because indomethacin also thins the blood, and extreme blood thinning may lead to bleeding.
Can indomethacin cause high BP?
Although indomethacin increases blood pressure in certain patients, those with pre-existing hypertension are at the greatest risk [5,10]. Indomethacin increases blood pressure in patients controlled on ACE inhibitors, but a minimal effect is seen in patients under calcium channel blockers.
Does indomethacin damage the liver?
Drug-induced liver injury from indomethacin is usually mild-to-moderate in severity and transient but can also progress to acute liver failure and death. In larger case successions, indomethacin is rarely mentioned as a cause of acute liver failure. Rechallenges may also lead to reproduction and should be avoided.
Who should not take indomethacin?
You should not utilize indomethacin if you are allergic to it, or if you have ever had an asthma attack or extreme allergic reaction after taking aspirin or an NSAID. If you are pregnant, you should not take indomethacin unless your medic tells you to.
Does indomethacin increase uric acid?
Indomethacin (2.5 mg/kg) causes a rapid expansion in plasma urate concentrations and at 5 mg/kg I.M. may also cause death by deposition of urates in the viscera (visceral gout). This enlargement is probably a consequence of decreased renal tubular urate secretion.