Instrument Assisted Soft Tissue Mobilization
Introduction
Instrument Assisted soft tissue mobilization (IASTM) may be a skilled myofascial intervention utilized for soft-tissue treatment. it is supported by the principles of James Cyriax cross-friction massage. Manual therapies are units practiced by many sorts of practitioners worldwide to alleviate human tormented by myofascial syndromes, improve well-being, and/or increase athletic performance.
Instrument Assisted Soft Tissue Mobilization (IASTM) is an associate adjunct modality that will facilitate the delivery of many manual medical aid techniques and ultimately improve patient outcomes. Like another manual therapy, Instrument Assisted soft tissue mobilization has not been resistant to contention and confusion created by proprietary entities dueling over language, precedence, and exclusivity.
This has sadly prevented evolution within the technique by creating teachers reluctant to show and introduce fearing revenge for not properly endorsing an advertisement completely. Today, there’s no have to be compelled to endorse any business complete of instrument or technique faculty. This short Primer is meant to be used as a resource to introduce IASTM to practitioners, academic establishments, clinic systems, and associated continued education seminars openly. All technique recommendations area unit was nonmoving within the current science of manual medical aid and function as a baseline for intuitive application whereas permitting flexibility for innovation.
It is applied exploitation instruments that area unit typically fabricated from stainless steel with beveled edges and contours which will change to different body anatomical locations and permit for deeper penetration. it’s used for the detection and treatment of soppy tissue disorders. A planned definition for IASTM is “a skilled intervention that features the employment of technical instrument to manage the skin, myofascial, muscles, and tendons by numerous direct compressive stroke techniques”.
The procedure itself is said to have evolved from Gua sha which is a method used in Chinese medicine. Gua sha uses instruments with smoothed edges to scrape the skin till red blemishes occur. However, Gua sha has a different rationale, goals, and application method from Instrument Assisted Soft Tissue Mobilization. Unlike the Cyriax approach utilizing digital cross friction, Instrument Assisted Soft Tissue Mobilization is applied using specially designed instruments to provide a mobilizing effect to soft tissue (e.g., scar tissue, myofascial adhesion) to reduce pain and improve range of motion (ROM) and function. The usage of the instrument is thought to supply a mechanical advantage for the clinician by allowing deeper penetration and more specific treatment, while also reducing imposed stress on the hands Using instruments for soft tissue mobilization is theorized to increase vibration sensed by the clinician and patient. The improved perception of vibration may also facilitate the clinician’s ability to catch altered tissue properties (e.g., identify tissue adhesions) while enabling the patient’s awareness of altered sensations within the feasted tissues.
Musculoskeletal (MS) disorders are frequently affecting approximately 100 million adults in the US per year. So tissue mobilization or manipulation (STM) is a variety of manual therapy frequently used by clinicians to address the pain and dysfunction associated with a multitude of MS conditions. 87% of clinicians report using manual therapy daily Soft Tissue Mobilization is a massage-based modality that can be administered by hand alone or with rigid devices. Instrument-assisted STM (IASTM) employs rigid devices that can also be made of different materials (e.g. wood, stone, jade, steel, ceramic, resin) to analyze and treat the soі tissue. Regardless of the method or approach or instrument material or design, Instrument Assisted Soft Tissue Mobilization, if not all types of soft tissue mobilization interventions are in essence forms of mechanotherapy that impart mechanical stimulation to the tissue with the end purpose of improved healing. Although soft tissue mobilization, including Instrument Assisted Soft Tissue Mobilization, has been used since ancient times, much remains to be understood about its mechanisms and outcomes. Нe purpose of this short review is to provide an overview of the literature related to current IASTM practice
Abstract of IASTM
This composition reviews the medium and goods of an instrument-supported soft towel rallying( IASTM), along with guidelines for its practical operation. IASTM refers to a fashion that uses instruments to remove scar apkins from injured soft apkins and grease the mending process through the conformation of new extracellular matrix proteins similar to collagen. lately, the frequent use of this instrument has increased in the fields of sports recuperation and athlete training.
Some experimental studies and case reports have reported that Instrument supported Soft Towel rallying can significantly ameliorate soft towel function and range of stir following a sports injury, while also reducing pain. Grounded on former studies, it’s allowed that IASTM can help dock the recuperation period and time to return to sports among athletes and ordinary people who have suffered sports injuries. still, many experimental studies of the mechanisms and goods of Instrument supported Soft Towel rallying has been examined, while case reports have reckoned for the maturity of papers. In the future, the scientific base of IASTM and its trustability should be handed through well-designed experimental studies on humans. also, Instrument supported Soft Towel rallying studies that have substantially concentrated on tendons need to broaden their compass toward other soft apkins similar to muscles and ligaments. Keywords Injury, Instrument- supported soft towel rallying, Pain, Range of a stir, Soft towel function
What is Instrument Assisted Therapy?
One of the most typically performed Instrument Assisted Therapies is the Graston Technique. The Graston Technique is a state of instrument-assisted soft tissue mobilization (IASTM), which is exactly what it sounds like. Graston has designed various contoured instruments to assist healthcare providers and manual therapists with an efficient way to assist treat soft tissue injuries or pain sites. They may also look scary (one of them looks like a crowbar!), but I assure you, they are not meant to be extremely painful!
How do the Graston techniques work?
Graston Technique (GT) is a non-invasive, soft tissue technique that uses specially developed stainless steel instruments to assist the clinician to identify and/or treat areas of the body exhibiting soft tissue fibrosis or adhesions. Areas of fibrosis or adhesions are thought to be found in the muscles and connective tissues with few injuries ranging from neck pain to ankle sprains.
Graston Technique permits healthcare providers to get as deep into the tissue as necessary to summon change, yet be sensitive to the patient’s pain and tolerance. As the instruments are moved over the affected area and come in contact with the soft tissue, the action will assist restore the tissue’s capacity to slide over each other for normal movement and range of motion, reducing adhesions between layers of tissue. Some will make claims that it breaks up scar tissue, but I ensure you, the only things that do that are a scalpel (surgery) and healthy movement over long periods.
In time, this process will decrease the adhered fibers, restoring the range of motion and assisting in destroying the associated pain. It can also help transform your soft tissue injury into healthy functioning tissue.
What are the benefits?
Graston Technique® permits a clinician to get as deep into the tissue to promote change. As the devices are moved over the affected area, they help break up scar tissue and fascial restrictions. In time, this process can also decrease or eliminate the adhered fibers, restoring the range of motion and assisting to eliminate the associated pain. Graston Technique® is useful for a wide range of patients, including those with surgical and non-surgical orthopedic conditions. Any patient with soft tissue restrictions affecting their progress can benefit from this technique.
What could you expect from experience with Graston or other instrument-assisted soft tissue mobilization (IASTM) therapies?
The sensation of a Graston treatment (or any other type of instrument-assisted soft tissue treatment) may also be similar to a massage that is paired with some light active movement or stretching throughout. The intensity can also easily be changed to fit the pain tolerance of the patient. A typical treatment does not require to be long, with some lasting only a few minutes to get the desired effect. As with most soft tissue issues or injuries, the treatment should be paired with some sort of exercise afterward to receive the desired effect and assist restore the healthy function of the affected area.
Are there situations where Graston Technique should not be used?
The most familiar situation in which clinicians will avoid this treatment is if you are taking a prescription blood thinner due to improved risks of bruising.
Are there any side effects from IASTM?
Probable side effects from Graston Technique or IASTM must be minor if any. It is expected to have some mild tenderness or redness around the affected area, but this should clear up within hours or a couple of days thereafter. It is not abnormal to also have some minor bruising around the area, although this is not necessary to obtain the desired effect.
How does it work?
Instruments break down fascial restrictions and scar tissue. The ergonomic form of these instruments provides the clinician with the ability to locate restrictions and permits the clinician to treat the affected area with the appropriate quantity of pressure. The introduction of controlled microtrauma to affected soft tissue structure generates the stimulation of local inflammatory response. Microtrauma initiates the reabsorption of improper fibrosis or excessive scar tissue and stimulates a cascade of healing activities resulting in the remodeling of affected soft tissue structures. Adhesions within the soft tissue which may also have developed as a result of surgery, immobilization, repeated strain, or other mechanisms, are broken down allowing full functional restoration to occur.
The Purpose of Instrument Assisted Soft Tissue Mobilization?
Instrument Assisted soft tissue mobilization is a specialized technique used with hand-held tools which enable clinicians to efficiently locate and treat soft tissue dysfunction. Instrument Assisted soft tissue mobilization is performed with specifically designed instruments that are used to catch and treat fascial restrictions such as scar tissue. Scar tissue forms in an irregular pattern within a damaged area of tissue. Scar tissue can also limit movement and produce pain. Instrument Assisted soft tissue mobilization is performed to break up scar tissue and trigger an inflammatory response. The inflammation response allows the body to absorb scar tissue and produce new collagen around the site of injury.
Conditions For Which IASTM is Usually Used
Anyone with soft-tissue pain, injuries, or conditions can benefit from Instrument assisted soft-tissue mobilization. These often contain athletes, warehouse workers, or others who perform a repeated motion many times per day. Some of the many conditions we can also treat with IASTM include:
- Medial Epicondylitis, Lateral Epicondylitis
- Carpal Tunnel Syndrome
- Neck Pain
- Plantar Fascitis
- Rotator Cuff Tendinitis
- Patellar Tendinitis
- Tibialis Posterior Tendinitis
- Heel Pain or Achilles Tendinitis
- DeQuervain’s Syndrome
- Post-Surgical and Traumatic Scars
- Myofascial Pain and Restrictions
- Musculoskeletal Imbalances
- Chronic Joint Swelling Associated with Sprains/Strains
- Ligament Sprains
- Muscle Strains
- Non-Acute Bursitis
- RSD (Reflex Sympathetic Dystrophy)
- Back Pain
- Trigger Finger
- Hip Pain (Replacements)
- IT Band Syndrome
- Shin Splints
- Chronic Ankle Sprains
- Acute Ankle Sprains (Advanced Technique)
- Scars (Surgical, Traumatic)
Although, some patients are not good candidates for Instrument assisted soft tissue mobilization. If you have a degenerative joint condition, such as arthritis, IASTM may assist to relieve pain in the tissues surrounding the joint but not in the joint itself.
What to expect from the IASTM treatment
A person receiving the Instrument Assisted Soft Tissue Mobilization treatment must realize that it essentially re-injures the body in a controlled manner, and to a lesser degree. During the procedure, patients may have some discomfort and may have soreness in the area that was treated. The numeral of treatments may also vary from person to person, but usually two treatments per week for up to five weeks. Generally, positive results can be experienced by the third or fourth treatment.
Exercise after the IASTM treatment is important. The muscles need to be stretched to help build up strength in the injured area, and flexibility as well. The entire process can also be accelerated if patients follow the specified guidance of their physical therapist to do home exercises following an Instrument Assisted Soft Tissue Mobilization treatment. The body will discern like new again.
Contraindications of IASTM
- Acute wound or infection (viral or bacterial), fever, or contagious condition
- Petechiae (severe) or ecchymosis
- Skin hives, open wounds, blisters, local tissue inflammation, or tumors
- Treatment over surgical hardware
- Osteoporosis (advanced)
- Cancer or malignancy
- Unhealed or unstable bone fracture
- Hypertension (uncontrolled)
- Hematoma, myositis ossificans
- Insect bite of unexplained origin
- Acute or severe cardiac, liver, or kidney disease
- Congestive heart disease, circulatory disorders
- Neurologic conditions resulting in loss or altered sensation (e.g. Multiple Sclerosis)
- Bleeding disorders (Hemophilia)
- Metabolic conditions (e.g. Diabetes) or high-risk pregnancy
- Unhealed surgical site
- Connective tissue disorders (e.g. Ehlers-Danlos syndrome, Marfan’s syndrome)
- Peripheral vascular disorder or deficiency, varicose veins
- Medications that thin blood or altered sensations
- Thrombophlebitis or osteomyelitis
- Chronic pain conditions (e.g. Rheumatoid Arthritis)
- Unassuming pressure over the face, eyes, arteries, veins (varicose veins), or nerves
- Recent surgery or injury
- Direct pressure over bony prominences or provinces (e.g. lumbar vertebrae)
- Severe pain felt by the patient
- Epilepsy (unstable)
IASTM Physiology & Benefits
Physiological Mechanism
- Studies have addressed the advantages of IASTM at the cellular level. The inflammatory response initiated through micro trauma to the affected tissues results in increased fibroblast proliferation, collagen synthesis, maturation, and the remodeling of unorganized collagen fiber matrix following Instrument-Assisted Soft Tissue Mobilization application. Which results in a breakdown of scar tissues, adhesions, and fascial restrictions.
- Fibroblast is considered the most important cell in the extracellular matrix (ECM). The repair, regeneration, and supervision of soft tissue take place in the ECM. The fibroblast synthesizes the extracellular matrix, which includes collagen, elastin, and proteoglycans, among many other essential substances. Fibroblasts can react as mechanotransducers, which means they are competent to detect biophysical strain (deformation) such as compression, torque, shear, and fluid flow, and create a mechanochemical response.
- Gehlsen et al analyzed the effects of 3 separate IASTM pressures on rat Achilles tendons. They concluded that fibroblast production is directly proportional to the magnitude of Instrument Assisted Soft Tissue Mobilization pressure used by the clinician. Davidson et al supported Gehlsen et al. by concluding that Instrument Assisted Soft Tissue Mobilization significantly increased fibroblast production in rat Achilles tendons by using electron microscopy to analyze tissue samples following Instrument Assisted Soft Tissue Mobilization application. Davidson et al. found morphologic changes in the rough endoplasmic reticulum following Instrument Assisted Soft Tissue Mobilization application. Therefore, indicating micro-trauma to damaged tissues, resulting in an acute fibroblast response.
- IASTM has a neurophysiological effect as it stimulates mechanosensitive neurons via skin deformation by the instrument. Mechanosensitive neurons consist of mechanoreceptors which are responsible for two-point discrimination and mechano-nociceptors which are reliable for pain perception. A study by Weiqing Ge found that Instrument Assisted Soft Tissue Mobilization changed the neural activity of the large mechanoreceptor neurons affecting the two-point discrimination. Another study by Scott W. Cheatham et al examine the effect of IASTM on DOMS (delayed onset muscle soreness) and the results found a decrease in the area of two-point discrimination suggesting increased local tactile sense through mechanoreceptors stimulation and a reduction in the pain pressure threshold which suggest that light Instrument Assisted Soft Tissue Mobilization modulated the nociceptors ( small pain fibers) activity.
- IASTM involves the vascular response to the damaged soft tissue, by increasing the blood flow. As evident by Loghmani et al, who studied the effect of Instrument Assisted Soft Tissue Mobilization on the knee MCL in rats, and found an increase in tissue perfusion and an increase in the proportion of arteriole-sized blood vessels in the treated leg.
Researchers have also found that IASTM changes local temperature and has an effect on two-point discrimination and pressure pain threshold. Instrument Assisted Soft Tissue Mobilization treatment might also have the potential for provoking connective tissue remodeling through resorption of excessive fibrosis, along with inducing repair and regeneration of collagen secondary to fibroblast recruitment. In turn, this may also result in the release and breakdown of scar tissue, adhesions, and fascial restrictions. In laboratory analyses using a rat model, the use of instruments resulted in improved fibroblast proliferation and collagen repair (e.g., synthesis, alignment, and maturation) in cases of enzyme-induced tendinitis. Many of these benefits were also found in a laboratory study on ligament healing utilizing the rat model which demonstrated that IASTM in an animal model produces a significant short-term (e.g., four weeks) improvement in ligament strength and stiffness compared to the contralateral control limb. While these findings provide initial support for Instrument Assisted Soft Tissue Mobilization stimulating connective tissue remodeling, these physiological changes are still being studied and have not been confirmed in human trials.
Clinical Benefits
Investigations have also shown clinical benefits of IASTM showing improvements in range of motion, strength, and pain perception following treatment. Melham et al found that IASTM significantly improved the range of motion in a college football player following 7 weeks of IASTM and physical therapy. Melham et al. found that scar tissue wrapping the lateral malleolus was relieved and remodeled structurally following IASTM application. Wilson et al found improvement in pain reduction and impairment scale at 6 & 12 weeks following Instrument Assisted Soft Tissue Mobilization application for patellar tendonitis. Targeted IASTM treatments can have several benefits, such as:
- Faster pain relief
- Quicker rehabilitation and recovery
- Increased collagen production
- Restoring proper function
- Speeding up recovery time
- Reducing inflammation
- Improved mobility
- Alleviating chronic pain conditions
- No downtime, you can continue activities at normal
IASTM concentrates on specific areas to relieve stiffness and improve the range of motion. This allows you to perform exercises your physical therapist recommends strengthening the injured area, which promotes healing and can help restore your normal function.
Benefits to the Therapist
IASTM provides clinicians with a mechanical benefit, thus discouraging over-use of the hands, it provides deeper tissue penetration with less compressive forces to the interphalangeal joints of the clinician’s hand. Snodgrass SJ surveyed physical therapists and found that after spinal pain, the second most common cause for absenteeism from work was the overuse of the thumb. Ninety-one percent of physiotherapists employing some sort of massage had to modify their treatment strategies because of thumb pain.
Also, it improves the vibratory perception of the physical therapist’s hand carrying the instrument to alter soft tissue properties such as tissue restrictions or adhesions. So the therapist can detect soft tissue irregularities easier.
Types of Tools
The utilization of tools to evaluate tissue quality and to treat areas identified to have scar tissue, soft tissue restrictions, chronic inflammation, or degeneration. There are many corporations for IASTM such as RockTape®, HawkGrips®, Graston®, Técnica Gavilán®, Functional and Kinetic Treatment with Rehab (FAKTR)®, Adhesion Breakers®, augmented soft-tissue mobilization or ASTYM®, and Fascial Abrasion Technique™. Each company has its treatment approach with different instrument designs. The tools such as

- Spoon Shaped Tools
- Beveled edge tools
- Handlebar
IASTM could be made from varying materials including stainless steel, titanium, plastic, buffalo horn, stone, quartz, and/or jade. The considerable common IASTM instruments used are stainless steel.
We commonly advise against the type of self-IASTM gaining popularity among CrossFitters, etc. It is important to comprehend the anatomy and function of the areas being treated. Most chiropractors and body workers that use IASTM have comprehensive training. Self-myofascial escape tools, such as foam rollers, trigger point balls, and/or massage sticks, have become some of the most popular tools used for corrective exercises, fitness, and sports performance.
Practical Application Of IASTM
IASTM can not be done by itself, it must be combined with a motion and strengthening program to improve tissue remodeling. When IASTM is applied it goes through 6 steps
- Examination
- Warm-up, warm-up is done for 10 to 15 mins by light jogging, elliptical machine, stationary bike, or an upper body ergometer
- IASTM, done at 30 to 60 degrees angle for 40 to 120 seconds
- Stretching, 3 reps for 30 seconds
- Strengthening, high repetitions with low load exercise
- Cryotherapy, 10 to 20 min
It is important to disinfect the instrument between patients to dodge the transfer of infections. It is suggested to disinfect the instrument with intermediate-level disinfectants (e.g. isopropyl alcohol), then wash it with soap and water to empty any residuals of the chemical disinfectant from the instrument. If the tools contact with blood, bodily fluids, mucous membranes, or non-intact skin then disinfecting it with high-level disinfectant should be done.
Effect of IASTM
Soft tissue function
Diminished soft tissue function following a sports harm makes it difficult to partake again in sports or activities of daily living. Hence, recovery of soft tissue function represents one of the most important goals in sports rehabilitation. IASTM has been studied mostly concerning tendon injuries. Previous investigations have demonstrated IASTM as a treatment technique that can also bring about positive changes in the recovery of soft tissue function following a tendon injury. Black (2010) stated that when five sessions of IASTM were applied over 4 weeks in patients who sustained patellar tendon injury from basketball, their lower extremity functional scale (LEFS) scores increased by 23% to 44%, while Sevier and Stegink-Jansen (2015) reported that when IASTM was applied twice a week for 4 weeks in patients with lateral elbow tendinopathy, better known as tennis elbow, their DASH (disabilities of the arm, shoulder, and hand) scores reduced more than those of the eccentric exercise group and their maximum grip strength improved. Meanwhile, Park et al (2015) reported that providing IASTM three times a week for approximately 22 days in patients hospitalized for Achilles tendinitis resulted in a significant improvement in walking distance; patients who had difficulties walking 180 m before IASTM application were able to increase their walking distance up to 390 m after IASTM. Moreover, Papa (2012) also revealed that when IASTM was applied for one to two sessions per week for 8 weeks as part of a rehabilitation program for patients with Achilles tendinopathy, their LEFS scores enhanced from 48 to 80.
Recently, McConnell et al (2016) applied eight sessions of IASTM over 4 weeks in adults with Achilles tendinopathy and found that Young’s modulus, a measure of elasticity, increased by 34.5% and stiffness increased by 31.8%, while the Victorian Institute of Sport Assessment for Achilles (VISA-A) score, an index showing the severity of Achilles tendinopathy, improved from an average of 13 points to 86 points. Moreover, two subjects, in particular, conducted VISA-A scores of ≥90 points, indicating that they had recovered from Achilles tendinopathy. In addition, McConnell et al (2016) also reported clinically significant changes in the functional test results of patients with Achilles tendinopathy after applying IASTM. Furthermore, a study by McCormack et al (2016) showed that applying a combination of eccentric exercise together with IASTM for 12 weeks resulted in a greater improvement in VISA-A scores of patients with Achilles tendinopathy when corresponding with applying eccentric exercise alone. The fact that these improvements were sustained actually at the 26th and 52nd week of treatment is especially noteworthy.
Chronic tendon injuries, such as tendinopathy, require lengthy management due to the physiological and/or anatomical features of tendons and, in some cases, the patient may not reply well to treatments (Sharma and Maffulli, 2005). In comparison to muscles, tendons have lower oxygen consumption and metabolic rate and therefore demonstrate slower healing after an injury (Williams, 1986). Up to now, drugs and/or physical therapy have been used for the treatment of tendinopathy, but there are inconsistent opinions on their effectiveness (Andres and Murrell, 2008). especially in the case of steroids, they may be effective for controlling pain in a patient with tendinopathy over the short term, but long-term use might have negative effects on the soft tissue function as they can also delay tissue healing and further exacerbate the injury (Magra and Maffulli, 2006; Marsolais et al., 2007).
In light of this, IASTM can be considered a good alternative for the recovery of soft tissue function following tendinopathy. Current reports have also revealed that IASTM can be used to prevent Achilles tendinopathy. Bayliss et (2015) applied eight sessions of IASTM over 4 weeks in adults who had been confirmed to have a shortened Achilles tendon from a lunge test and found that their tendons showed a pattern of a significant gain in Young’s modulus and an increase in tendon resting length than the control tendons that underwent simple stretching alone. If the Achilles tendon becomes shortened, it advances the risk of injury to the lower extremities and can also progress into Achilles tendinopathy, while the running efficiency is also decreased (Bayliss et 2015). Therefore, increasing Young’s modulus or the resting length of shortened tendons through IASTM can not only destroy the potential risk for Achilles tendinopathy but could also lead to a potential functional improvement.
In the meantime, some analyses have reported that IASTM can also affect muscles. Faltus et al (2012) stated that when five sessions of IASTM were applied over 6 weeks in a cyclist who had sustained a partial rectus femoris tear, ultrasound examination demonstrated a reduced focal lesion size, echogenicity, and/or hypoechoic zone around the tissue when compared with the outcome from the early stage of treatment, while also demonstrating improved tissue continuity. After involving IASTM, morphological changes in the tissues confirmed via ultrasound examination can also serve as direct evidence of musculoskeletal functional recovery, and such morphological changes have been shown to lead to improved LEFS scores (from 67 to 75). Nevertheless, this study was a case report applying just one cyclist, implying that it is necessary to conduct studies with larger sample sizes. Kivlan (2015) used a unilateral isometric squat to measure muscle interpretation in patients with muscular weakness from injury instantly after a single application of IASTM on lower extremity muscles.
The results demonstrated that the change in maximal force output was significantly improved in the IASTM group than in the placebo and control groups. Unlike the study by Faltus (2012), the study by Kivlan (2015) was able to quickly show a significant change in muscle function despite only a single application of IASTM. Concerning the potential mechanism of action, Kivlan (2015) suggested an expansion in fascial mobility, the proliferation of extracellular matrix fibroblasts, and blood supply to the area near the injured tissue, along with a decrease in cellular matrix adhesion and/or localized ischemia. As already described in the “Mechanism of IASTM” section of this article, some of the hypotheses suggested by Kivlan (2015) have been proven through several animal and human studies (Davidson et al., 1997; Loghmani and Warden, 2009, 2013; Portillo-Soto et al., 2014).
In outline, it was found that IASTM can also stimulate not only tendons but also other soft tissues, such as muscles, to assist improve soft tissue functions chronically or acutely. Nevertheless, it is still unclear to which extent structural and functional changes in tendons or muscles generated by IASTM may also affect future injuries or prevention. Hence, it is necessary to confirm these aspects through long-term observations.
Pain
The pain decrease effects of IASTM have already been proven in some studies of musculoskeletal diseases. Lee et al. (2016) reported that when IASTM was applied for 4 weeks in 30 patients with chronic lumbar pain, the pain reduced significantly. Earlier, Howitt et al. (2006) demonstrated that applying eight treatment sessions of IASTM over 4 weeks on trigger thumb patients was useful in reducing pain. Similar outcomes have been found in studies of sports injury. Aspegren et al. (2007) stated that when IASTM was applied twice a week for 2 weeks in female collegiate volleyball players diagnosed with acute costochondritis, the pain was reduced, enabling the players to participate in their sport again, while in a study by Daniels and Morrell (2012), the pain was decreased in youth football players with plantar fasciitis by applying IASTM once a week for 6 weeks. Howitt et al. (2009) also reported that when IASTM was included in the rehabilitation program for triathletes with tibialis posterior sprain, the pain was decreased 2 weeks after applying IASTM, and after 6 weeks, the pain dispersed completely to allow the triathletes to participate again in running or swimming. Meanwhile, White (2011) involved one to two sessions of IASTM a week for 6 weeks in a 36 year aged distance runner with hamstring tendinopathy, following which the hamstring pain was fixed.
Normally, pain is caused by inflammation( Proske and Allen, 2005). When an injured towel becomes lit, vulnerable cells are signed and phagocytosis occurs. Pain is convinced when towel fractions perished by phagocytosis or substrates buried by colorful vulnerable cells stimulate type III and IV whim-whams consummations( Graven- Nielsen and Mense, 2001). In particular, following a sports harm, if the injured area is not treated duly or rehabilitated adequately, also habitual inflammation may lead to towel degeneration and come cause of long- term pain( Franceschi and Campisi, 2014).
Theoretically, control of inflammation can be considered as an implicit reason for the capability of IASTM to reduce pain. Crane et al.( 2012) stated that soft towel rallying was effective in reducing exercise-convinced inflammation, but in this particular study, a massage fashion, and not IASTM, was applied. still, according to a study by Vardiman et al. ( 2014), IASTM was set up to not affect changes in inflammation-related factors, and pain increased after applying IASTM. In the study by Vardiman et al.( 2014), there were no situations in which inflammation passed. The study subjects were healthy with no inflammation and an exercise model for converting injury wasn’t applied. thus, the goods of IASTM on seditious changes are still unknown and this content requires further study. Another possibility includes increased blood inflow because of IASTM. Increased blood inflow can snappily remove pain substrates or reduce swelling that develops around the injured towel( Zainuddin et al., 2005). Loghmani and Warden( 2013) indicated that IASTM bettered perfusion, while Portillo- Soto et al. ( 2014) suggested that IASTM increased blood rotation. still, there’s no direct substantiation of increased blood inflow caused by IASTM leading to pain reduction.
Range of motion
Sufficient common ROM is demanded optimal musculoskeletal function and inadequate inflexibility can make one vulnerable to overuse patterns and acute injuries( Hreljac et al., 2000; Sainz de Baranda and Ayala, 2010). thus, having sufficient ROM is important for perfecting exercise performance, in addition to the recuperation or forestallment of sports injuries( Merkle et al., 2016). Some studies have suggested that IASTM can significantly ameliorate ROM( Baker et al., 2013; Hammer and Pfefer, 2005; Kim et al., 2014; Laudner et al., 2014). Hammer and Pfefer( 2005) reported that when IASTM was applied doubly per week for 3 weeks in cases who had midriff pain from cube pattern, there was an increase in hamstring inflexibility, while Baker et al.( 2013) applied three sessions of IASTM for 1 week on the hamstrings and triceps surae of men who had problems in the lower extremities, similar as miserliness and pain, which redounded in increased sit and reach( 5 cm) and active straight leg raise (7.5 °).
IASTM improves the extensibility of soft apkins by treating their restrictions( Heinecke et al., 2014), and when heat is generated from disunion by the instrument, the density of the towel decreases, making it softer( Markovic, 2015). Physiologically, a drop in the density of the towel improves ROM( Ostojic et al., 2014). Meanwhile, significant changes in ROM as a result of IASTM can also be explained by suppositions related to the nervous system. When mechanical stress is wielded on the muscle fascia, interfacial mechanoreceptors come stimulated. This change alters the proprioceptive input transferred to the central nervous system, which in turn changes the pressure in towel-related motor units( Schleip, 2003). Although it’s believed that IASTM improves ROM via the mechanisms described in these suppositions being singly or as a combination, scientific evidence to support similar claims is still lacking.
IASTM showed enhancement in ROM in studies in athletes as well. Merkle et al.( 2016) indicated that applying two sessions of IASTM per week for 3 weeks in healthy collegiate baseball players significantly bettered their hamstring ROM, while Heinecke et al.( 2014) mentioned that applying two sessions of IASTM per week for 4 weeks to the shoulder area of collegiate softball, baseball, and volleyball players was useful in precluding a loss of ROM. Unlike some studies, other studies have shown a significant enhancement in ROM from just a single operation. Kim et al.( 2014) showed enhancement in ROM after a single operation of IASTM in the hamstrings of adult men and women( before133.4 ° ±6.7 °, after146.1 ° ±13.2 °), while Laudner et.( 2014) reported that a single operation of IASTM helped ameliorate ROM in the entire shoulder area of collegiate baseball players. In the study by Laudner et al.( 2014), the IASTM group(11.1 °) showed significantly bettered ROM when compared with the control group(−0.12 °), and a significant difference in glenohumeral internal gyration ROM was also set up between the IASTM(4.8 °) and control groups(−0.14 °).
Lately, Markovic( 2015) applied a single session of IASTM or froth breakers on the hips and knees of soccer players and measured their ROM via unresistant knee flexion and straight leg raise tests. Their results showed that incontinently after the treatment, ROM was bettered more in the IASTM group than in the froth comber group( 10 – 19vs. 5 – 9); at 24 hr after the treatment, only the IASTM group showed bettered ROM( 7 – 13). The fact that the studies by Laudner et al.( 2014) and Markovic( 2015), in particular, were conducted on baseball or soccer players can be viewed as furnishing evidence that IASTM can be applied with positive goods within a short period in athletes who suffer from habitual ROM restrictions. still, there’s one limitation in generalizing the results from these three studies that used a single operation of IASTM( Kim et al., 2014; Laudner et al. 2014; Markovic, 2015). The subjects in all three studies didn’t have sports injuries and were in a healthy state. thus, it’s necessary to probe whether a single operation of IASTM could significantly ameliorate ROM in people with sports injuries. Meanwhile, Vardiman et al.( 2014) reported that a single operation of IASTM in healthy men doesn’t affect changes in ROM. It’s believed that these disagreeing study results may be attributed to differences in subject characteristics, material and operation protocol of the IASTM instrument, and ROM dimension positions.
Precautions For IASTM
- Anti-coagulant medications, hormone replacement, fluoroquinolone antibiotics NSAIDs, steroids, narcotics
- Cancer, Hypertension
- Varicose veins
- Burn scars, Lymphedema, Osteoporosis
- Acute inflammatory conditions, Rheumatoid arthritis, ankylosing spondylitis
- Kidney dysfunction
- Inflammatory condition secondary to infection
- Pregnancy, Diabetes, Polyneuropathy
- Petechiae, Abnormal sensations (e.g. numbness).
- Patient age, flu or flu-like symptoms
- Post-injection (e.g. steroid)
- Unhealed closed or non-complicated fractures
- Congestive heart disease, circulatory disorders
- Pacemaker or insulin pumps (treatment around devices)
- Patient intolerance, hypersensitivity, and high pain sensation due to injury
- Autoimmune disorders, Reflex sympathetic dystrophy, or chronic regional pain syndrome
- Allergies to metals, emollients, latex (professional wearing gloves)
More cautions to assume regarding IASTM treatment are:
Critical Injuries- many IASTM rationales and the strokes associated with them are not appropriate for acute injury. Yet, edema stroking with a concave edge around the tissue – bringing interstitial protruding proximally out of the injured compartment is extremely beneficial. Following that, Kinesio-tape can also often be used to support the compartment and lessen additional edema. Performance Event or Life Event Timing- it is not a good idea to perform an intense treatment (one that requires 1 to 3 days of recovery) right before the championship game, marathon, work commitment, travel, etc. All you have to do is communicate with your patient and adjust the treatment accordingly
Compressive Neuropathy- Nerves are not connective tissue and are extremely sensitive. A radiculopathy or nerve compaction is treated by addressing the connective tissue adjacent to the nerve. Having a tool that is easy to manage along with an appropriate understanding of anatomy will make treatment successful. Be aware when utilizing deep strokes with a long edge, that you may be incidentally applying too much pressure over a nerve. Injured Tendons or Ligaments- Never apply IASTM to the site of acute tendon or ligament trauma. Comprehend the Kinetic Chain concept sufficiently to know that the point of failure or site of pain is RARELY the primary site of myofascial dysfunction. Look for attributes above and below the injury to perform your treatment.
Bony Importance eases up pressure during the stroke when you are working near or crossing over a bony landmark. Treatment Mark or Social Implications- occasionally incidental during the correct application of IASTM, bruising, reddening, and capillary damage can be misinterpreted as abuse, and either cause a loved one of the patient to make false assumptions or cause embarrassment to the patient if the mark is in a visible area of the anatomy during social interaction. Case in point- the author left a mark on the levator scapulae the day before a female patient was to stand up at a wedding wearing a strapless dress
Limitations of IASTM
The leading limitation of this systematic review is the paucity and heterogeneity of evidence encircling IASTM. For example, it is difficult to compare the results of analyses utilizing only IASTM therapy versus those utilizing IASTM as part of a medicine protocol with other adjunct therapies (e.g., ultrasound, stretching, exercise, etc.). This problem is further compounded when the IASTM application is used with patient populations who may theoretically react to IASTM therapy without adjunct therapy (e.g., tendinopathy) and those who likely require adjunct therapy (e.g., chronic ankle instability). Additionally, it is challenging to assess IASTM treatment effectiveness, even when used in isolation, given the unpredictable methodology (e.g., treatment time variation, application of static versus dynamic IASTM treatment, etc.) used across studies. A second limitation is the search criteria for this review which banned lower-level evidence (e.g., case reports) and concentrated on higher-level clinical trials. A third limitation is the literature search only contained English language publications which may not have described all the available evidence from non-English studies or investigations currently submitted for the magazine. Another potential limitation may be the search criteria concentrating on IASTM methods utilizing the most homogenous rationale and therapy approach which led to the exclusion of Gua sha and ASTYM® for comparison.
Treatment of IASTM
The IASTM treatment is allowed to stimulate connective towel revising through resorption of inordinate fibrosis, along with converting form and rejuvenescence of collagen secondary to fibroblast reclamation. In turn, this will affect the release and breakdown of scar towels, adhesions, and fascial restrictions. In laboratory studies using a rat model, the use of instruments redounded in increased fibroblast proliferation and collagen form(e.g., conflation, alignment, and development) in cases of enzyme-convinced tendinitis. numerous of these benefits were also set up in a laboratory study on ligament mending using the rat model which further handed supporting substantiation that instrument massage produces a significant short-term (e.g., 4 weeks) increase in ligament strength and stiffness compared to the contralateral control branch. While these findings give original support for IASTM stimulating connective towel redoing, these physiological changes are still being studied and haven’t been verified in mortal trials.
There are colorful IASTM tools and companies similar to Graston ®, Técnica Gavilán ®, Hawk Grips ®, Functional and Kinetic Treatment and Rehab( FAKTR) ®, Adhesion Breakers ® and Fascial Bruise fashion ™ that have their approach to treatment and instrument design(e.g., instrument accouterments, instrument shape). Anecdotally, the Graston ® fashion contains a protocol for treatment that contains several factors examination, warm-up, Instrument assisted soft tissue mobilization treatment(e.g., 30 – 60 seconds per lesion),post-treatment stretching, strengthening, and ice( only when subacute inflammation is of concern).12 Despite the variations in treatment approaches and design, the general premise of IASTM is to enhance myofascial mobility with limited adverse goods similar to discomfort during treatment or bruising(e.g. petechiae) after treatment.
For Instrument assisted soft tissue mobilization, the subject was seated in a relaxed position. The subject’s forehead catnapped on his or her forearm on a table in front of him or her. A lubricant (Vaseline) was applied to the skin around the neck area before treatment and the M2T blade was cleaned with an alcohol pad. First, the M2T blade was used to find the precise areas of restriction in the RT upper trapezius. Then the M2T blade was used, at an angle of 45° and utilizing treatment planes 1, 2, and 3, to apply slow strokes along the muscle, without causing any distress or pain, from the muscle origin to its insertion (sweeping technique), for approximately 3 min. This technique was repeated twice a week for four weeks. Subjects were instructed to put an ice pack on the area if they sensed any burning sensations after the session.
After the IASTM session, each subject received a passive stretching exercise of the RT upper trapezius. This involved laterally flexing the head toward the left side, holding that position for 30 s, and repeating it 3 times. Flexion of the neck was raised, when appropriate, to increase the tension of the stretch. Subjects were advised to perform self-stretching exercises 5 times a week as a home program. For performing self-stretching, each subject was instructed to sit on a chair, holding the bottom of the seat with his or her RT hand to stabilize the RT shoulder, and put his or her left hand on his or her head to pull the head toward the left side. Subjects were instructed that flexion of the neck could be increased, where applicable, to increase the tension of the stretch, and that they were needed to maintain the position for 30 s and repeat 3 times.
Adequate treatment for muscle, ligament, and tendon injuries
Instrument Assisted soft tissue mobilization (IASTM) is a procedure we often use in physical therapy. IASTM works like a standard massage, but specialized instruments are utilized in place of a physical therapist’s hands. These instruments permit more direct treatment of the soft tissues concerned with the movement. The tissues include:
- Muscles
- Fascia is the connective tissue that surrounds and separates muscles
- Ligaments, the tissue that attaches bones to other bones
- Tendons, the tissue that connects muscles to bones
Instrument Assisted soft tissue mobilization can involve broad or targeted treatments. The former would be used for large muscle groups, such as an injured back, and the latter for an injury to a particular area. By using various tools, angles and pressures, your therapist can focus on a specific layer of soft tissue during treatment.
IASTM is used on many occasions. Instrument Assisted soft tissue mobilization can be used post-injury and post-surgery. IASTM is a specific treatment type to help treat acute and chronic soft tissue conditions and assist recovery after injury. Instrument Assisted soft tissue mobilization can help treat an injured area by breaking down scar tissue, restoring movement, and increasing the healing process. IASTM helps break down scar tissue that is formed around the injury. Scar tissue does not align with previous tissues which can also cause reduced strength, restrictive movement, and reduced blood flow. Instrument Assisted soft tissue mobilization helps break down scar tissue by applying movement and pressure onto the area to realign and correct the alignment of tissues. By breaking down scar tissue, movement is improved. IASTM also helps to increase the healing process to help speed up recovery from injury. Instrument Assisted soft tissue mobilization causes a mild inflammatory response that brings blood flow with cells that can help assist the injured area and remove toxins and waste products.
IASTM can also be effective in enhancing healing and soft tissue mobilization post-surgery. After surgery scarring and thickening of tissues occur produced by the body’s response to injury. Instrument Assisted soft tissue mobilization helps separate and break down scar tissue around an area. IASTM can also help me stretch connective tissue and muscle fibers to help restore movement. The friction of Instrument assisted soft tissue mobilization against the skin also increases blood circulation which is crucial to help assist in the healing process. The result of Instrument assisted soft tissue mobilization treatment after surgery can help eliminate pain and regain movement.
Basic Technique Strokes
This section will describe different therapy strokes with IASTM instruments to include their clinical rationale, and one or more of the following stroke descriptors: tool contact, approach direction, pressure, target tissue, & duration. If you have skipped straight to this section please go back and quickly inspect the precautions. If you have a clinical understanding of manual therapy, these technique strokes will be very easy to assimilate. My recommendation is, to begin with, straightforward cases of lateral epicondylitis or Illio-Tibial band syndrome. After a few treatments, you will get a feel for the instruments and patient reactions and soon be able to move on to more advanced cases. If you are a student or new to Instrument assisted soft tissue mobilization, have the tools at hand and practice the stroke on your forearm while you read the descriptions. After that practice the strokes lightly on a friend, associate student, or family member. I have been asked many times to make videos of these strokes (which I may soon), but remember it is easier to assimilate tactile information by reading simple step-by-step directions and practicing at your own pace vs. trying to emulate a stroke while watching a video. A quick note about the use of emollient- many strokes does not require emollient or oil. A highly polished finish on stainless steel provides a balance of “glide” and “grab.” If you require more glide, oil is often preferred, because it can be applied by the drop and absorbs into the skin quickly.
It is best to utilize a dropper bottle or a flip-cap bottle where you can squeeze out one drop at a time. Sunflower oil and Jajoba oil are natural, and hypoallergenic, provide good glide and absorb quickly into the skin. A Jojoba and Instrument assisted soft tissue mobilization emollient is available for Some strokes like Cyriax or Fascial Manipulation® specifically DO NOT require emollient or oil because more “grab” is desired to pull the skin back and forth over the underlying myofascial. Finally, many strokes can also be performed through the cloths when treating during a sports event, or in your treatment room when approaching sensitive anatomy (e.g. sternal area, coccyx)
1 – Diagnostic Scanning Stroke
Diagnostic scanning is used with light pressure and applied gradually in long strokes around the area of concern to make use of the ability of a tool to “amplify” the palpation of tissue topography under the skin. It is important to check an area from various vectors– both directions, parallel, cross fiber, and diagonal. When you locate a general area of interest scanning, you can also leave the tool fixed to the skin (like the Cyriax stoke described later) to get an even better feel for tissue density and tension
2 – Warming Pre-Treatment Stroke
This diversified border stroke is performed like a corresponding therapeutic massage stroke with the hands. There is much flexibility in its application. Pressure is mild to medium and strokes are usually long, 3 to 8 inches (8 to 20cm). The Warming Stroke is applied to muscle, tendon, ligament, fascia, and/or capsule in preparation for, and to enhance the effectiveness of a more intense manual therapy to follow- such as more specific Instrument assisted soft tissue mobilization, contract or relax stretching, therapeutic exercise, or joint manipulation. Direction manages to be parallel to fibers, and the duration is less than 30s for each area. The Warming Stroke is more specific and quicker than a traditional massage as a pre-treatment
3 – Cross Friction Strokes
Traditional, Modified, and Combined Movement These three-stroke styles are the most common and versatile therapeutic strokes for Instrument assisted soft tissue mobilization. These strokes are applied perpendicular to fiber mostly to tendons, musculotendinous junctions, capsules, and ligaments where tendonosis, chronic inflammation, and structural dysfunction have occurred. Based on our current understanding, connective tissue “perpendicular to the fibers” can mean in any direction over the skin depending on which layer of muscle, fascia, or ligament is being treated. Functional movements and palpation with and without the tools will help localize the plane of restriction
Traditional Cross Friction (TCS): No emollient is used. With moderate to deep pressure, the tool surface is reciprocated back and forth (about 1/4”) keeping hold of the skin– without slipping. A brisk stroke rate is applied for the 20s and repeated several times with a 10s break. Total treatment application 3-4 minutes. Considerations: between intervals, move the contact surface of the tool up or down the target area along the fibers in a 50% overlap. Possible Tool Contacts: Numerous likely the prow of the “S” or “M” instruments. It is often helpful to let the tool edge grab between the fibers- the edge is parallel- while stroking perpendicularly.
- Modified Cross Friction (MCF): Applied just as above except for “holding onto the skin.” Here, you can let the tool contact surface slide during the reciprocation. Emollient/oil is optional and may help in some applications.
- Combined Movement Cross Friction (CMCF): the limited stroke above- with additional reciprocating perpendicular to fibers- now following a vector similarity to the fibers. This concept was first expressed by therapist Therese Pfrimmer. It is also conceptualized by Andre Farasyn with his Instrument assisted soft tissue mobilization tool.
4 – Deep Fascial Release or Travell Deep Stroking
This stroke is applied similarly to fibers. A low-viscosity massage oil like jojoba is most useful. With deep pressure, the tool surface moved gradually along the fibers for the full length of a muscle and sometimes across anatomical landmarks (easing pressure accordingly) into larger fascial planes according to the lines defined by Thomas Myers. Three to Five passes via a given treatment area are usually sufficient. Travell Deep Stroking needs the same deep, slow, linear application. However, it was never given much of an official protocol, it seems instinctive to apply the Deep Fascial Release stoke over the string of points in a fibrous trigger band.
5 – Hyaluronic Acid Viscosity Stroke
This stoke is similar to a traditional cross-fiber stroke in that the contact moves fixed to the skin in a back-and-forth manner, but with two main differences. The first is the extraordinary diagnostic methodology of Fascial Manipulation® that is utilized to determine your treatment strategy. In FM you are rarely regaling the pain site or the point of structural failure as you are with a Cyriax approach. Rather, you are treating points of fascial densification that relate to the kinetic chain in 10 possible planes of motion- the two reciprocal directions in the standard anatomical planes along with reciprocal pairs in two diagonal planes. The second distinction is the duration of the stroke. This was a Eureka! the moment for the author. Where many “points” had been treated over the years relating to different techniques none maintained that steady contact is made with consistent strokes for up to 4 minutes. As soon as the third or fourth minute approached there was a simultaneous “letting go” of the tissues- an actual felt “release” that was also encountered by the patient.
6 – Riving or Channeling
(Tendon Release, Nerve Flossing, Surgical Scar Mobilization) Linear troughs for nerves, vessels, tendons, and muscle fascicules are transition points in the fascial system where layers come together. When glide is encouraged between layers as the body moves all is well- a nerve, for example, can absorb stretch within its entire length. If, nevertheless, injury overuse or structural dysfunction limits linear movement of nerve, tendon, or fascicle these structures will be prone to inflammation and degeneration. With a satisfactory understanding of anatomy and good palpation skills, a practitioner can “trace” the channels of various structures with IASTM tools and affect better manual therapy treatment. This is nevertheless another example where the human hand or finger is too big to adequately work at this scale of anatomy.
7 – Movement Assisted
(Pin & Stretch, Levy Style, FAKTR, Kinetic Mirroring) These stroke styles are very intuitive and synergize greatly with IASTM for certain approaches. For sure, the hands will still be the main avenue but there will be the “ah-ha!” times when an instrument helps. When the practitioner is combining complex restorative movement with both hands- the grip and maneuverability of an IASTM instrument become vital. The tool’s grip and especially, the balance point will either make the treatment a joy for the practitioner or be a source of frustration if the tool is uncomfortable to control.
8 – Edema Reduction Stroke
The concave border of an IASTM tool works just like a squeegee. Similar to washing water off your car windshield, it is much more comfortable to do with the squeegee at the gas station than with your bare hands. Prolonged recovery times associated with sports sprains are due mainly to the inflammatory mediators and pain-generating proteins sitting in the interstitial fluids near the injury site. Icing after an injury has been seriously questioned as it provokes immobilization, and proprioceptive numbing, and may increase swelling in the long term.
Instrument Hygiene And Safe Treatment
IASTM requires to have standard, best-practice guidelines for instrument hygiene and safe treatment because tools are utilized to treat multiple patients. Currently, no published standards exist. A recent search of peer-reviewed literature (conducted in June 2019) from electronic databases revealed no current studies analyzing the instrument disinfecting process or safe treatment sequence. The IASTM instruments are often constructed of different materials including but not limited to stainless steel, titanium, plastic, buffalo horn, stone, quartz, and jade. Regardless of material, the instruments should be considered reusable medical devices that should undergo proper hygienic procedures before and after patient treatment. Disposable or single-use IASTM instruments may be beneficial to help prevent infections, but to the author’s knowledge, manufacturers are only creating reusable instruments.
The main concern for sports medicine professionals is to determine if IASTM instruments should be classified as critical, semi-critical, or non-critical items for sterilization according to the Centers for Disease Control and Prevention (CDC). Critical items (e.g., surgical instruments) may be in touch with sterile tissues or the vascular system needing sterilization of the instruments for recurring use. Semi-critical items (e.g., respiratory equipment) are in contact with mucous membranes or non-intact skin and require sterilization or high-level chemical disinfectants (e.g., Glutaraldehyde) to clean before reuse. A few items that may come in touch with non-intact skin (e.g. hydrotherapy tanks) may also require an intermediate-level disinfectant (e.g., isopropyl alcohol, chlorine). Non-critical items (e.g., blood pressure cuff) are in touch with intact skin but not mucous membranes. Generally, they require an Environment Protection Agency (EPA) approved low-level chemical disinfectant to cleanse.
Tool disinfecting: use an intermediate-level disinfectant to clean the instrument. The flush instrument with soap and clean water before therapy. If the instrument contacts blood, bodily fluids, mucous membranes, or non-intact skin, then proper disinfecting with a high-level disinfectant or sterilization must be done.
Safe treatment series: Wash hands and wear personal protective equipment as needed. It recommends following the safe treatment sequence outlined in the instrument hygiene and safe treatment section of the commentary.
Safe Treatment Sequence Recommendations
Step 1 Before and after treatment the clinician’s hands should be cleaned. Centers for Disease Control and Prevention (CDC) guidelines recommend hand washing with soap and water or rubbing hands together using an alcohol-based hand sanitizer (e.g., gel or wipe) for a minimum of 15 seconds. Sports medicine specialists may choose to follow PPE guidelines and wear gloves during therapy but should still follow pre and post-hand hygiene procedures.
Step 2 Before treatment, the body region is inspected and cleared for treatment. Then the patient’s skin (at the treatment site) is scrubbed with a low-level sanitizing wipe (e.g. Purell®) that is secure for the skin, or 60 to 70% isopropyl alcohol to further reduce the risk of infection.
Step 3 The IASTM treatment is administered using the lubricant and PPE procedures, as needed.
Step 4 During the prescribed treatment, the sports medicine professional monitors for changes in the patient’s status (e.g., skin color changes such as petechiae, sensitivity to treatment, etc.)
Step 5 Upon completion of treatment, the body region is re-inspected and cleaned again using a sanitizing wipe or isopropyl alcohol.
Step 6 The sports medicine professional concludes with post-treatment hand hygiene, disposing of any PPE, and cleaning of the instruments.
Clinical Implications
The heterogeneity among the current IASTM analyses makes it a challenge when attempting to translate the outcomes into clinical practice. The variability in study protocols including the study population, kind of IASTM intervention, dosage time, and outcome measures make it difficult to determine the optimal treatment protocol. Five examinations were reported utilizing the Graston® technique but modified or excluded parts of the protocol. This constructs a challenge for the clinician because the Graston® method is based upon a sequential protocol and the current evidence failed to utilize this treatment method. Possibly, prospective studies must further define the intervention protocol by stating if the Graston® protocol was followed or just the tools were utilized. To date, the best available evidence for the Graston® strategy is the RCT by Burke et al. which followed the entire protocol.
Clinicians may also benefit from reading related research on the myofascial system to further understand the postulated physiological mechanisms that occur with the different myofascial therapies. Several authors have contributed to the existing body of knowledge via their research. Renowned authors such as Findley, Stecco, Langevin, and Schleip have assisted to increase our knowledge of this complex system. The reader is referred to the connection section which provides the citations for these authors
Discussion
Pre-clinical studies have demonstrated the positive effects of IASTM on connective tissue lesions. One study showed Instrument assisted soft tissue mobilization administered to chemically induced injured rat Achilles tendon resulted in fibroblast proliferation and activation, which may be associated with enhanced healing. In a subsequent study, using the same model to investigate various Instrument assisted soft tissue mobilization pressures, significantly increased fibroblast proliferation and activation were found at a greater pressure (1.5 N·mm-2) compared to light pressure (.5 N·mm-2). Loghmani and Warde found IASTM-treated injured knee medial collateral ligaments demonstrated improved biomechanical properties and structure compared to contralateral uninjured ligaments in a rodent model. Follow-up studies demonstrated increased blood flow and possible angiogenesis in the vicinity of the Instrument assisted soft tissue mobilization treated injured rat knee ligament as compared to the untreated limb. More recent animal model studies have employed mechatronic Instrument assisted soft tissue mobilization devices to explore the time and dose-pressure-dependent response effects of massage-based modalities; which have not been adequately considered in human subjects studies.
Multiple case reports have demonstrated positive IASTM treatment outcomes for numerous diagnoses, including post-natal chronic calf pain, ankle pain or fibrosis, knee arthrofibrosis, quadriceps insufficiency after a patellar tendon repair, plantar fasciitis, trigger thumb, tendinopathies, epicondylopathy and other conditions. In one case study, a male guitarist with chronic pain and functional limitations following a traumatic sprain of his left second finger proximal interphalangeal joint realized significant gains in finger flexion range of motion immediately following only one GT Instrument assisted soft tissue mobilization treatment at the first session. After six sessions, the patient encountered positive outcomes in self-reported pain and function, individually reaching a minimum clinically important difference. Physical measures also enhanced, including improved finger range of motion and grip strength. Most significantly, he was able to play the guitar with the tiniest to no pain as desired. In another case, a young male who had re-strained his quadriceps rectus femoris while playing soccer 12 months after his original injury sustained while cycling, reported improvements in pain and function after 5 GT Instrument assisted soft tissue mobilization treatments. He was able to return to playing soccer without pain or limitations, and musculoskeletal diagnostic ultrasound imaging showed decreased edema in the area of the soft tissue lesion; although, the size of the fibrotic scar did not notably change. Case series reports also suggest the benefit of Instrument assisted soft tissue mobilization intervention. Looney et al. found GT Instrument assisted soft tissue mobilization treated patients with heel pain experienced a clinically meaningful improvement in self-reported pain and function levels. McCrea et al. found Asytm IASTM benefited individuals with knee tendinopathy pain.
In a pilot study by Vardimer et al., 11 healthy, young males received one treatment of GT Instrument assisted soft tissue mobilization to one calf while the opposite calf served as an untreated, internal control. No significant discrepancies were found in the passive properties of treated vs. untreated calf muscles before, instantly after, or at 24 h, 48 h, or 72 h post-intervention; nor was there a discrepancy in physical measures or muscle biopsy inflammatory markers. However, a significant increase in self-reported pain and a decrease in function was found at 72 h post-treatment. It is essential to note that only one treatment session was delivered in this study, whereas common clinical practice typically involves at least 4 to 8 sessions for conditions affecting the calf region. Although subjects did not have a clinical condition, findings mirror a common clinical response of increased soreness within 2 to 3 days post-treatment; which typically resolves and improves during subsequent treatments. Portillo-Soto et al. demonstrated both GT Instrument assisted soft tissue mobilization and massage increase skin temperature which is associated with increased blood flow. One pilot study suggests the benefit of System Instrument assisted soft tissue mobilization in improving post-operative total knee arthroplasty stiffness and function. In another study, Davies et al. importantly found women treated post-mastectomy with Asytm IASTM had enhanced motion and function.
A diminutive clinical trial by Burke et al., in which 22 patients with carpal tunnel syndrome were randomly allocated to two treatment groups to compare the effects of two forms of manual therapy (GT IASTM vs. STM by hand-alone), for 10 restorative sessions, demonstrated improved nerve conduction latencies, wrist strength, and motion, and reduced pain in each treatment group, but no statistically significant differences were found between groups. Although this study revealed the clinical efficacy of manual therapy in this patient population, a larger sample size was needed to detect the distinction between groups. A contemporary, randomized controlled clinical trial demonstrated subjects with lateral epicondylitis had enhanced outcomes with Aystm IASTM alone and after failed eccentric exercise. Other clinical trials using System Instrument assisted soft tissue mobilization demonstrated increased lower extremity maximum force output during an isometric squat test immediately following treatment in subjects with lower extremity pain, and greater improvements were realized with Instrument assisted soft tissue mobilization in combination with eccentric exercise than with exercise alone in subjects with Achilles tendinopathy. Interestingly, no systematic inspections on massage-based therapies that included IASTM were found.
Based on the literature, it seems apparent that the rationale for using Instrument assisted soft tissue mobilization and how it’s implemented depends on several factors, e.g. the stage of tissue healing and repair; of all the patient conditions and co-morbidities; the underlying pathology, disease process or condition; tissue structure, type and location; and importantly, the desired therapy response (e.g. pro-inflammatory vs. non-inflammatory). The effects of the Instrument assisted soft tissue mobilization approach may be influenced by the instrument(s) shape and/or material. Similarly, results are instantly related to the magnitude and application of the treatment pressure, i.e. the characterization of the mechanical stimulus. Fundamentally, the key to positive developments is optimal tissue loading within a therapeutic window; yet, a limitation in the literature is the difficulty in comparing results between investigations since the quantification of IASTM force was considerably often not established. Another limitation when analyzing the literature is potential author bias.
Future directions in Instrument assisted soft tissue mobilization research consists of force quantification of the mechanical stimulus delivered with IASTM to standardize care and better compare therapy outcomes; tissue imaging to determine the effects of treatment on soft tissue structure and condition; dose-response studies in animals and humans; effects of Instrument assisted soft tissue mobilization mechanotherapy on facilitating the regenerative healing capacity and tissue properties and function of all tissue types; and necessarily, clinical outcome studies. Yet many Instruments assisted soft tissue mobilization approaches now live, it should be noted that no comparative analyses have been completed to date confirming that one is superior to another. Instrument Assisted soft tissue mobilization supposedly allows for precise and targeted delivery of force, and greater sensitivity during palpation examination of the tissue and is often utilized to enhance the clinician’s mechanical advantage and ergonomics, but further investigations are needed to validate these claims. For example, studies comparing different Instrument assisted soft tissue mobilization approaches, instrument designs, materials, and methods and STM by the hand-alone need to be completed. More studies comparing Instrument assisted soft tissue mobilization to other modalities and exercise, either in combination or alone are also warranted. Finally, all articles reviewed focused on the use of IASTM for treatment only; none considered its use in the evaluation of soft tissue dysfunction, which opens a new avenue of exploration.
Conclusion
The current evidence of RCTs does not support the efficacy of Instrument assisted soft tissue mobilization for treating certain musculoskeletal pathologies. There is weak evidence reinforcing the efficacy of IASTM for increasing lower extremity joint ROM for a short period. Instrument Assisted soft tissue mobilization is a prevalent form of myofascial therapy but its efficacy has not been fully determined due to the paucity and heterogeneity of evidence. There is a gap between the current analysis and clinical practice. A consensus has not been established regarding the optimal Instrument assisted soft tissue mobilization program, type of instrument, dosage time, and outcome measures. Future investigations are needed to assess the different IASTM tools and IASTM protocols such as Graston® utilizing the strict methodology and fully powered controlled trials. The current evidence seems to lack the methodological rigors necessary to validate the efficacy of IASTM itself or any of the Instrument assisted soft tissue mobilization protocols.
IASTM refers to a strategy that uses an instrument to remove scar tissue that had developed in soft tissues and assists in the healing process by activating fibroblasts. Instrument Assisted soft tissue mobilization is simple and practical and requires only a short period for a single treatment. According to earlier investigations, IASTM was found to enhance soft tissue function and Range of motion in acute or chronic sports injuries to soft tissues, while also reducing pain. Such positive effects can be helpful in the fields of sports rehabilitation and athletic training. However, most of the studies that supported the hypotheses concerning the mechanisms and effects of Instrument assisted soft tissue mobilization were animal studies, with very few human studies. Broadcasted articles consist mostly of patient reports rather than experimental investigations. Some of the case reports even failed to present the details of the Instrument assisted soft tissue mobilization protocol that was applied. Therefore, the scientific basis for the mechanisms and effects of IASTM must be broadened through experimental studies in humans and the reliability of the application protocol must be improved as well. Finally, to date, most of the studies concerning Instrument assisted soft tissue mobilization has focused on injuries to tendons, rather than to muscles or ligaments. Moving forward, it is necessary to provide additional proof of the effects of IASTM on muscle and/or ligaments as well.
Instrument Assisted soft tissue mobilization (IASTM) uses instruments along the skin and soft tissues to treat problem areas. IASTM can help relieve tight tissues and increase the healing process of an area. Instrument Assisted soft tissue mobilization can be effectively used post-injury and post-surgery to help break down scar tissue and adhesions which form. Instrument Assisted soft tissue mobilization produces an increase in cellular exchange, and increased vascular response, and helps realign collagen fibers. Many benefits of Instrument assisted soft tissue mobilization can be used as a specialized treatment to help reduce pain, increase movement, increase tissue elasticity and improve recovery. Massage therapists performing physiotherapy can also use IASTM to treat many conditions.
FAQ
What does IASTM manual therapy?
Instrument-assisted soft tissue mobilization (IASTM) is a method we often use in physical therapy. IASTM works like a traditional massage, but technical instruments are used in place of a physical therapist’s hands. These instruments permit more direct treatment of the soft tissues involved with the movement. It is a form of manual therapy that has been proven effective for several chronic soft tissue conditions including Plantar Fasciitis, Achilles Tendinosis, IT Band Syndrome, Shin Splints, Knee Pain, and Hip Pain.
Does the Graston Technique work?
Through this intense research, it is effective as much as 75% to 90% of the time in a range of conditions. This evidence has revealed that the Graston Technique: Divides and breaks down collagen cross-links, splaying and stretching connective tissue and muscle fibers.
Is cupping instrument Assisted soft tissue mobilization?
A new state of soft tissue mobilization that we now offer at Carousel Physical Therapy is Cupping and Instrument Assisted Soft Tissue Mobilization (IASTM). Cupping has been utilized for many years in ancient Chinese medicine.
Can you do Graston Technique yourself?
Self-treating with the incorrect tools and without expert help can cause more harm than good. I have seen patients try to achieve a Graston-like technique at home using butter knives or wrenches. Unfortunately, they usually apply too much pressure or target the wrong areas, making the problem worse.
Is Graston Technique painful?
When your chiropractor uses the Graston Technique, he or she will use stainless steel instruments to first detect areas of soft-tissue injury and then break up the restricted tissue. Although some insignificant discomfort may occur, the treatment is not painful.
How often should you do Graston?
How frequently Graston treatments are recommended can vary based on your presentation, goals, and your therapist’s assessment. Most typically this therapy is done 1 to 2 weeks with a minimum of 48 hours in between sessions.
Who should consider IASTM?
If this treatment is right for you, your physical therapist will suggest it as a part of your treatment program. IASTM can also be utilized for several pain conditions in the neck, back, feet, hands, and wrists, as well as in the joints such as the elbow, shoulder, knees, and ankles. IASTM is also very efficacious in addressing and reducing scar tissue.
What kind of tissue does IASTM work to break down?
The IASTM remedy is thought to stimulate connective tissue remodeling through resorption of excessive fibrosis, along with inducing repair and regeneration of collagen secondary to fibroblast recruitment. In turn, this will result in the release and breakdown of scar tissue, adhesions, and fascial limitations.
How effective is IASTM?
The study showed that IASTM with Graston Technique® and plantar fascia-specific stretching was effective in decreasing pain and improving foot function in patients with chronic plantar fasciitis. Participants were tested before and after treatment to determine the effect on foot pain, function, and health
What is the difference between Graston and IASTM?
IASTM includes a variety of instrument-based treatments, including cupping, Hawk Grips, the Fascial Abrasion Technique (FAT), and Graston. The Graston Technique, a method within IASTM, uses six stainless-steel tools to find and target scar tissue and promote movement and mobilization in injured areas.
Is IASTM evidence-based?
The available evidence on IASTM does not support its use to improve function, pain, or range of motion in individuals with upper body, lower body, and spinal conditions.





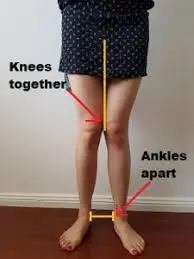
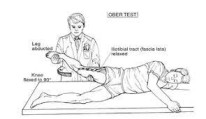

One Comment