Hamstring Muscle Strain
What is a Hamstring muscle strain?
Hamstring strains are caused by a fast extensive compacting or a forceful stretch of the hamstring muscle group which causes high mechanical stress. This results in differing degrees of rupture within the fibers of the musculotendinous branch.
Hamstring strains are typical in sports with dynamic qualities like sprinting, jumping, and communication sports such as Australian Rules football (AFL), American football, and soccer where fast eccentric contractions are regular. In soccer, it is the most frequent injury. Hamstring damage can also occur in recreational sports such as water skiing and bull riding, where the knee is strongly fully developed during injury.
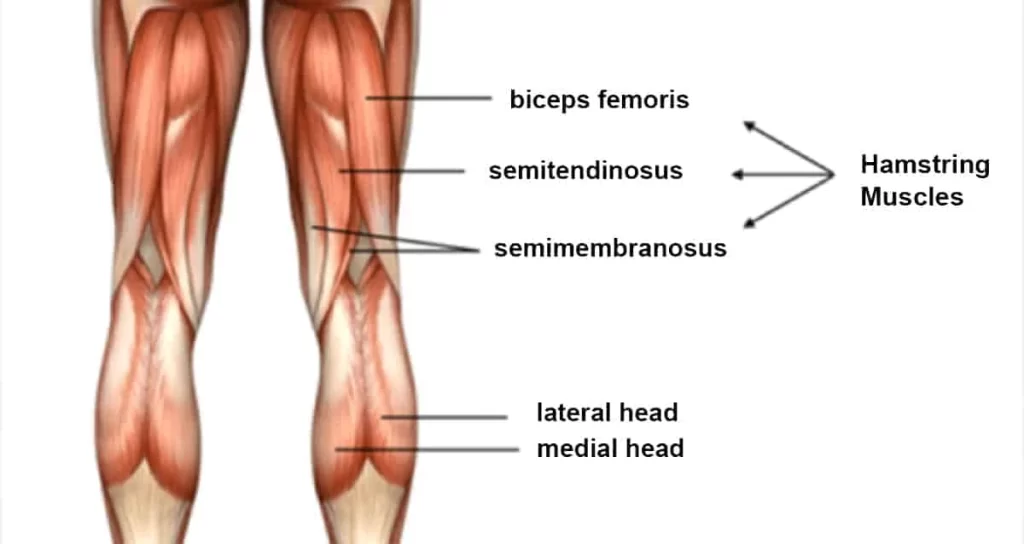
The hamstrings muscle are a group of three muscles:
- The biceps femoris
- The semitendinosus
- The semimembranosus
The biceps femoris:
Origin
Short head: lateral supracondylar line and linea aspera of the femur
Long head: ischial tuberosity
Insertion
Lateral aspect of the fibular head
Nerve Supply
Long head: tibial branch of the sciatic nerve (L5-S2)
Short head: common peroneal branch of the sciatic nerve
Blood Supply
Perforating departments of profound femoris, inferior gluteal, and medial circumflex femoral arteries
The semitendinosus
Origin
It occurs, from a common tendon origin with the long head of the biceps femoris, from the lower medial aspect of the lateral area of the ischial tuberosity. The semitendinosus muscle mainly originates from the medial surface of the tendon of the long head of the biceps femoris, and also arises from the ischial tuberosity with a thin tendon and a muscular part.
Insertion
The semitendinosus tendon inserts at the upper part of the medial surface of the tibia, behind the branch of the sartorius, and infero-anterior to the component of the gracilis.
Nerve Supply
The tibial part of the sciatic nerve (L5, S1, 2).
The semimembranosus.
Origin
A strong membranous tendon connects to the upper lateral facet on the rough region of the ischial tuberosity.
Insertion
The anatomy of the distal insertion of the semimembranosus can be defined as the distal semimembranosus complex: six separate semimembranosus insertions can be determined. Anatomic dissection showed six insertions of the distal semimembranosus tendon: direct arm, anterior arm, posterior oblique ligament extension, oblique popliteal ligament extension (capsular arm), distal tibial expansion (popliteus aponeurosis), and meniscal arm.
Nerve
Tibial section of the Sciatic Nerve (root value L5, S1, and 2).
The nerve supply for the skin wrapping the muscle is L2.
Artery
Branches from the internal iliac, popliteal, and profunda femoris arteries.
Epidemiology
In the second half of the swing phase, the hamstrings are at their most significant length, and at this point, they generate maximum tension. In this phase, hamstrings tighten eccentrically to decelerate flexion of the hip and extension of the lower leg. At this point, a peak is achieved in the movement of the muscle spindles in the hamstrings.
A strong contraction of the hamstring and relaxation of the quadriceps is required. According to “Klafs and Arnheim”, research in the coordination between these contrasting muscles can cause the hamstring to tears. The most significant musculo-tendon stretch is incurred by the biceps femoris, which may donate to its tendency to be more frequently injured than the other 2 hamstring muscles (semimembranosus and semitendinosus) during high-speed running.
Causes of a Hamstring strain
The major cause of injury to the hamstring is muscle overload. Strains and tears happen when the muscle is increasing as it contracts or shortens. They may also occur if the muscle is stretched too far or is taxed too unexpectedly.
When you run, for example, your hamstring muscles must contract frequently as your leg lengthens with your stride. All this lengthening and loading of the muscles makes a perfect environment for injury. You may feel anything from impulsive pain to a popping or snapping feeling in your leg. Your hamstring may feel tender and you might see bruising at the site of your injury.
There are several risk factors for hamstring strain:
Exercising with stretched muscles. Athletes who have extremely tight muscles may be more possible to experience injury.
Muscle imbalances, where individual muscles are stronger than others.
Poor activity. If the muscles are weak, they’ll be small and able to deal with the needs of specific sports or exercises.
Fatigue in the muscles, because tired muscles don’t absorb as much power.
Hamstring strain is generally seen in people who experience the following activities:
- football
- soccer
- basketball
- tennis
- running and sprinting, and other way events
- dancing
- Older athletes who walk as their immediate form of exercise are also at higher risk. So are adolescents whose bodies are still developing. Muscles and bones don’t necessarily grow at an identical rate. This means that any force or stress to the muscles, like a jump or impact, may leave them helpless to tearing.
Some of the more typical things that can donate to a hamstring strain include:
- Not heating up properly before exercising. Tight muscles are much more possible to strain than muscles that are maintained strong and flexible.
- Being out of the constitution or overdoing it. Weak muscles are less able to handle the stress of exercise, and muscles that are tired lose some of their capability to absorb energy, making them more likely to get hurt.
- An imbalance in the length of your leg muscles. The quadriceps, the muscles at the front of your legs, is often more extensive and more powerful than your hamstring muscles. When you do an activity that implicates running, the hamstring muscles can get tired more quickly than the quadriceps, putting them at a more significant risk of strain.
- Poor technique. If you don’t have good running practice, it can increase the stress on your hamstring muscles.
- Producing activities too quickly after an injury. Hamstring strains require plenty of time and rest to heal completely. Trying to come back from a strain too soon will make you more likely to hurt your hamstring again.
Symptoms of a Hamstring strain
A hamstring injury generally causes an impulsive, sharp pain in the back of the thigh. There might also be a “popping” or tearing sensation.
Swelling and tenderness generally form within a few hours. There might be bruising or a difference in skin color along the back of the leg. Some people have muscle deficiency or are not able to put weight on the injured leg.
Hamstring strain effects in sudden, minimal to intense pain in the posterior thigh. Also, a “popping” or tearing appearance can be described. Sometimes swelling and ecchymosis are viable but they may be delayed for several days after the injury occurs. Rare symptoms are numbness, tingling, and distal extremity deficiency. These symptoms require further examination into sciatic nerve irritation. Large hematoma or scar tissue can be caused by complete tears and avulsion damages.
Other likely symptoms: Pain, Tenderness, Loss of movement, Reduced strength on isometric contraction, Reduced length of the hamstrings
Hamstring strains are classified into 3 groups, according to the amount of pain, weakness, and loss of motion.
Grade 1 (mild): just a few fibers of the muscle are injured or have ruptured. This rarely affects the muscle’s power and endurance. Pain and sensitivity usually happen the day after the injury (depends on person to person). Normal patient complaints are stiffness on the posterior side of the leg. Patients can walk fine. There can be a small swelling, but the knee can still flex normally.
Grade 2 (medium): around half of the fibers are torn. Symptoms are acute pain, swelling, and a mild case of function loss. The walk of the patient will be affected. Pain can be produced by applying accuracy on the hamstring muscle or flexing the knee against resistance.
Grade 3 (severe): varying from more than half of the fibers ruptured to complete rupture of the muscle. Both the muscle belly and the tendon can suffer from this damage. It generates massive swelling and pain. The function of the hamstring muscle can’t be accomplished anymore and the muscle shows great weakness.
Risk Factors of a Hamstring strain
Different suggested risk factors may play a part in hamstring injuries:
- Older generation
- Earlier hamstring injury
- Determinate hamstring flexibility
- Expanded fatigue
- Poor core strength
- Strength imbalance
- Ethnicity
- Earlier calf injury
- Earlier significant knee injury
- Osteitis pubis
- Raised quadriceps flexibility was inversely associated with a hamstring strain
- Players showing specific polymorphisms, IGF2 and CCL2 (especially its allelic form GG), might be more helpless to severe injuries and should be involved in specific deterrence schedules
- Tight hip flexors
- Previously associated lumbar spine anomalies. Kicking and conducting abdominal strengthening exercises with straight legs have been identified as possible contributory causes of lordosis. The anatomical reason appears to be that the iliopsoas muscle group is mainly involved in kicking and straight leg raising or straight leg sit-up exercises and donates to strengthening this muscle. Therefore, specific athletic activities and training methods that exacerbate postural deficiencies may also predispose the party to injury.
During exercises like running and kicking, the hamstring will lengthen with contemporary hip flexion and knee extension, this lengthening may reach the mechanical limits of the muscle or lead to the collection of microscopic muscle damage. There is a possibility that hamstring injuries may arise secondary to the potential ungainly contraction of the biceps femoris muscle resulting from double nerve supply.
Another argument is on hamstring variation in muscle architecture. The short head of biceps femoris(BFS) maintains longer fascicles (which allow for greater muscle extensibility and decrease the risk of over-lengthening during eccentric contraction) and a much smaller cross-section area compared to the long head of biceps femoris(BFL). Whereas BFL presents with shorter collections compared to BFS which undergoes repetitive over-lengthening and collected muscle damage.
Exaggerated anterior pelvic tilt will place the hamstring muscle group at longer lengths and some studies suggested that this may raise the risk of strain injury.
Differential Diagnosis
On examining the patient, the physiotherapist conceivably has to determine between different injuries e.g.
adductor strains, avulsion damage, lumbosacral directed pain syndrome, piriformis syndrome, sacroiliac dysfunction, sciatica, Hamstring tendinitis, and ischial bursitis.
Other origins of posterior thigh pain could also be complicated by hamstring strains and should be evaluated during the examination process. Specific tests and imaging are used to assess and ban those different pain source chances.
Sciatic nerve mobility restrictions can contribute to posterior thigh pain and negative neural tension could in some cases be the only source of pain without any particular muscular damage. In certain cases, it is challenging to determine whether it is the
Hamstrings or other muscle groups like hip adductors Gracilis are impaired due to their immediacy. Sometimes imaging techniques may be required to determine the precise location of the injury.
Other conditions with similar expressions as hamstring strains are strained popliteus muscle, tendonitis at either origin of the gastrocnemius, sprained posterior cruciate ligament, apophysitis-pain in ischial tuberosity, Lumbar spine diseases and lesions of the upper tibiofibular joint.
Diagnostic Procedures
Most acute damages can easily be found by letting the patient tell how the injury happened. To be sure they must do a little research on the hamstrings as well.
Radiographs: a good thing about radiographs is that with that kind of imaging, it’s possible to determine the etiology of the pain. It can differentiate into a muscular disorder (e.g muscle strain) or a disorder of the bone (e.g. Stress fracture).
Ultrasound(US): this kind of imaging is used a lot because it is an affordable method. It is also a good method because it can image muscles dynamically. A negative point about Ultrasound is that it needs a skilled and trained clinician.
Magnetic Resonance Imaging (MRI): MRI gives an exact view of muscle injury. But occasionally it may not be clear according to the images.
MRI study was done to differentiate between two main groups of muscle injuries: Injury by Direct or Indirect trauma.
Within the group of damages due to indirect trauma, the classification brings the concept of functional and structural lesions. Functional muscle injuries present alterations without macroscopic proof of fiber tear. These lesions have multifactorial reasons and are grouped into subgroups that image their clinical origins, such as overload or neuromuscular disorders. Structural muscle injuries are those whose MRI study presents macroscopic evidence of fiber tear, i.e., structural damage. They are usually encountered in the Musculotendinous junction, as these areas have biomechanical vulnerable points. Some studies strained patients after hamstring damage and they concluded that normalization of this increased signal power in MRI seems not needed for a successful return to play (RTP).
Examination of Hamstring muscle strain
Running gait: The physical analysis begins with an examination of the running gait. Patients with a hamstring strain generally show a shortened walking gait. Swelling and ecchymosis existed always noticeable at the initial stage of the injury because they often occur several days after the initial injury.
Observation: The physical test also exists for visible examination. The posterior thigh is examined for asymmetry, swelling, ecchymosis, and deformation.
Palpation: Palpation of the posterior thigh is useful for determining the specific region injured via pain stimulation, as well as specifying the presence/absence of a palpable defect in the musculotendon unit. With the patient placed pronely, repeated knee flexion-extension movements without resistance through a small range of motion may help in determining the location of the individual hamstring muscles and tendons. With the knee carried in full extension, the point of maximum pain with palpation can be selected and located relative to the ischial tuberosity, in addition to measuring the total length of the painful region. The total length, width, and distance between the ischial tuberosity and the area with maximal pain are estimated in centimeters. While both of these actions are used, only the location of the point of maximum pain (relative to the ischial tuberosity) is associated with the convalescent period. That is, the more proximal the site of maximum pain, the greater the time needed to return to the pre-injury level. The proximity to the ischial tuberosity is believed to deliberate the extent of involvement of the proximal tendon of the injured muscle, and therefore a more significant healing period.
Range of motion: Range of motion tests should assume both the hip and knee joints. Passive straight leg raise (hip) and active knee extension test (knee) are commonly used in sequence to estimate hamstring flexibility and greatest length. Typical hamstring length should allow the hip to flex 80° during the passive straight leg raise and the knee to extend to 20° on the active knee extension test.61 When considering post-injury muscle length, the extent of joint motion, in general, should be based on the onset of discomfort or stiffness reported by the patient. In the acutely disabled athlete, these tests are often limited by pain and thus may not provide an accurate estimation of musculotendon extensibility. Once again, a bilateral comparison is suggested.
Hip flexibility: The hip flexion test merged a passive unilateral straight leg raise test (SLR) with pain estimation according to the Borg CR-10 scale. The sprinters were positioned supine with the pelvis and contralateral leg fixed with straps. A common flexometer was placed 10 cm cranial to the base of the patella. The foot was plantar flexed and the researcher slowly(approximately 30 degrees) raised the leg with the knee straight until the subject assessed a 3 (“moderate pain”) on the Borg CR-10 scale (0 = no pain and 10 = maximal pain). The hip flexion angle at this point was recorded, and the most significant angle of three repeats was taken as the test result for Range of Motion (ROM). The importance of the injured leg was represented as a percentage of the undamaged leg for comparisons within and between groups. No warm-up forewent the flexibility measures.
Knee flexion strength: Isometric knee flexion power was assessed with the sprinter in a prone position and the pelvis and the contralateral leg fixed. A dynamometer was positioned at the ankle, perpendicular to the lower leg. The foot was in plantar flexion and the knee was in an extended position. Three maximal voluntary isometric knee flexion compactions were performed, each with gradually increasing effort. Each contraction lasted 3 s with 30 s of rest in between. The highest force value was taken as the test result for power. Attempts to bias the medial or lateral hamstrings by internal or external rotation of the lower leg, respectively, during strength testing, may help in the resolution of the involved muscles.
Treatment of Hamstring muscle strain
Medical Treatment
Surgical intervention is an incredibly rare procedure after a hamstring strain. Only in case of a complete rupture of the hamstrings, surgery is suggested. Almost all patients thought that they had improved with surgery. A study shows that 91% were satisfied after surgery and rated their satisfaction at 75% or better. Hamstring constancy tests and hamstring strength tests were better and highly achieved after a surgical procedure. The muscle strength testing after surgery ranged from 45% to 88%. The hamstrings endurance testing ranged from 26% to 100%. The physical assessment and follow-up show that all repairs stayed unchanged.
Physiotherapy Treatment
Pain relief
Utilize the RICE formula as soon as possible after the injury:
Rest. Limit the amount of walking you do, and try to avoid putting weight on your leg if your doctor suggests this.
Ice. Use a bag of ice or a cold compress to help reduce swelling for the first 48 hours after the injury. This should start as soon as possible after the injury and then every 3 to 4 hours for 20 to 30 minutes at a time until the swelling is gone. Wrap the ice or ice pack in a towel. Don’t put ice or ice packs directly on the skin because it can lead to tissue damage.
Compress. Use elastic bandages or sports wraps to support your leg and keep the swelling down if your doctor suggests doing so. Doctors suggest using elastic compression bandages rather than compression shorts because you can change the bandages as needed.
Elevate. When you are sitting or lying down, maintain your leg elevated.
Elevation. Try to maintain your leg supported on a pillow to limit swelling.
OTC pain medications may help ease your pain with a hamstring injury. Oral nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Motrin, Aleve), or another OTC pain drug like acetaminophen (Tylenol), may be useful for short-term relief.
Topical NSAID lotions or gels can also help ease the pain. If you feel you have hurt yourself severely, though, it’s a good idea to see your doctor before self-medicating.
Another option for pain relief affects using a foam roller to apply what’s called myofascial release to your hamstrings. Put the roller just above the back of your knee and roll upward in the direction of blood flow to massage the muscles. Experienced sports massage may also help with your pain.
The primary goal of physical therapy and the rehabilitation program is to restore the patient’s procedures to the highest possible degree and/or to replace the athlete to sport at the former status of performance and this with minimal risk of re-injury.
Hamstring strain damage stay a challenge for both athletes and clinicians, given their high incidence rate, slow healing, and persistent symptoms. Moreover, nearly one-third of these injuries recur within the first year following recovery to sport, with subsequent injuries often being more powerful than the original. The use of a specific and acceptable training program to rehabilitate hamstring strains can be a determinant for the recovery and prevention of a recurrent hamstring strain injury. Various kinds of treatments are used to rehabilitate hamstring strains, but are they all sufficient sufficiently to prevent a recurrence within the first year following a return to sport? Further studies tried to show the result of eccentric exercises, dry needling, deep stripping massage, etc. on hamstring strain rehabilitation.
The use of eccentric strengthening, at long muscle length exercises, as a rehabilitation tool was used to analyze the effects to contain a recurrence of hamstring injury following the revalidation. The results showed that the use of eccentric strengthening activities on long muscles had a positive effect.
On the other hand, a study attempted to compare eccentric strengthening exercises (STST) with developed agility and trunk stabilization exercises (PATS). The rehabilitation of the STST group consisted of static stretching, isolated progressive hamstring resistance exercises, and icing. The PATS group consisted of progressive dexterity and trunk stabilization exercises and icing as treatment. The study found a particularly better outcome in patients that were rehabilitated with progressive agility and trunk stabilization. The reinjury speed was significantly lower in the PATS group after one year of producing to sport (1 of the 13 athletes instead of 7 of the 11 athletes in the STST group). A rehabilitation program consisting of progressive agility and trunk stabilization exercises is more useful than a program emphasizing isolated hamstring stretching and strengthening in promoting the return to sports and preventing injury reproduction in athletes suffering an acute hamstring strain.
Deep stripping massage is another method used as rehabilitation for hamstring strain injury. Most of the time it is connected with other rehabilitation techniques. Deep stripping massage (DSMS) alone or with eccentric antagonism was used to analyze the effect on hamstring length and strength. These results indicate that DSMS increases hamstring length in less than 3 min but has no impact on strength. Furthermore, combining DSMS with eccentric resistance has more hamstring flexibility gains than DSMS alone and does not involve strength.
Functional dry needling is a method that has been reported to be useful in the management of pain and dysfunction after muscle strains and in combination with an eccentric training program, but there is limited disseminated literature on its effects on rehabilitation or reproduction of injury.
The impact of kinesiology tape has been indicated to be efficient at improving muscle flexibility, which can prevent or enhance the risk of damage.
There are lots of methods and programs that can be used for the revalidation of hamstring strain injuries but due to a lack of studies, the significance of these procedures can not all be demonstrated. Therefore eccentric exercises are the most known and used program for the rehabilitation of hamstring strain injuries. The use of this kind of program has shown good effects. One common objection to rehabilitation programs that emphasize eccentric strength exercise, is the lack of attention to musculature adjacent to the hamstrings. It has been indicated that neuromuscular control of the lumbopelvic region is required to enable optimal functioning of the hamstrings during regular sporting movements.
Rehabilitation Exercises for hamstring strain
You can begin gently stretching your hamstring directly away by doing the standing hamstring stretch. Make sure you do not feel any intense pain, only mild pain in the back of your thigh when you are accomplishing this stretch.
Standing hamstring stretch
Put the heel of your injured leg on a stool about 15 inches high. Keep your knee straight. Lean forward, flexing at the hips until you feel a gentle stretch in the back of your thigh. Make sure you do not roll your shoulders and flex at the waist when doing this or you will stretch your lower back rather than your leg. Hold the stretch for 15 to 30 seconds. Repeat 3 times.

Hamstring stretch on wall:
Lie on your back with your buttocks near a doorway, and your legs straight out in front of you along the floor. Lift one leg and rest it against the wall next to the door frame. Your other leg should rise via the doorway. Feel a stretch in the back of your thigh. Hold this position for 15 to 30 seconds. Repetition 3 times and then change legs and do the exercise again.

Standing calf stretch:
Facing a wall, place your hands against the wall at eye level. Maintain one leg back with the heel on the floor, and the further leg forward. Rotate your back foot slightly inward (as if you were pigeon-toed) as you slowly bend into the wall until you feel a stretch in the back of your calf. Hold for 15 to 30 seconds. Repetition 3 times and then change the position of your legs and then repeat the exercise 3 times. Do this activity several times each day.

Prone knee bend:
Lie on your stomach with your legs instantly out behind you. flex your knee so that your heel reaches toward your buttocks. Hold 5 seconds. Relax and return your foot to the floor. Do 3 sets of 10. As this evolves easier you can add weights to your ankle.

Prone hip extension:
Lie on your stomach with your legs directly out behind you. Tighten the buttocks and thigh muscles of your injured leg and lift it off the floor approximately 8 inches. Keep your knee straight. Hold for 5 seconds. Then lower your leg and relax. Do 3 sets of 10.

Resisted hamstring curl:
Sit in a chair facing a door (about 3 feet from the door). Loop and connect one end of the tubing near the ankle of one leg. Tie a knot in the other end of the tubing and closed the knot in the door. Flex your knee, bringing your foot down to the floor, and allow your foot to slide along the floor and move back beneath the chair, stretching the tubing. Slowly let your foot slide forward again. Do 3 sets of 10.

Chair lift:
Lie on your back with your heels relaxing on the top of a chair. Slowly lift both hips off the floor. Hold for 2 seconds and lower slowly. Do 3 sets of 15.
Lunge:
Stand and take a large step forward with your good leg. Drop your left knee down toward the floor and flex your right leg. Back to the starting position. Repeat the exercise, this time stepping forward with the left leg and dropping the leg on your right side down. Do 3 sets of 10 on each side.
Rehabilitation Protocol
Phase I (weeks 0-3)
Goals
Cover healing tissue
Minimize atrophy and strength losing
Control motion loss
Precautions
Avoid extreme active or passive lengthening of the hamstrings
Avoid antalgic gait pattern
Rehab
Ice – 2-3 times daily
Standing bike
Sub-maximal isometric at 90, 60 and 30
Single leg balance
Painfree isotonic knee flexion
Balance board
Soft tissue mobs/IASTM
Progressive hip strengthening
Pain-free isometric contraction against submaximal (50%-75%) resistance during prone knee flexion at 90.
Active sciatic nerve flossing
Conventional TENS
Criteria for progression to the next phase
Pulsed ultrasound (Duty cycle 50%, 1 MHz, 1.2 W/cm2)
Normal walking stride without pain
Phase 2 (weeks 3-12)
Goals
Regain pain-free hamstring strength, moving via full ROM
Generate neuromuscular control of the trunk and pelvis with progressive growth in movement and speed training for functional motions
Precautions
Avoid end-range extension of the hamstring if painful
Rehab
Ice – post-exercise
Nordic hamstring Ex
Treadmill at moderate to high-intensity pain-free speed and stride
Prone leg dropsIsokinetic eccentrics in the non-lengthened state
Single limb balance windmill touches without weight
Single leg stance with perturbations
Supine hamstring curls on theraball
STM/IASTM
Shuttle jumps
Eccentric protocol
Stationary bike
The lateral and retro band walks
Sciatic nerve tensioning
Criteria for progression
Greatest strength 5/5 without pain during prone knee flexion at 90
Pain-free forward and backward, jog, moderate-intensity
Strength deficiency is less than 20% compared to the undamaged limb
Pain-free max strange in a non-lengthened state
Phase 3 (week 12+)
Goals
Symptom-free during all movements
Normal concentric and eccentric strength through full ROM and speed
Enhance neuromuscular control of the trunk and pelvis
Combine postural control into sport-specific motions
Precautions
Train within the symptoms-free intensity
Rehab
Ice – Post-exercise – as required
Treadmill medium to high power as tolerated
Isokinetic eccentric exercise at end ROM (in hyperflexion)
STM/IASTM
Plyometric jump training
5-10 yard accelerations/downshift
Single-limb balance windmill connects with weight on an unstable surface
Sport-specific drills that include postural control and developed speed
Eccentric protocol
Maintain higher velocity eccentric movements that include plyometrics and sports distinctive activities
Examples: include squat jumps, split jumps, bounding and depth jumps, single leg bounding, backward skips, lateral hops, lateral bounding, zigzag hops, bounding, plyometric box jumps, eccentric backward steps, eccentric lunge drops, abnormal forward pulls, single and double leg deadlifts, and split stance deadlift
Return to sports criteria
Full strength without pain in the increased state testing position
Bilateral balance in knee flexion angle of peak torque
Full ROM without pain
Replication of sport-specific motions at contest speed without symptoms.
Isokinetic strength testing should be conducted under both concentric and eccentric motion conditions.
Prevention of Hamstring strain
Not all hamstring strains can be controlled. You may be in a higher-risk group, like an older adult or an adolescent, or understanding a sudden effect that causes injury. Regular stretching and strengthening activities may help you lower your risk of hamstring strains.
Following are some general prevention tips:
- Warm up before performing or playing sports, and cool down afterward.
- Exercise regularly to maintain cardiovascular and muscular fitness. Doing so will help you control injuries related to fatigue.
- Spend time stretching and strengthening muscles in your weekly training routine. Doing so will help prevent muscular imbalances that may cause damage.
- Take days off or have easy days between extremely hard physical sessions to give your body sufficient rest.
- Try adding speed work to your routine to train hamstring muscles for the types of forces that may lead to injury.
FAQ
How long does a strained hamstring assume to heal?
Mild to moderate (grade 1 or 2) tears or strains can recover within three to eight weeks with occupied home therapy. For a grade 3 hamstring tear or strain, healing may be as long as three months. Replacing to sports before the injury is fully recovered can cause more intense injuries.
Should you stretch a hamstring strain?
Active Hamstring Stretch
At the point where a mild stretch is supposed to pause and hold. The stretch should not be painful. Mild stretching is helpful for healing. Forceful stretching of your hamstring will slow your recovery.
How can I speed up my hamstring recovery?
The most significant factor in healing your hamstring fast is resting the muscle. It is important that you do not rush back into exercising, but that you gradually ease into using the hamstring muscle more and more during the healing period. To Heal Faster, You May Also: Ice your leg to relieve pain and swelling.
Should you massage a hamstring injury?
If you have continued hamstring tightness, pain, and discomfort “shin splints”, “runner’s knee” or an acute hamstring strain, you may need a soft, early intervention physiotherapy massage session to help relieve the pain and speed up the healing process
How long does a sore hamstring last?
A Grade 1 hamstring strain is a moderately mild muscle pull that commonly heals in anywhere from a few days to a couple of weeks. Grade 1 strains usually cause some light pain and tenderness at the back of the thigh, making it tough to move. That being said, the hamstring muscles’ strength should be natural.
Can sitting cause hamstring pain?
Discomfort or pain when sitting down, specifically if it gets worse after sitting for a long time. Pain that is activated or aggravated by an activity that involves repetitive leg motion, particularly running or biking. The pain may even start at the same point in the movement.





3 Comments