Manual Physical Therapist
Description
Manual therapy, or manipulative therapy, is a physical treatment primarily used by physical therapists, physiotherapists, and occupational therapists to treat musculoskeletal pain and disability; it mostly includes kneading and manipulation of muscles, joint mobilization, and joint manipulation. It could also be used by Rolfers, massage therapists, athletic trainers, osteopaths, and physicians. Manual therapy has a prolonged history within the profession of physical therapy and physical therapists hold greatly contributed to the current diversity in manual therapy approaches and techniques. Mechanical explanations were historically used to describe the mechanisms by which manual therapy interventions are performed. Contemporary research reveals complex neurophysiologic mechanisms are even at play and the beneficial psychological effects of providing hands-on examination and intervention have been substantiated.
The International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) defines orthopedic manual physical therapy as: “a specialized area of physiotherapy or a Physical Therapy for the management of neuromusculoskeletal (NMS) conditions, based on clinical reasoning, using highly specific treatment approaches consisting manual techniques and therapeutic exercises. Orthopedic Manual Therapy also encompasses, and is driven by, the available scientific or clinical evidence and the biopsychosocial framework of every individual patient.” According to the American Academy of Orthopaedic Manual Physical Therapists (AAOMPT) Description of Advanced Specialty Practice (DASP) (2018), orthopedic manual physical therapy (OMPT) is defined as: “an advanced specialty area of physical therapy practice that is based on manual examination and treatment techniques integrated with exercise, patient education, or another physical therapy modalities to address pain, loss of function, and wellness.
Early, consistent, and skillful manual physical therapy, combined with exercise and/or patient education, is central to the Orthopedic MPT therapist’s practice. Advanced examination, communication, and decision-making skills are built on the foundations of professional and scientific education to facilitate the provision of effective and efficient care. Practitioners of Ortho MPT provide patient management, consult with other health care providers regarding simple as well as complex neuromusculoskeletal (NMS) conditions, and provide recommendations and interventions in the area of health and wellness.”
What is a manual physical therapist?
The American Physical Therapy Association (APTA) defines manual therapy techniques as “skilled hand movements and/or skilled passive movements of joints and soft tissue.” In another word, it’s physical therapy that employs the practitioner’s hands rather than machines. These techniques can be used to improve the range of motion and tissue extensibility, mobilize or manipulate soft tissue and joints, control pain, reduce soft tissue swelling, inflammation, or restriction, and induce relaxation.
Before prescribing manual therapies, a doctor or a physical therapist will take into account several factors surrounding the patient’s condition, medical history, and outpatient care, according to the American Physical Therapy Association. Factors that might influence decisions involving physical therapy comprise age, comorbidities, social support, the primary caregiver’s expertise, the condition’s stability, and environmental factors such as living situations. These factors impact the types of physical therapy a patient might undergo, as well as whether the patient can or should undergo physical therapy at all.
Benefits of Manual Therapy
- It can Modulate pain
- Increase joints mobility to stiff joints and range of motion
- Improve tissue repair
- Improving tissue stability and extensibility
- Reduce soft-tissue inflammation
- Reduce muscle tension
- Induce relaxation
- Facilitate movement and exercise therapy
Three Paradigms for Manual Therapy Therapeutic Effects
- Physiological: positive placebo response
- Biomechanical and Physical: facilitates repair and tissue modeling
- Psychological: pain relief via stimulates the pain gating mechanism; muscle inhibition; reduction of nociceptive activity; decreased intraarticular or periarticular pressure.
Manual Therapy Frameworks
Cyriax
- System of Prescription: The problem is either caused by a joint, a muscle, or a nerve
- Area: Spine and peripheral joints:
- Treatment Methods: Deep transverse friction or traction and manipulation techniques:
Lewit Manual therapy
- System of Prescription: Viewed as a chain of the interrelated pathologies
- Area: Spine and peripheral joints
- Treatment Methods: Mobilizing, manipulating, and actively exercising
Kaltenborn Evjenth manual therapy
- System of Prescription: Specialized manual tests to determine whether the source of pain is an intense muscle, an irritated nerve, or a degenerated joint:
- Area: Spine and joint
- Treatment Methods: Transverse massage, functional massage, post-isometric relaxation, joint mobilization, joint manipulation, and neuro mobilization
Mckenzie manual therapy
- System of Prescription: Therapy to heal the spine through an active, an active assisted, and/or passive patient movements
- Area: Spine
- Treatment Methods: The therapist and the patient are looking for the direction of the movement that brings a relevant improvement after a few repetitions.
Maitland manual therapy
- System of Prescription: Joints, muscles, and nerve tissue in both the spine and peripheral joints.
- Area: the foremost important thing is not to discover the immediate cause of the dysfunction, but to observe the symptoms and apply the best therapeutic technique: Also looks to solve a given functional problem by eliminating pain sensations, restoring proper mobility in the joint, and normalizing the muscle tension.
- Treatment Methods: The Rhythmic, passive, painless movements introduced into the tissue (mobilizations) and rapid movements (manipulations)
Mulligan manual therapy
- System of Prescription: Mulligan’s therapy is based on active patient movements combined with the passive correction of the joint position held by a physiotherapist.
- Area: Spine, and limbs, primarily to address pathologies affecting the periphery
- Treatment Methods: Painless, functional loading of the articular surfaces within the force of gravity. A Combining passive movement in the plane of the articular surfaces with active movement. By exerting overpressure at the end of the painless movement range. Applying an appropriate number of repetitions.
Manual Therapy Application Framework
- Speed
- Location within ROM
- Force direction – Anatomical and/or Biomechanical
- Relative Movement (anatomical or positional)
- Subject Position (both limb and gross)
What is the difference between Maitland and Mulligan?
Mulligan mobilization allows a patient to perform the offending movements in a functional position. hence, leading to a rewarding outcome. The Maitland mobilization aims to reestablish the spinning, gliding, and rolling motions of the two joints.
The primary two items (speed and location within ROM) feature heavily in Manual Therapy grading guides. Including the two guides discussed below (Maitland and Kaltenborn).
Types of Manual Therapy Techniques
Physical therapists have many manual therapy techniques at their disposal, each of which targets different types of the body and a range of conditions. The manual therapy includes :
- Integrative Manual Therapy (IMT)
- Myofascial Release
- Muscle Energy Technique (MET)
- Neural Tissue Tension Techniques
- Strain Counterstrain
- Positional Release Therapy
- Craniosacral Therapy
- Lymphedema and Manual Lymphatic Drainage (MLD)
- Range of Motion
- Manual Stretching
- Proprioceptive Neuromuscular Facilitation (PNF)
- Mobilization with Movement
- Active Release
- Manual Traction
- Trigger Point Therapy
- Instrument-Assisted Soft Tissue Massage (IASTM)
- Cupping Therapy
- Dry Needling
- chiropractic therapy
- massage
- joint manipulation and mobilization
- taping
- acupressure
- acupuncture
- bobath concept
- osteopathy
- MacKenzie method
Integrative Manual Therapy (IMT)
Integrative Manual Therapy is a specific type of manual therapy developed by Dr. Sharon Weiselfish Giammatteo, Ph.D., PT, IMT-C. IMT uses a conglomeration of various manual therapy theories, techniques, and methodologies to address pain and dysfunction and assist the body to heal itself. With a holistic approach to physical therapy, IMT practitioners sense blockages in body systems and work to guide your tissues to clear those impairments and restore optimal function.
Myofascial Release
Myofascial release (MFR, self-myofascial release) is an alternative medicine therapy claimed to be useful for the treatment of skeletal muscle immobility and pain by relaxing contracted muscles, improving blood and lymphatic circulation, and/or stimulating the stretch reflex in muscles. Fascia is a thin, tough, elastic type of connective tissue that wraps most structures within the human body, and comprises the muscle. Fascia supports and protects these structures. The osteopathic practice holds that this soft tissue may become restricted due to psychogenic disease, overuse, trauma, infectious agents, or inactivity, often resulting in pain, muscle tension, and corresponding diminished blood flow.
Fascia is fibrous connective tissue around the muscles, vessels, and nerves, giving the body shape and form. Fascia is made up of densely packed bundles of collagen. Some types of fascia bind structures together and other areas of fascia are meant to glide smoothly over each other allowing the body to move. When areas of fascia that are meant to glide become adhered, or stuck, a Myofascial Release is a technique of manual therapy that releases those adhesions and restores gliding motion to the underlying tissues. Myofascial Release uses gentle, sustained pressure to mobilize the connective tissue or to relax contracted muscles, and increase blood and oxygen circulation to the tissues.
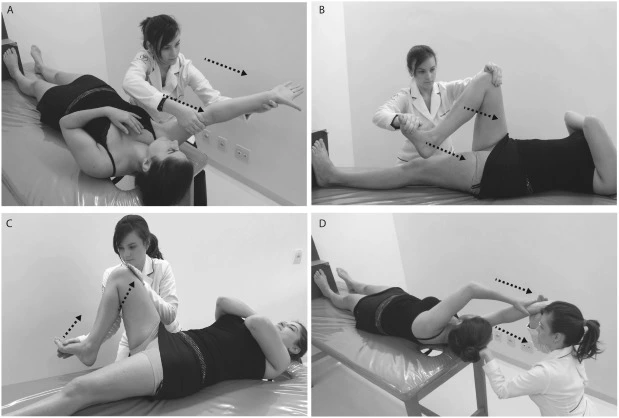
Muscle Energy Techniques (MET)
Muscle Energy Techniques (METs) describe a broad class of manual therapy techniques directed at improving musculoskeletal function and joint function and improving pain. METs are commonly used by manual therapists, physical therapists, occupational therapists, chiropractors, athletic trainers, osteopathic physicians, and massage therapists. Muscle energy is required for the patient to actively use his or her muscles on request to aid in treatment. Muscle energy techniques are used to treat somatic dysfunction, especially reduced range of motion, muscular hypertonicity, and pain.
Mechanism of action for muscle energy techniques
Muscle energy is a direct and active technique; which means it engages a restrictive barrier or requires the patient’s participation for maximal effect. A restrictive barrier that describes the limit in the range of movement prevents the patient from being able to reach the baseline limit in his range of motion. As the patient performs an isometric contraction, the following physiologic alteration happen are as follows: Golgi tendon organ activation leads to direct inhibition of the agonist’s muscles. A reflexive reciprocal inhibition happens at the antagonistic muscles. As the patient relaxes, the agonist and the antagonist’s muscles remain inhibited allowing the joint to be moved further into the restricted range of motion. Despite the varied claims made regarding the efficacy of these techniques, there are only two peer-reviewed studies that have shown that muscle energy techniques might significantly decrease disability and improve functionality in patients with the disorders such as low back pain.
Pathophysiology – Injury could also occur as a result of trauma, accidents, overuse, strain, sprain, etc., not all of which should be treated within muscle energy. These techniques are most appropriate for the subsequent injury patterns: The reduced range was of motion secondary to muscular spasticity, rigidity, hypertonicity, or hypotonicity. Hypertonicity commonly follows overuse and can result in altered joint position, increased irritability, and decreased elasticity. This injury pattern is frequently accompanied by a non-specific muscle ache in the area of injury. In interneuronal injury, when dysfunction occurs at one joint or segment, the related agonist muscles also are affected. If uncorrected, the antagonistic muscles eventually get involved as well, leading to the dysfunction of both muscle groups. This presents as a decreased range of motion with pain and/or tenderness in the area.
Indications and contraindications – Muscle energy techniques could be employed to reposition a dysfunctional joint and treat the affected musculature. Indications include, but are not limited to muscular shortening, low back pain, pelvic imbalance, edema, limited range of motion, somatic dysfunction, respiratory dysfunction, cervicogenic headaches, and lots of others.
These techniques are inappropriate when a patient has injuries such as fractures, open wounds, avulsion injuries, severe osteoporosis, or metastatic disease. In addition, because these techniques need active patient participation, they are inappropriate for any patient that is unable to cooperate.
Techniques
Muscle energy techniques may be applied to most areas of the body. According to one textbook, each technique requires 8 essential steps: 4
Perform and obtain an accurate structural diagnosis. Engage the restrictive barrier in as numerous planes as possible. The Physician and patient engage in an unyielding counterforce where the patient’s force matches the physician’s force. The patient’s isometric contraction has the correct amount of force, the correct direction of effort (away from the restrictive barrier), and the correct duration (5 to 10 seconds).
Complete relaxation occurs after the muscular effort. The patient is repositioned into the new restrictive barrier in as numerous planes as possible. Steps 3 to 6 are repeated approximately 3 to 5 times or until no further improvement in range of motion is observed.
The structural diagnosis is repeated to judge if the dysfunction has resolved or improved.
Types
There are many different types of muscle energy techniques:
- Post-Isometric relaxation: Treat by engaging the restrictive barrier in many planes.
- Reciprocal inhibition: Treat by contracting the antagonistic muscles, which leads to the agonist’s muscle to relax through the reciprocal inhibition reflex arc.
- Joint mobilization using muscle force: Use muscle contraction to restore the range of motion in a joint.
- Oculocephalogyric reflex: Treat cervical or truncal muscles by using extraocular muscle contraction.
- Respiratory assistance: Use the patient’s voluntary respiratory motions to treat somatic dysfunction. Generally used in treating inhalation rib dysfunctions.
- Crossed extensor reflex: Use crossed extensor reflex to treat a muscular injury. For example, the contraction of a muscle on the right side leads to the relaxation of the same muscle on the left side.
If one of your joints is too stiff or not moving well, then a muscle energy technique can help that area of your body move a little more smoothly. Your therapist will position you in a particular way and instruct you to gently squeeze and relax specific muscles. This kind of isometric contraction uses the muscle’s own energy to release the tension and lengthen the muscle. Muscle Energy Technique may make stretching more effective.
Neural Tissue Tension Techniques
There are 37 miles (60 km) of the nerves in the human body, continuously sending signals to your spinal cord and brain. These nerves are surrounded by connective tissue and another structure. If a nerve gets “stuck”, or adheres to a structure nearby, that may send a pain signal to your brain or limit your ability to move that part of your body. Neural tissue tension techniques are used to release the tension, adhesions, or “stuck” nerves, restoring optimal function.
Strain Counterstrain, or Positional Release Therapy
When you have a muscle spasm and one of your muscles is too tight, too short, overactive, and would not let go, then your therapist may put you in an optimal position for that muscle and/or guide you through relaxation and breathing while that muscle unwinds, softens, relaxes, and lengthens.
Craniosacral Therapy
Your Cerebrospinal Nervous System is your brain and your spinal cord. It is surrounded by fluid and membranes. When those membranes have tension in them, stick with structures around them, or produce other dysfunction, it affects the fluid flow. If the membranes and fluid are not gliding and flowing optimally, it may affect your nervous system function, causing symptoms like headaches and neck and back pain. Craniosacral Therapy uses very kindly hands-on pressure to release tension and improve fluid flow, allowing your body to self-heal and calm the nervous system.
Manual Lymphatic Drainage
Manual Lymphatic Drainage might be a highly specialized form of manual therapy for people who have Lymphedema. Manual lymphatic drainage (MLD) could even be a type of massage based on the hypothesis that it will encourage the natural drainage of the lymph, which carries waste products far away from the tissues or may go back toward the heart. The lymph system depends on intrinsic contractions of the smooth muscle cells in the walls of lymph vessels (peristalsis) and/or the movement of skeletal muscles to propel lymph through the vessels to lymph nodes and then to the lymph ducts which goes back lymph to the cardiovascular system. Manual lymph drainage uses a selected amount of pressure (less than 9 ounces per square inch or about 4 kPa) and rhythmic circular movements to stimulate lymph flow.
Passive and Active-Assistive Range of Motion
Each joint in the human body has an arc or range of motion through which it can be moved. When there is injury or dysfunction, that range is commonly reduced. Your range may be impaired because of pain, stiffness, scar tissue, adhesion, muscle imbalance, altered biomechanics, or other reasons. Your therapist might glide your joint passively, where they do the movement for you, or actively, where you and your therapist do the movement together. These techniques can reduce pain and improve the range of motion of the joint.
Manual Stretching
Regular stretching could also improve your flexibility and your range of motion. When appropriate, your therapist might perform stretching techniques including static stretching, dynamic stretching, pre-contraction stretching, and highly skilled Proprioceptive Neuromuscular Facilitation. Different Stretches for Different Situations.
- Active Stretching – Active stretching involves holding a pose to use a targeted muscle group. For instance, an overhead stretch can target your shoulders, chest, forearms, and lats. Active stretching is often performed as a warm-up to prepare the muscles for exercise.
- Passive Stretching – This type of stretching is best for balance enhancement and flexibility. For instance, stretching your hamstrings by bending over and stabilizing your legs may foster flexibility by staying in that position for a set period of time. Passive stretching is frequently utilized in Yoga.
- Dynamic Stretching- Dynamic stretching is achieved on the movements with momentum, preferably than a static stretch. A typical example of dynamic stretching would be moving your arm in a full rotation to stretch your shoulder repeatedly. Each pass is a stretch to activate the muscles or to increase flexibility.
- PNF Stretching- PNF (short for proprioceptive neuromuscular facilitation) stretching is an assisted stretching method, consisting of laying on a table, with the help of a certified specialist. PNF stretches are very focused, and the same as passive stretching, or the physical therapy specialist will hone in specifically on target muscles by holding you in position.
stretching improves – Increase Blood Flow. Stretching may increase your circulation, which can ultimately improve blood flow: Increase Flexibility, Increase Range of Motion, Reduce Injuries, Improve Posture, and Reduce Stress.
Proprioceptive Neuromuscular Facilitation (PNF)
PNF is a highly skilled and specific type and sequence of stretches.PNF is a stretching technique utilized to increase ROM and flexibility.PNF is a progressive stretch involving muscle contraction and relaxation. Your physiotherapist will kindly stretch the muscle and you will resist the stretch by contracting the muscle for about 5 seconds. Your physiotherapist will indicate the force of contraction required and/or this depends on the condition of the muscle. You then relax the muscle and your physiotherapist will kindly stretch the muscle further for about 30 seconds. There are then about 30 seconds of rest and the process is repeated again many times. PNF increases ROM by increasing the length of the muscle and increasing neuromuscular efficiency. PNF stretching has been found to increase ROM in trained, as well as untrained, individuals PNF works with the reflexes between the nerves, muscles, and brain to trigger the desired responses in muscle contraction and relaxation. There are three various types of PNF stretches:
- Contract-Relax Method – Involves contracting, holding, relaxing, and then stretching the targeted muscle group.
- Agonist-Contract Method – Involves static or dynamic contraction of the opposing muscle group prior to the stretching of the targeted muscles, and is followed by a static or dynamic stretch. Static stretch: the holding of a muscle in an extended position for a period of your time. Dynamic stretch: an active movement that brings joints and muscles through their full range of motion.
- Contract Relax and Agonist Contract Method – A combination of Contract Relax and Agonist Contract. (Sometimes called hold relax and agonist contraction.)
The progressive stretching and alteration between contraction and relaxation allow the muscle to adapt to its new position each time it is held in position. This permits it to stretch further the next time. If this is often on a regular basis, gains could be made in flexibility and range of movement. PNF could also be of benefit to individuals recovering from muscle damage as part of treatment. It could also help healthy individuals to increase flexibility and range of movement. This may be beneficial for sporting activities to improve the body’s ability to perform.
Mobilization with Movement
Mobilization with Movement may be called an Active Release, or Mulligan Mobilization. Through careful evaluation and assessment, your therapist may identify areas of tissue tension in your body. Mobilization with movement (MWM) is the concurrent application of sustained accessory mobilization applied by a therapist and an active physiological movement to the end range applied by the patient. At the Passive end range of motion overpressure, or stretching, is then delivered without pain as a barrier. These areas may have scar tissue, adhesions, fibrosis, weakness, tightness, or stiffness. The therapist applies pressure to the area while instructing you in a particular movement that helps the tissue soften and release.
Manual Traction
Traction is a manual technique that is designed to reduce pressure on affected vertebral discs that are causing pain. Traction is a manual ‘stretching’ of the spine that reduces pressure on the discs and therefore reduces the individual’s pain. Traction is the application of a pull and force to body tissues in opposition to an area of compression. Manual Traction is also one type of minimally invasive treatment option for neck and back pain. It has proven to be an effective mechanism for providing patients with pain relief and/or increased mobility. The most important principle behind the lumbar and cervical traction is to decompress the spine. A disc is a circular structure that sits between every vertebra in the spine. It has a tough outer layer around soft inner tissue. When a disc is under pressure or damaged, the tough outer layer is damaged and the soft inside protrudes through the gap. This protrusion compresses nearby nerves causing pain. The Traction pulls the vertebra away from the disc, releasing the pressure on the disc. This helps the soft part of the disc to return within the disc. This decompresses the nerve and reduces pain. This also assists to rehydrate the disc.

For instance, if you have stiffness in your neck, your therapist may choose to apply manual cervical traction as one of the treatments to ease your neck pain and stiffness. Traction is normally applied in conjunction with several other manual techniques, like Myofascial Release and Range of Motion. Manual traction is a physical therapy treatment technique that is used to help separate the discs, joints, and bones in your cervical or lumbar spine. It also assists to improve circulation, relieve muscle spasms, decrease pain, and improve the range of motion of the spine. usually, traction is followed by a series of exercises to strengthen the muscles in the area to support the newly stretched and released tissues. Traction therapy, or spinal decompression therapy, is a non-surgical treatment that uses manual or mechanical means to stretch the spine and relieve pain among affected discs. This treatment repositions herniated or bulging discs, reducing pressure on the back.
Traction could also be beneficial for problems such as:
- Herniated or prolapsed disc
- Sciatica
- Neck pain
- Spondylitis
- Spinal stenosis
- Degenerative disc disease
Trigger Point Therapy
The Trigger points are tender points in the body where a muscle or group of muscles has become hyperactive, or too short and too tight. Trigger points commonly cause “referred pain”, which is when you feel pain in a different spot in the body from where the dysfunction actually is. For example, you may have pain on the outside of your shoulder but the trigger point is actually in a tight muscle between your shoulder blades. Your therapist could also help you to identify your trigger points and pain patterns and show you how to treat them at home with trigger point techniques. They might also show you how to prevent them from returning by helping you correct your posture and learn specific stretches and exercises for muscle imbalances.
Causes –
Generally, TrPs happen due to:
- Ageing,
- Injury carries by a fall, stress, or birth trauma.
- Lack of exercise – commonly in sedentary persons between 27,5 to 55 years, of which 45% are men,
- A Bad posture – upper crossed pattern and lower crossed pattern, swayback posture, telephone posture, cross-legged sitting,
- Muscle overuse and respective micro-trauma – weightlifting,
- Chronic stress conditions – anxiety, psychological stress trauma, depression,
- Vitamin deficiencies – ascorbic acid (vitamin c), vitamin D, vitamin B; folic acid; iron;
- Sleep disturbance,
- Joint problems and hypermobility.
- Another sign to test up to be sure we are at the proper spot is:
- The initial onset of pain and the recurrence of pain is of muscular origin.
- Reproducible spot tenderness occurs within the muscle at the site of the trigger point pain.
- Pain is referred to locally or at a distance on mechanical stimulation of the trigger point. This referred pain or tenderness projects in a pattern characteristic of that muscle and reproduce part of the patient’s complaint.
- There are muscle stiffness and/or palpable hardening of a taut band of the muscle fibers passing through the tender spot in a shortened muscle (like a string of a guitar),
- A local twitch response of the taut muscle and jump sign occurs when the trigger point is stimulated
Physical Therapy Management
- If possible, everyday life factors that arouse the emergence of a TrPs should be eliminated or reduced,
- Posture training and/or education about postures and lifestyle,
- Passive stretching and/or Foam Roller stretching, a few times a day,
- Self-massage, a few times a day, and particularly Deep Stroking Massage done rhythmically and in only one direction,
- Strengthening: primarily only isometric and then isotonic exercises,
- Ischemic Compression Technique – the term has been wont to describe treatment in which ischemia is induced in the TrPt zone by applying sustained pressure. As yet, this principle is questionable since the nucleus of the TrP intrinsically presents important hypoxia. Simons described an identical treatment modality, though without the necessity to induce additional ischemia in the TrP zone (TrP Pressure Release). The goal of this system is to free the contracted sarcomeres within the TrP. The number of pressure applied should suffice to produce gradual relaxation of the tension within the TrP zone, without causing pain. even both the techniques show imitate significant improvement of the ROM after treatment.
- Taping Technique,
- Spray and/or Stretch Technique by using ethyl chloride spray,
- Manual Lymphatic Drainage (MLD), therefore the presence of TrPs obstacle lymphatic flow,
- Another proprioceptive neuromuscular techniques: Reciprocal Inhibition (RI), Post-Isometric Relaxation (PIR), Contract Relax and Hold Relax (CRHR), Contract Relax and Antagonist Contract (CRAC),
- Some specific techniques like Neuromuscular Technique (NMT), Muscle Energy Technique (MET), and Myotherapy (MT).
Instrument Assisted Soft Tissue Massage (IASTM)
Instrument Assisted soft tissue mobilization (IASTM) may be a skilled myofascial intervention used for soft-tissue treatment. It is established on the principles of James Cyriax cross-friction massage. A proposed description for IASTM is “a skilled intervention that consists of the use of specialized tools to manipulate the skin, myofascial, muscles, and tendons by various direct compressive stroke techniques”.
To perform Instrument assisted soft tissue mobilization, your therapist will use a tool made up of surgical-grade stainless steel to treat muscles, tendons, ligaments, fascia, and skin. The tools have different shapes and beveled edges that conform to your body’s contours, allowing your therapist to supply more specific pressure and treatment. IASTM evolved from the normal Chinese Medicine practice of Gua sha. Research into Instrument assisted soft tissue mobilization has shown that when applied by a talented practitioner it stimulates mechanoreceptors in the cells to increase fibroblastic activity, and creates vascular and neurophysiological effects. That is, it activates your body’s ability to heal on its own. you would possibly be familiar with some brand names of the tools, such as HawkGrips®, Graston, and RockTape.

There are a number of different speeds and pressures that an Instrument Assisted Soft Tissue Massage trained physical therapist might use while conducting this specific technique, and it will be based on the nature of your condition and your specific needs. These different speeds and pressures work to facilitate a contraction (also known as turning a muscle on) and/or inhibit a muscle (also known as turning a muscle off). When using certain levels of pressure through Instrument Assisted Soft Tissue Massage on the affected muscles, tendons, or ligaments, a mild inflammatory response is initiated. While this can seem counterintuitive, inflammation helps promote the body’s natural healing process, so you can recover and get back to your life faster.
Conditions For Which Instrument assisted soft tissue mobilization is Usually Used – Medial Epicondylitis, Lateral Epicondylitis, Carpal Tunnel Syndrome, Neck Pain, Plantar Fascitis, Rotator Cuff Tendinitis, Patellar Tendinitis, Tibialis Posterior Tendinitis, Heel Pain or Achilles Tendinitis, DeQuervain’s Syndrome, Post-Surgical and Traumatic Scars, Myofascial Pain and Restrictions, Musculoskeletal Imbalances, Chronic Joint Swelling Associated with Sprains or Strains, Ligament Sprains, Muscle Strains, Non-Acute Bursitis, RSD (Reflex Sympathetic Dystrophy), Back Pain, Trigger Finger, Hip Pain (Replacements), Iliotibial Band Syndrome, Shin Splints, Chronic Ankle Sprains, Acute Ankle Sprains (Advanced Technique), Scars (Surgical, Traumatic).
Contraindications – Open wound (unhealed suture site), Unhealed fracture, Thrombophlebitis, Uncontrolled hypertension, Patient intolerance or hypersensitivity, Hematoma, Osteomyelitis, Myositis ossificans, Hemophilia.
Types of tools –
There are many companies for Instrument assisted soft tissue mobilization such as RockTape®, HawkGrips®, Graston®, Técnica Gavilán®, Functional and Kinetic Treatment with Rehab (FAKTR)®, Adhesion Breakers®, augmented soft tissue mobilization or ASTYM®, and/or Fascial Abrasion Technique™. All company has their own treatment approach with different instrument designs. Instrument-assisted soft tissue mobilization can be made from varying materials including stainless steel, titanium, plastic, buffalo horn, stone, quartz, and jade. The most often IASTM instruments used are stainless steel.
When Instrument assisted soft tissue mobilization is applied it goes through 6 steps
- Examination
- Warm-up, warm-up is done for 10 to 15 mins by light jogging, elliptical machine, stationary bike, or an upper body ergometer
- IASTM, done at a 30 to 60 degrees angle for 40 to 120 seconds
- Stretching, 3 reps for 30 seconds
- Strengthening, high repetitions with low load exercise
- Cryotherapy, 10 to 20 min
Benefits to the Therapist –
IASTM provides clinicians with a mechanical advantage, thus preventing over-use to the hands, it provides deeper tissue penetration with less compressive forces to the interphalangeal joints of the clinician’s hand. Snodgrass SJ surveyed physical therapists and found that after spinal pain, the second most often cause for absenteeism from work was the overuse of the thumb. Ninety-one percent of physiotherapists which utilize some sort of massage had to modify their treatment techniques because of thumb pain. Also, it increases the vibratory perception of the physical therapist’s hand holding the instrument to alter soft tissue properties such as tissue restrictions or adhesions. So the therapist is able to detect soft tissue abnormalities easier.
Cupping Therapy
Cupping Therapy is one of the oldest known forms of treatment, found in the people ancient cultures. New research has shown that Cupping Therapy helps in the treatment of many conditions, by reducing pain and inflammation, improving blood and lymph flow, stimulating nerves and the body’s systems, and facilitating the healing process. Cupping Therapy is meant to assist the body’s innate ability to heal itself. Vacuum or suction cups are applied to the body to draw toxins or waste products out of the surrounding tissues and increase blood flow to the area. Cups could also be applied in one spot and left in place, they can be applied and slid across a larger area as a massage technique, and they can be applied with or without heat. Some people experience local redness and/or swelling after the application of Cupping Therapy. There are various methods of cupping, including Dry and Wet.

During both types of cupping, your therapist would put a flammable substance such as alcohol, herbs, or paper in a cup and/or set it on fire. As the fire goes away, they put the cup upside down on your skin. As the air inside the cup becomes cooler, it creates a vacuum. This causes your skin to rise and/or redden as your blood vessels expand. The cup is normally left in place for up to 3 minutes. A more modern version of cupping utilizes a rubber pump instead of fire to create a vacuum inside the cup. a few times therapists use silicone cups, which they could move from place to place on your skin for a massage effect.
Dry Needling
Dry needling may be a treatment performed by skilled, trained physical therapists, certified in the procedure. Trigger point dry needling is an invasive procedure where a fine needle or acupuncture needle is inserted into a specific muscle and skin. It is aimed at myofascial trigger points (MTrP) which are hyperirritable spots within the skeletal muscle that are associated with a hypersensitive palpable nodule in a taut band. Trigger point dry needling could also be carried out at the superficial or deep tissue level. A skinny monofilament needle that penetrates the skin and treats underlying muscular trigger points for the management of neuromusculoskeletal pain and movement impairments. Dry needling could also be performed by physical therapists certified in Clean Needle Technique. Where there are trigger points, tender points, or areas of fascia and muscle that are hypersensitive or irritated, needles may be inserted in particular spots to treat those areas. The needle might create a fasciculation, or small movement, in the muscle that then releases the tension from that area. Needling may also stimulate blood flow to the area, increase oxygenation to the tissues, and reduce central sensitization (overactivity in the surrounding nerves).

Dry needling has been shown to immediately increase pressure pain threshold and range of motion, reduce muscle tone and decrease pain in patients with musculoskeletal conditions. Its suggested mechanisms of action include:
- Local Twitch Response: Dry needling can elicit a ‘local twitch response’ which is an involuntary spinal reflex resulting in a localized contraction of the affected muscles that are being dry-needled. Local twitch response can lead to alteration in the length and tension of muscle fibers and stimulate mechanoreceptors like A Beta fibers.
- Effects on Blood Flow: Sustained contraction of taut muscle bands within trigger points might cause local ischemia and hypoxia. Dry needling causes vasodilation within the small blood vessels leading to increased muscle blood flow and oxygenation.
- Neurophysiological effects: Dry needling may produce local and central nervous responses to restore hemostasis at the site of the trigger point which results in a reduction in both central and peripheral sensitization to pain.
- Remote Effects: Dry needling of distal MTrP has been found to possess an analgesic effect on proximal MTrP. The literature has conflicting evidence regard to the contralateral effect.
- Placebo Effect
Indication
- Dry needling can be indicated for myofascial pain with the presence of trigger points. Dry needling has also been shown to be beneficial for the treatment of strains, osteoarthritis, and tendinopathies.
- Contraindications
- Patient unwilling – fear, patient belief,
- Not able to give consent – communication, cognitive, age-related factors,
- Medical emergency or acute medical condition,
- Over an area or limb with lymphedema as this can increase the risk of infection or cellulitis and the difficulty of fighting the infection if one should occur,
- Abnormal bleeding tendency, Compromised immune system, Pregnancy, Children, Vascular disease, Diabetes.
Chiropractic Therapy
Chiropractic therapy marks pain and movement issues in the musculoskeletal system, specifically for pain in the back, neck, arm, or leg joints, and headaches, according to the American Chiropractic Association. One of the most often chiropractic therapies is spinal manipulation, sometimes called a chiropractic adjustment, where the practitioner applies controlled force to the spine at certain joints to restore mobility and reduce pain. chiropractic is a form of alternative medicine which is concerned with the diagnosis, treatment, and prevention of mechanical disorders of the musculoskeletal system, especially of the spine. It has esoteric origins and is based on many pseudoscientific ideas.
Many chiropractors, especially those within the field’s early history, have proposed that mechanical disorders of the joints, especially of the spine, affect general health, and that regular manipulation of the spine (spinal adjustment) improves general health. The important chiropractic treatment technique involves manual therapy, especially manipulation of the spine, other joints, and soft tissues, but could also include exercises and health and lifestyle counseling. Spinal manipulation, which chiropractors call “spinal adjustment” or “chiropractic adjustment”, is that the most common treatment used in chiropractic care. Spinal manipulation may be a passive manual maneuver during which a three-joint complex is taken past the normal range of movement, but not thus far as to dislocate or damage the joint. Its defining factor may be a dynamic thrust, which is a sudden force that causes an audible release and attempts to increase a joint’s range of motion.
High velocity, low amplitude spinal manipulation (HVLA-SM) thrusts have physiological effects that signal neural discharge from paraspinal muscle tissues, based on the duration and amplitude of the thrust are factors of the degree of paraspinal muscle spindle activation. Clinical skill in employing HVLA-SM thrusts that are based on the ability of the practitioner to handle the duration and magnitude of the load. More generally, spinal manipulative therapy (SMT) describes techniques where the hands are wont to manipulate, massage, mobilize, adjust, stimulate, apply traction to, or otherwise influence the spine and/or related tissues.
Massage
Massage might be similar to chiropractic therapy because it involves controlled pressure applied by the practitioner’s hands to the patient’s body. Although, the parts of the body targeted by each method differ and so do the actual techniques themselves. Some of the massage therapy techniques include:
- Stroking: Soft tissue massage – Stroking or gliding motions can be performed over a muscular and/or connective tissue area that assists to improve tissue relaxation, mobility, or pain in the region.
- kneading or Petrissage – lifting or picking up muscles and rolling the folds of skin.
- Percussion or Tapotement – Includes hacking, clapping, beating, pounding, or vibrations. rapid or repeated striking with the side of the hand, generally with partly flexed fingers. In Vibration, Oscillatory movements shake or vibrate the body. Tapotement is one of the main stimulating massage techniques that can wake the body up.
- Friction massage: A more irritating form of massage that is meant to temporarily increase inflammation and break up scar tissue in an effort to promote healing and decrease pain. Frictions involve applying pressure to little problematic areas. Massage therapists will kindly use their thumbs and fingers to apply deep pressure in a back and forth and/or in a circular motion to underlying muscles. Massage clients might also feel some discomfort when friction is applied, but it should not be painful. The friction massage technique is generally utilized after the body has been warmed up from other massage techniques. Friction helps to break scar tissue and adhesions, and realign tissue fibers. It might also be helpful in rehabilitating an injury.
- Effleurage – Effleurage involves applying a little amount of pressure with hands laid flat, side by side, gliding over the body. Knuckles and/or forearms could also be used when applying this massage technique. The effleurage technique is used to ease muscles and/or help relax clients. It could also help to encourage blood circulation and ready the client for more intense massage strokes.
- Compression Massage – Rhythmic compression into muscles is used to create deep hyperemia and softening effects in the tissues. Normally used for sports massage as a warm-up for deeper, more specific massage work. Compression may relieve tightness in muscles, aid in injury recovery, and assist with relaxation. Since compressions would initially restrict blood flow, it will encourage a larger amount of blood to gather in that area until it’s released. This process can also help to improve blood circulation.
Massage could target soft tissue, such as muscles, nerves, and blood vessels, or connective tissue, such as tendons, ligaments, skin, and fat. Several physical and neurological pain conditions can improve from the implementation of regular, targeted massage therapies.
Joint manipulation and mobilization
Joint manipulation:
- A quick, thrust-style technique that takes a joint beyond its normal range of motion in order to improve mobility and (in some cases) help with the pain. Joint manipulation is characteristically associated with the production of the audible ‘clicking’ or ‘popping’ sound. This sound is believed to be the result of a phenomenon known as cavitation occurring with the synovial fluid of the joint. When a manipulation is performed, the applied force divides the articular surfaces of a fully encapsulated synovial joint. This deforms the joint capsule and intra-articular tissues, which successively creates a reduction in pressure within the joint cavity. In this lower-pressure environment, a few of the gases that are dissolved in the synovial fluid (which are naturally found in all bodily fluids) leave the solution creating a bubble or cavity, which rapidly collapses upon itself, leading to a ‘clicking’ sound. The contents of the gas bubble are thought to be mostly carbon dioxide. The consequences of this process would remain for a period of time termed the ‘refractory period’, which could also range from a few minutes to more than an hour, while it is steadily reabsorbed back into the synovial fluid. There is little evidence that ligament laxity surrounding the target joint is associated with an increased probability of cavitation
- Kinetics – Until recently, force-time histories measured during spinal manipulation were described as consisting of three distinct phases: the preload (or thrust) phase, the thrust phase, and therefore the resolution phase. Evans and Breen added a fourth ‘orientation’ phase to describe the period in which the patient is oriented into the appropriate position in preparation for the thrust phase.
- When individual peripheral synovial joints are manipulated, the distinct force-time phases that occur in spinal manipulation are not as evident. In particular, the rapid rate of change of force that happens during the thrust phase when spinal joints are manipulated is not always necessary. Most studies to possess measured forces which are utilized to manipulate peripheral joints, such as the metacarpophalangeal (MCP) joints, show no more than a gradually increasing weight. This is commonly probably because there are many more tissues restraining a spinal motion segment than an independent metacarpophalangeal joint.
Kinematics- The kinematics of a complete spinal motion segment when one of its constituent spinal joints is manipulated is much more complex than the kinematics that occurs during the manipulation of an independent peripheral synovial joint. Even so, the motion that happens between the articular surfaces of any people’s synovial joint during manipulation must be very similar and is described below.
- Early models describing the kinematics of a private target joint during the different phases of the manipulation (notably Sandoz 1976) were based on studies that investigated joint cracking in MCP joints. The cracking was elicited by pulling the proximal phalanx far away from the metacarpal bone (to separate, or ‘gap’ the articular surfaces of the Metacarpophalangeal joint) with steadily increasing force till a pointly resistance, caused by the cohesive properties of synovial fluid, was met and then broken. These studies were therefore never designed to make models of therapeutic manipulation, and therefore the models formed were erroneous in that they described the target joint as being composed at the end range of a rotation movement, in the orientation phase. The model then predicted that this end range position was maintained during the thrust phase until the thrust phase where it had been moved beyond the ‘physiologic barrier’ created by synovial fluid resistance; conveniently with the limits of anatomical integrity provided by restraining tissues such as the joint capsule or ligaments. This model still dominates the literature. Although, after re-examining the original studies on which the kinematic models of joint manipulation were based, Evans and Breen argued that the optimal thrust position is the equivalent of the neutral zone of each joint, which is the motion region of the joint where the passive osteoligamentous stability mechanisms exert tiny or no influence. This new model predicted that the physiologic barrier is only confronted when the articular surfaces of the joint are divided (gapped, rather than the rolling or sliding that generally happen during the physiological motion), and that it is more mechanically efficient to do this when the joint is near to its neutral configuration.
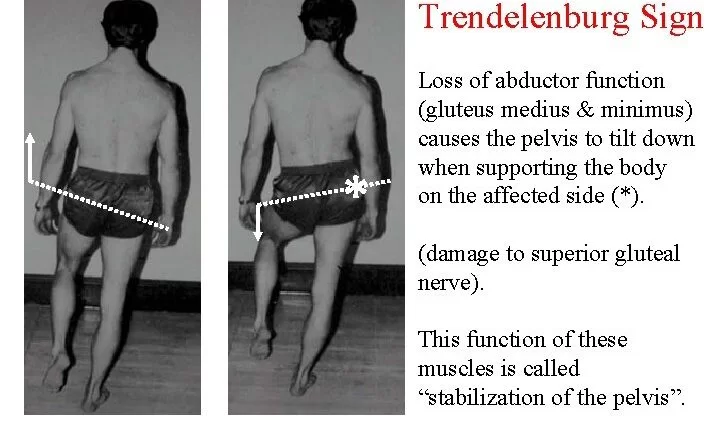
Joint mobilization:
Slower, repetitive oscillations within a joint’s range of motion limit that promote mobility and increase the range of movement in a joint. To mobilize a joint, your therapist may apply passive movements to the joint during a varying range of pressure, speed, and amplitude. That means they might also move your joint a little bit, gently, in a short distance back and forth, or they could make a bigger movement with more pressure. The goal of joint mobilization is to decrease pain and restore optimal biomechanics, movement, and function to the joint. Visceral Mobilization – Visceral mobilization or manipulation is a particular manual therapy technique to relieve fascial adhesions in the deep tissues surrounding your organs and your abdominal wall. Whether from surgery, pregnancy, car accident, trauma, poor posture, muscle imbalance, illness, or other injury, strains in the connective tissue in your abdomen can cause back pain, hip pain, groin pain, shallow breathing, and other dysfunctions. Your therapist may assess these deep tissues, to see if they are contributing to your symptoms, and release them as a part of your physical therapy program.
Guide to Grading of Mobilisations and Manipulations
Maitland Joint Mobilization Grading Scale:
- Grade I – A Smaller amplitude with rhythmic oscillating mobilization in the early range of movement.
- Grade II – Larger amplitude with rhythmic oscillating mobilization in the midrange of movement
- Grade III – Larger amplitude with rhythmic oscillating mobilization to point of limitation in range of movement
- Grade IV – Smaller amplitude rhythmic oscillating mobilization at end of the available range of movement
- Grade V (Thrust Manipulation) – Smaller amplitude, quick thrust at end of the available range of movement
Kaltenborn Traction Grading Scale:
- Grade I – Neutralises joint pressure without separation of the joint surfaces
- Grade II – Separates articulating surfaces, taking up the slack or eliminating play with the joint capsule
- Grade III – Stretching of the soft tissue surrounding joint
Cyriax:
- Grade A – mobilization within a pain-free range of motion
- Grade B – sustained stretch at EOR
- Grade C – high velocity or low amplitude manipulation at EO
Taping
Taping is commonly used as an adjunct or transient technique. Athletes typically make use of taping as a protective mechanism in the presence of an existing injury. Some of the purposes of taping are to restrict the movement of injured joints, and soft tissue and compression to decrease swelling. support anatomical structures, and/or as protection from re-injury.

Taping is used as one of the means of rehabilitation or prophylaxis in instances where support and stability are required, as a first-aid tool, for the precluding of injury and preservation of an injured anatomical structure while healing is taking place. Manual therapy practitioners commonly use therapeutic taping to relieve pressure on injured soft tissue, alter muscle firing patterns or prevent re-injury. A few techniques are designed to enhance lymphatic fluid exchange. Behind a soft tissue injury to muscles or tendons from sports activities, over-exertion, or repetitive strain injury swelling might also restrict blood flow to the area and slow healing. Elastic taping methods could also relieve pressure from swollen tissue and enhance circulation to the injured area.
Acupressure
It is an alternate medicine technique often used in conjunction with acupuncture or reflexology. It is dependent on the concept of life energy which flows through “meridians” in the body. In the treatment, physical pressure is applied to acupuncture points and/or ashi trigger points with the aim of clearing blockages in these meridians. Pressure might also be applied by hand, by the elbow, or with various devices.
Although some medical studies have suggested that acupressure could also be effective at helping manage nausea and vomiting, insomnia, low back pain, migraines, and constipation, among other things, such studies have been established to have a high likelihood of bias. There is no well-founded evidence for the effectiveness of acupressure. Acupressure therapy was prevalent in India.
Acupuncture
Acupuncture is a component of traditional Chinese medicine (TCM) in which thin needles are inserted into the body. It is used most frequently for pain relief, though it is also used to treat a wide range of conditions. Acupuncture is usually, only utilized in combination with other forms of treatment.
Needling technique
- needles – The most frequent mechanism of stimulation of acupuncture points employs penetration of the skin by thin metal needles, which are manipulated manually or the needle might be further stimulated by electrical stimulation (electroacupuncture). Acupuncture needles are generally made of stainless steel, making them flexible and preventing them from rusting or breaking. Needles are usually disposed of after each use to stop contamination. Reusable needles when used must be sterilized between applications. In all areas, only sterile, single-use acupuncture needles are allowed, including in the State of California, USA. Needles may vary in length between 13 to 130 millimeters (0.51 to 5.12 in), with shorter needles used near the face and eyes, and longer needles in areas with thicker tissues; needle diameters vary from 0.16 mm (0.006 in) to 0.46 mm (0.018 in), with thicker needles, utilize on more robust patients. Thinner needles can be flexible and require tubes for insertion. The tip of the needle should not be made too sharp to prevent breakage, yet, blunt needles cause more pain.
- Apart from the usual filiform needle, other types of needles include three-edged needles and therefore the Nine Ancient Needles. Japanese acupuncturists utilize extremely thin needles that are used superficially, sometimes without penetrating the skin, and surrounded by a guide tube (a 17th-century invention adopted in China and thus the West). Korean acupuncture uses copper needles and includes a greater focus on the hand
Insertion
The skin is sterilized then needles are inserted, frequently with a plastic guide tube. Needles can also be manipulated in various ways, including spinning, flicking, or moving up and down relative to the skin. Since most pain is felt within the superficial layers of the skin, a quick insertion of the needle is recommended. Generally, the needles are stimulated by the hand in order which leads to a dull, localized, aching sensation that is called de qi, as well as “needle grasp,” a tugging feeling felt by the acupuncturist and/or generated by a mechanical interaction between the needle and skin. Acupuncture may be painful. The skill level of the acupuncturist might influence how painful the needle insertion is, and a sufficiently skilled practitioner can be able to insert the needles without causing any pain.
Bobath concept
- A Bobath concept is an approach to neurological rehabilitation that is applied in patient assessment or treatment (such as with adults after stroke or children with cerebral palsy). The aim of applying the Bobath concept is to promote motor learning for efficient motor control in different environments, thereby improving participation and function. This is done through specific patient handling skills to teach patients through the initiation and completion of intended tasks. This approach to neurological rehabilitation is multidisciplinary, primarily consisting of physiotherapists, occupational therapists, and speech and language therapists. In the United States, the Bobath concept is also called ‘neuro-developmental treatment (NDT).
- Stroke rehabilitation – The concept and its international tutors or instructors have embraced neuroscience and the developments in understanding motor control, motor learning, neuroplasticity, and human movement science. They believe that this approach should continue to develop.
- In the Bobath Concept, postural control is the inspiration on which patients begin to develop their skills. Patients undergoing this treatment generally find out how to control postures and movements and then progress to more difficult ones. Therapists analyze postures or movements and look for any abnormalities that can be present when asked to perform them. Examples of frequent abnormal movement patterns that comprise obligatory synergy patterns. These patterns could also be described as the process of trying to perform isolated movement of a particular limb but triggering the use of other typically uninvolved muscles (when compared to normal motion) in order to achieve movement. Obligatory synergy patterns might be further subdivided into flexion and extension synergy components for both the upper and lower extremities. This approach requires active participation from both the patient and also the therapist. Based on the patient, rehabilitation goals might work to improve any or all of the following: postural control, coordination of movement sequences, movement initiation, optimal body alignment, abnormal tone, or muscle weakness. Treatment will therefore address both negative signs such as impaired postural control, and/or positive signs such as spasticity.
- Intervention strategies and techniques for Bobath consist of therapeutic handling, facilitation, and/or activation of the key points of control. Therapeutic handling is used in order to influence the quality of the patient’s movements and incorporates both facilitation and inhibition. Facilitation may be a key technique used by Bobath practitioners to promote motor learning. It is the use of sensory information (tactile cues through manual contacts, verbal directions) to strengthen weak movement patterns and to discourage overactive ones. The suitable provision of facilitation during the motor task is regulated in time, modality, intensity, and withdrawal, all of which affect the outcome of motor learning. Inhibition could also be described as reducing parts of movement or posture that are abnormal and interfere with normal performance. The Key points of control generally refer to parts of the body that are advantageous when facilitating or inhibiting movement or posture.
- Activities assigned by a Physical Therapist or Occupational Therapist to an individual person who has suffered from a stroke are selected based on functional relevance and are varied in terms of difficulty and the environment in which they are performed. Making use of the individual’s less involved segments, also known as compensatory training strategies, is avoided. Carryover of the functional activities in the home and community setting is largely attributed to patient, family, and caregiver education.
Osteopathy
Osteopathic manipulation is the core set of techniques in osteopathy. Parts of osteopathy, such as craniosacral therapy, have no therapeutic value or have been labeled as pseudoscience and quackery. The techniques depend on an ideology created by Andrew Taylor Still (1828 – 1917) which posits the existence of a “myofascial continuity” a tissue layer that “links every part of the body with every other part”. Osteopaths try and diagnose and treat what was originally called “the osteopathic lesion”, but which is now named “somatic dysfunction”, by manipulating an individual’s bones and muscles. Osteopathic Manipulative Treatment (OMT) techniques are most often used to treat back pain and other musculoskeletal issues. Osteopathic manipulation is still included in the curricula of osteopathic physicians, to not be confused with non-physician osteopaths, and is taken into account as a unique aspect of Doctor of Osteopathic Medicine (DO) training.
Counterstrain may be a system of diagnosis and treatment that considers the physical dysfunction to be a continuing, inappropriate strain reflex, which is inhibited during treatment by applying an edge of a mild strain in the direction exactly opposite to that of the reflex. After a counter strain point tender to palpation has been diagnosed, the identified tender point is treated by the osteopathic physician who, while monitoring the tender point, positions the patient such that the point is not elongated tender to palpation. This position is held for ninety seconds and therefore the patient is subsequently returned to her normal posture. Most frequently this position of ease is usually achieved by shortening the muscle of interest. Improvement or resolution in the tenderness at the identified.
counter strain point is the desired outcome. The utilization of the counter-strain technique is contraindicated in patients with severe osteoporosis, pathology of the vertebral arteries, and in patients who are very ill or cannot voluntarily relax during the procedure.
Lymphatic pump treatment (LPT)
It is a manual technique intended to encourage lymphatic flow in a person’s lymphatic system. The first modern lymphatic pump technique was developed in 1920, However, an osteopathic physician used various forms of lymphatic techniques as early as the late 19th century.
Relative contraindications for the use of lymphatic pump treatments include fractures, abscesses or localized infections, and severe bacterial infections with body temperature elevated higher than 102 °F.
High velocity, low amplitude (HVLA)
It is a technique that employs a rapid, targeted, therapeutic force of brief duration that travels a short distance within the anatomic range of motion of a joint and engages the restrictive barrier in one or more places of motion to evoke the release of restriction. The use of High velocity and low amplitude is contraindicated in patients with Down syndrome due to instability of the atlantoaxial joint which may stem from ligamentous laxity and in pathologic bone conditions such as fracture, a chronology of a pathologic fracture, osteomyelitis, osteoporosis, and extreme cases of rheumatoid arthritis. The High velocity and the low amplitude are also contraindicated in patients with vascular diseases such as aneurysms, or disease of the carotid arteries or vertebral arteries. Individuals taking ciprofloxacin or anticoagulants, or who have local metastases should not receive HVLA.
McKenzie method
- There is only weak evidence for the effectiveness of the method, used for treating lower back pain, and research into the effectiveness of the McKenzie method has been of poor quality.
- As Compared to other treatments, the McKenzie method is not better at treating acute pain and disability for people with lower back pain. It might also be better than some other approaches for chronic lower back pain, but the evidence for this is insufficient to recommend the method.
- Exercises targeting midline strengthening, as used in the McKenzie method, are no more helpful to lower back pain than conventional flexion and extension exercises.
- Centralization occurs when pain symptoms off-centered from the mid-line of the spine migrate towards the center of the mid-line of the spine. This migration of pain symptoms to the core of the lower back is a sign of progress in the McKenzie method. The Extension exercises are a few times referred to as McKenzie exercises for this reason. According to the McKenzie method, movements and exercises that produce centralization are beneficial whereas movements that move pain away from the spinal mid-line are detrimental.
- Each of the techniques listed above may be beneficial when used in the correct circumstances. Individuals are often employed in tandem with one another. After a thorough evaluation, your physical therapist could also provide you with more information about which hands-on techniques may be useful to you.
- Physical therapists and doctors alike are seeing the potential manual therapy techniques have for many people suffering from painful conditions. Because of physical therapy, healthcare professionals may prescribe fewer medications and other more invasive, costly treatment methods. If you or your family member suffers from a pain-inducing condition, talk to your doctor about whether physical therapy could be an option. Your physical therapist would carefully evaluate and assess you and will work with you to select the types of manual therapy that best complement a complete physical therapy program customized for you.
The Benefits of Hands-On Physical Therapy
Manual physical therapy (PT) refers to a cluster of hands-on therapeutic techniques which is utilized by a therapist to treat a wide variety of symptoms and conditions. This style of treatment, which is frequently performed same side as other rehab techniques such as exercise or pain relieving modalities, could also be helpful in addressing numerous different concerns, including pain, stiffness, or range of motion limitations. Physical therapists or hand therapists incorporate manual therapy to assist a patient, restoring mobility, improving motor control, reducing pain, and enhancing the efficiency of movement.
What Makes Manual Therapy “Hands On”?
- Whether it is passively moving your joints, massaging a body region, or stretching a muscle, this type of therapy permits your physical therapist to harness their knowledge of anatomy and pathology while utilizing their own hands to treat your precise condition.
Manual therapy can also be utilized for various purposes, including increasing the flexibility of a muscle, relaxing a muscle group, improving the range of motion at a joint, or reducing your pain. - Oftentimes, this treatment category is particularly valuable during the more acute stages of rehab, when your movement may be more limited in a region and pain levels are traditionally higher.
As symptoms begin to subside and movement enhances, manual therapy may still be utilized later on in combination with more active therapy techniques, like strengthening balance training, or plyometric exercise.
Yet, passive hands-on treatments are a beneficial part of your care, whereas they are seldom performed in isolation without a complementary active component.
When to Try Hands-On Physical Therapy
- Manual therapy can be a valuable addition to physical therapy for a variety of concerns. For instance, following a surgery or procedure, joint mobilizations and passive stretching usually play an important role in recovering your range of motion in the affected area.
Certain types of manipulations and mobilizations might also be used following a more acute injury, like a back or neck strain. In addition, soft tissue massage might also be beneficial for managing chronic pain complaints and improving participation in the more active components of therapy.
Considerable different specific diagnoses have been found to benefit from manual physical therapy. For instance, several kinds of research have shown improved pain and function in patients with knee osteoarthritis after being treated with soft tissue massage.
Manual therapy contains several hands-on treatment techniques used by a physical therapist to treat different conditions. These techniques may be used together or separately, particularly in the acute phase of rehabilitation. Thereafter, they might also be used in addition to exercises. While all physical therapists are trained in manual therapy, particulars specialize in it. - People with shoulder pain also responded approvingly to joint mobilizations and manipulations to their middle back. The identical is true for an individual with neck pain whose therapy treatment comprised mobilizations and manipulations to their upper (cervical) spine.
Eventually, passive stretching, massage, and mobilizations can assist to manage the symptoms associated with plantar fasciitis.
Because of the wide range of conditions that may also benefit from hands-on physical therapy, it is important to speak to your physical therapist about your individual symptoms.
Manual Physical Therapy could Offer Pain Relief for Acute and Chronic Back Pain?
Manual therapy might also be helpful for the treatment of joints that lack adequate mobility and range of motion in particular musculoskeletal conditions. This regulation can also cause discomfort, pain, and an alteration in function, posture, and movement. Manual physical therapy concerns fixing mobility to stiff joints and decreasing muscle tension in order to return the patient to more natural movement without pain. Accordingly, manual physical therapy could provide back pain relief both for patients with chronic back pain concerning joint problems, such as sacroiliac joint dysfunction, and acute back pain from soft tissue injuries such as a back muscle strain and a stretched back ligament. Although extensive clinical analyses have yet to be performed on all areas of manual therapy, limited clinical data and patient reports reinforce the assertion that manual physical therapy may be effective in reducing back pain for certain patients. As a group, manual physical therapy techniques are aimed at relaxing tense back muscles and restricted joints in demand to decrease back pain and increase flexibility
At Home Alternatives
- There are no direct substitutes for the skilled manual therapy you obtain from a physical therapist. Although, in some cases, the cost of physical therapy makes receiving care unattainable, and at home, alternatives must be considered.
- Considerable additional devices are available for purchase that attempt to replicate some of the hands-on techniques performed by a therapist. For example, foam rollers can be used to enhance flexibility and range of motion in a muscle when combined with stretching exercises.
- Further pieces of equipment, such as massage guns or massage balls, are also widely available, though their uses are still being studied. Be sure to speak to your physician before starting to use any at-home device to ensure it is appropriate for your distinct situation.
- In expansion, you might want to speak to your physical therapist about any financial difficulties you are having. Multiple clinics have self-pay discounts or sliding scales established on your income, which can make receiving physical therapy better affordable.
What are the contraindications for manual therapy?
Articulatory techniques are contraindicated for the following:
- Patients with vertebral malignancy, Infection or inflammation, Myelopathy, Multiple adjacent radiculopathies, Cauda equina syndrome, Vertebral bone disease, Bony joint instability, and/or Cervical rheumatoid disease.
- Direct manipulation (eg, high velocity/low amplitude) is contraindicated in those patients and in the presence of the following:
- Spinal deformity, Systemic anticoagulation treatment, Severe diabetes or atherosclerotic disease, Degenerative joint disease, Vertebral basilar disease or insufficiency, Spondyloarthropathies, Ligamentous joint instability or congenital joint laxity, Aseptic necrosis, Local aneurysm, Osteoporosis, Acute disk herniation, Osteomalacia
Absolute contraindications to massage include the following:
- Deep venous thrombosis, has the potential of propagating emboli from increased blood flow in a limb causing thrombus detachment from the vessel wall, Acute infection, Bleeding, and A new open wound
Relative contraindications to massage include the following:
- Incompletely healed scar tissue, Fragile skin, Calcified soft tissue, Skin grafts, Atrophic skin, Inflamed tissue, Malignancy, Inflammatory muscle disease, Pregnancy
Summary
Manual therapy includes several hands-on treatment techniques utilized by a physical therapist to treat various conditions. These techniques may be used concurrently or separately, mainly in the acute phase of rehabilitation. Subsequently, they might be used in addition to exercises. While all physiotherapists are trained in manual therapy, some specialize in it.
FAQ
Which type of pain is relieved by manual therapy?
Manual therapy is a safe, highly effective treatment that may successfully treat a variety of painful conditions, including Chronic back pain and spasms. Muscle tension in the neck and shoulders. Problems with joint mobility and stiffness. Headaches and migraines.
What is orthopedic manual physical therapy?
Orthopaedic Manual Physical Therapy is a specialized area of physiotherapy or physical therapy for the management of neuro-musculoskeletal conditions, based on clinical reasoning, using highly specific treatment approaches including manual techniques and therapeutic exercises.
How does manual therapy differ from physical therapy?
Manual therapy refers to a group of hands-on treatments that may be included in a physical therapy session. Depending on your unique condition, passive manual therapy interventions are generally utilized alongside other more active treatments (like exercise) while you are in rehab.
What are the benefits of manual physical therapy?
Manual physical therapy can provide you with several advantages, including pain relief, increased joint mobility, a more adequate range of motion, and improved muscular flexibility.
Is manual therapy the same as massage?
Soft tissue massage is one of several “hands-on” techniques comprised in the cluster of manual therapy interventions. Unlike at-home massagers, the manual techniques delivered by a physical therapist operate their specific training in anatomy and pathology to care for your body’s unique needs.
Is a manual therapist a doctor?
So, since 2015, physical therapists are doctors, but they are not physicians. They experience additional schooling as required for their distinct professional practice just like any dentist, nurse, doctor, surgeon, optometrist, orthodontist, or therapist.
How many years accomplish it takes to be a physical therapist?
Bachelor of Science in Physical Therapy is a four and half year program that delivers professionals who promote optimal health and function by providing services that create, maintain, and restore maximum movement and functional ability, for a person at any stage of life, when their movement and function are intimidated by aging.
Can physical therapists do manual adjustments?
Physical therapists treat disease, injury, or deformity via exercise, massage, and heat. They are trained to treat the whole body exceeding the spine and skeletal body. A physical therapist would not perform manipulations or pop backs, but do manual therapy and work supportive muscles around the problem area.



2 Comments