Muscle Cramps
What is Muscle Cramps?
Muscle cramps are a common occurrence that most people experience at some point in their lives. They are characterized by an involuntary and forceful contraction of a muscle that remains contracted and does not relax. The cramp causes intense pain and a temporary inability to use the affected muscle.
Cramps typically only last a few seconds to several minutes, though they can sometimes persist longer. While sometimes just a nuisance, severe and frequent muscle cramps can negatively impact quality of life.
While cramps can occur seemingly at random in otherwise healthy individuals, they tend to be more prevalent under certain situations and conditions that predispose people to cramping. By understanding the various causes and risk factors for muscle cramps, individuals can take preventative steps to minimize cramp occurrences.
Causes of Muscle Cramps
Dehydration and Electrolyte Imbalances
One of the most common underlying causes of muscle cramps is inadequate hydration leading to a sodium and/or potassium electrolyte imbalance. Electrolytes like sodium and potassium facilitate electrical signals in the nervous system and muscles that enable muscle contraction and relaxation.
When these electrolytes are low, muscles are prone to abnormal activation and involuntary contraction. Athletes who sweat profusely and do not replenish their fluids and electrolytes are at high risk for related cramping. Elderly individuals are also susceptible as the thirst mechanism can decline with age leading to chronic mild dehydration.
Overusing a Muscle Group
Using any muscle excessively and fatiguing it can trigger associated cramping as the muscle struggles to continually contract and support activity. This type of cramping is very common in athletes or those who are using muscles in rigorous or unfamiliar ways.
For example, someone who goes out for a very long run or bike ride without proper training may cramp up their leg and calf muscles which become overtaxed.
Muscle strain or injury
When muscles are strained, including microscopic muscle tears that induce inflammation, this injury and swelling can irritate nerves and prompt cramping. Similarly, if scar tissue accumulates in a muscle after an injury, it can impair muscle mechanics in a way that induces cramping. Smoldering muscle injuries are a common cause of recurrent cramping.
Pregnancy
Pregnant women commonly deal with muscle cramping, particularly in the later stages of pregnancy. While the exact mechanisms are uncertain, cramping may be related to reduced circulation and compression of nerves in the extremities from the weight and position of the growing fetus.
Inadequate nutrition and hydration as pregnancy progresses or interacts with nausea and vomiting may also play a role. Cramping often affects the calves, thighs, or feet.
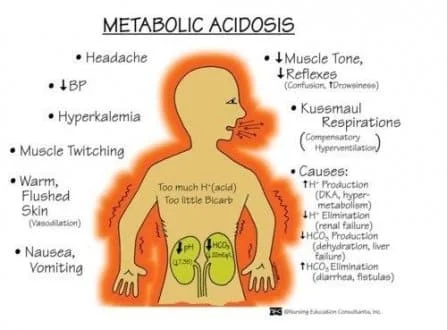
Liver Disease
Individuals with liver disease specifically cirrhosis of the liver are prone to muscle cramps, especially in the calves and feet. These cramps happen because liver disease disrupts the body’s ability to properly regulate plasma levels of electrolytes. Abnormal sodium regulation leads to impaired neural signaling to muscles and promotes cramping. These muscle cramps can be severe and persist for long periods.
Managing these cramps involves addressing the underlying liver dysfunction through dietary changes or medications to reduce associated fluid retention. Electrolyte supplements may also help restore balance.
Thyroid Issues
Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can make individuals more susceptible to muscle cramps. In hyperthyroidism, the excess thyroid hormone boosts metabolism which drives electrolyte imbalances and altered neuromuscular signaling.
This leads to painful cramping sensations, especially in the thigh region or calf muscles. In contrast, hypothyroidism reduces blood flow and slows neural conductivity which can trigger muscle immobility and cramping from inefficient relaxation of muscle fibers. Optimizing thyroid function under an endocrinologist typically helps minimize further cramping. Making appropriate dietary adjustments can also offset electrolyte losses.
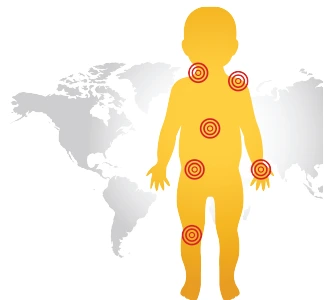
The most common locations for muscle cramps
Calf Cramps
Calf cramps are one of the most prevalent types of muscle cramps and can affect the gastrocnemius muscle or soleus muscle of the lower leg. Typically calf cramps are felt low down in the belly of the muscle rather than higher up near the knee. The cramp causes a visible hard knot in the muscle which stands out under the skin and is very painful to the touch.
Calf cramps tend to strike with active pointing of the ankle and toes such as walking up stairs or even when just lying in bed. Relieving a calf cramp can sometimes be achieved by gently straightening out the ankle which stretches the muscle fibers. Persistent calf cramps can be a sign of nerve root impingement or inadequate blood flow.
Thigh Cramps
Thigh cramps most commonly impact the hamstring muscles or quadriceps muscles of the upper leg. A quad cramp causes pain in the front of the thigh while a hamstring cramp is felt in the rear of the thigh. In addition to pain, an actively cramping thigh muscle will visibly bulge, feel very firm to the touch, and make it difficult to walk or bend the knee.
Thigh cramps are especially common later in long-distance running races when muscles become fatigued. Quickly stretching the thigh by bending at the hip can help relax a thigh cramp. Underlying lumbar spine issues that irritate nerves leading to the thigh should be ruled out.
Foot Cramps
Foot cramps often strike at night and affect muscles on the underside of the foot like the flexor digitorum brevis muscle situated above the arch. This muscle helps curl the toes downward which is why foot cramps cause painful balling of the toes which cannot relax.
Cramping makes the bottom of the foot feel extremely tense and tender with the sensation that radiates up from the arch. Walking around to stretch out the foot can undo the muscle contraction. Foot cramps may be associated with compression of nerves in the lower spine. Tight calf muscles or shoes with inadequate support may also contribute.
Hand Cramps
Cramps in the hand often manifest as a painful contraction of the palm muscle which forms the fleshy part of the hand below the thumb. This causes the fingers to tightly contract into the clasped palm, making it very difficult to open the hand or use it. The hand becomes locked in the cramped position and any attempt to extend the fingers increases discomfort.
The cramped hand muscle may visibly bulge out. These hand cramps tend to come on without warning and may wake someone up. Hand stretching exercises can unwind the sustained contraction. Hand cramps can be due to the compression of nerves that supply the hand as they exit the neck vertebrae or arm bone.
Abdominal Cramps
Abdominal muscle cramps cause sudden tightening and often severe pain in the abdominal wall muscles including the rectus abdominus or obliques. The tightly tensed abdominal muscles feel very firm to the touch during an episode of cramping. Sufferers are unable to relax the contracted muscles for a period lasting up to a few minutes leading to distress.
Changing body position to curl over the abdomen can help shorten these excruciating episodes. Persistent abdominal cramping can occur due to pinched nerves or disc issues in spinal segments supplying the abdomen. Cramping may also accompany gastrointestinal issues. Women may experience more frequent abdominal cramping during ovulation or menstruation.
Symptoms
- Sudden sharp muscle pain
- Involuntary contraction and tense knotting feeling
- Persistent tightness that does not ease up
- Muscle stiffness, tenderness, and temporary immobility
- Muscle cramping repetitively or for long periods
- Difficulty in stretching the contracted muscle
- Visible bulging muscle contour
- Discomfort using an affected muscle group
- Cramping interfering with activities
Risk Factors
Age
Muscle cramps become more common with advancing age. Older adults lose muscle mass and strength which makes muscles prone to cramping episodes. Also, neural conductivity and blood flow diminish putting muscles at risk.
Pregnancy
Pregnant women frequently deal with muscle cramps which seem related to nerve compression, decreased circulation, nutrition issues, and changing biomechanics. Cramping often starts in the second trimester and further increases through the third trimester and late pregnancy.
Deconditioning
Individuals who are sedentary and physically deconditioned are more susceptible to muscle cramps during and after physical activities due to fatigue, strained muscles, and poor oxygenation and nutrient delivery. Unaccustomed movements also provoke cramping.
Prior Injury
If a muscle suffers strain or tearing and still has residual scar tissue or swelling, this damage can irritate nerves and make that muscle group prone to painful cramping. Past injuries are a major risk factor.
Medications
Certain classes of medication like diuretics, statins, and steroids negatively impact electrolyte balance and muscle function which can increase cramping risk. Underlying conditions warranting these medications also contribute to risk.
Diagnosis of Muscle Cramps
Muscle cramps are usually diagnosed based on the characteristic symptoms. A detailed history and physical exam can help rule out serious medical causes.
There are no specific diagnostic tests for ordinary cramps. However, if the cramps are frequent, persistent, or unexplained, lab tests may help uncover potential causes:
- Blood tests to check electrolyte levels (sodium, potassium, calcium, magnesium)
- Blood tests to assess kidney or thyroid function
- Blood tests looking for muscle enzymes as markers of muscle injury
- Nerve conduction studies checking neural signals to muscles
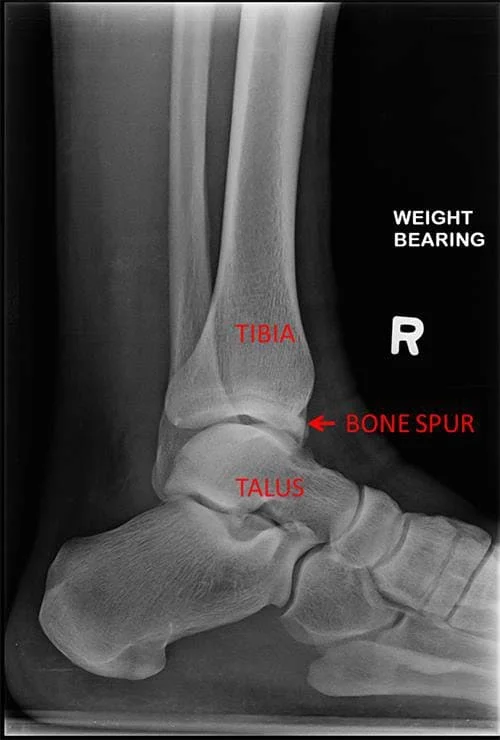
Imaging like an MRI or ultrasound may also visualize muscle tissue damage or nerve compression that could contribute to cramping.
When to See a Doctor
See a doctor promptly for evaluation if:
- Cramping arises after a new medication starts
- Cramps are accompanied by muscle weakness
- Cramps prevent the use of a muscle group
- Cramp symptoms rapidly worsen
- Swelling emerges around a cramping muscle
- Cramps disrupt sleep or daily activities
- Cramps coincide with an unexplained fever
- Potentially concerning health changes accompanying cramping
- Cramps are limited to 1 side of the body
- History of back injury with nerve issues
- Cramp relief interventions are unsuccessful
- Cramps commence without a clear trigger
Getting checked urgently is advised if cramps:
- Follow recent trauma from a fall or accident
- Cause severe muscle stiffness or spasms
- Progressively limit mobility
Early medical assessment can uncover serious causes like neurological, autoimmune, or vascular conditions warranting rapid treatment.
Treating Active Muscle Cramps
When a muscle cramp strikes, the following interventions may help provide relief:
- Gently stretch and massage the cramping muscle – Stretching activates the muscle’s inhibitory reflexes to promote relaxation. Massaging increases blood flow. However, stretching should be done carefully to avoid potential torn muscle fibers.
- Apply heat – Heat pads, heated rubs, warm wet towels, or a bath can encourage muscle relaxation and boost circulation to unknot the muscle. The direct warmth also eases pain.
- Hydrate with electrolyte-rich fluids – Replacing fluids and electrolytes can swiftly correct deficits driving the cramping. Sports beverages, coconut water, or oral rehydration solutions are ideal.
- Over-the-counter analgesics – Ibuprofen or naproxen sodium can temporarily alleviate cramp discomfort while also reducing any muscle inflammation.
- Walk around cautiously – Light activity and muscle contraction-relaxation cycles can unwind the sustained contraction once a cramp begins easing. The activity boosts blood flow as well.
- Ice after cramp passes – Applying ice packs after cramping stops helps reduce residual soreness and inflammation to prevent future episodes.
- Sit or lay in a position of comfort – Find a neutral body position that most relieves distress until the cramp dissipates.
Preventing Muscle Cramps
Various lifestyle measures and interventions can help prevent muscle cramps:
- Stay well hydrated daily and replace electrolytes – Consuming sufficient water and fluids containing sodium, potassium, magnesium, and calcium is key.
- Stretch and strengthen muscles – Flexibility, massage, yoga, and strength training bolsters muscle function.
- Increase physical activity gradually – Slowly ramp up the duration and intensity of exercise programs.
- Wear supportive footwear and orthotics if needed – Proper shoes are vital for foot and calf health.
- Address medical conditions proactively – Managing issues like thyroid disorders, circulation deficiencies, or mineral imbalances when present.
- Review medications with doctors – Adjustments to prescriptions may help if side effects are causing cramps.
- Apply heat before intense activity – Pre-warming muscles protect from strain and fatigue prompting cramps.
- Consider supplements if deficient – Magnesium, vitamin B complex, fish oil, and coenzyme Q10 aid muscle function.
Making muscles less prone to cramps involves nurturing strength, flexibility, blood flow, and neural signaling. Lifestyle adjustments, equipment modifications, and proactive treatment of underlying medical root causes all play a role.
Outlook and Complications
For the majority of individuals, muscle cramps are typically benign, self-limited events that resolve on their own without medical intervention. Especially with preventative lifestyle measures, most people only deal with sporadic cramping that poses little long-term consequence.
However, some individuals experience recurrent and persistent cramping several times a week that starts to significantly impair activities and quality of life. This frequent cramping warrants medical workup and management which usually can successfully control symptoms.
Overall, muscle cramping lacks serious complications. However in high-level athletics or occupations requiring extensive physical exertion, recurrent disabling cramps may necessitate changes or accommodations.
While ordinary muscle cramps pose low risks, a few scenarios where complications can arise include:
Torn Muscle Fibers
If an already tightly contracted muscle enduring cramping is forcefully stretched, some of the muscle fibers and connective tissue can tear leading to a muscle strain injury. This causes delayed onset muscle soreness and predisposes to future re-injury at the same site.
Intense Inflammation
Rarely, very forceful cramping can induce swelling, inflammation, and myositis in the muscle tissue prompting even worsening pain and stiffness that is slow to settle. The affected muscle suffers damage.
Link to Serious Disorders
While atypical, severely painful, recurrent, and disabling muscle cramps that continue to progress and do not respond to interventions can indicate an underlying neurological, vascular, or autoimmune condition requiring intensive treatment. Examples range from multiple sclerosis to peripheral nerve disorders, to compartment syndrome.
So while ordinary cramping is limited, inadequate precautions combined with other risk factors can permit complications in some patients. Seeking early medical advice to investigate persistent, treatment-resistant, and worsening cramping aims to identify those rare cases warranting advanced management.
Summary
Muscle cramps are characterized by sudden, involuntary, and painful contractions of muscles. While typically harmless, they can negatively impact the quality of life when severe or frequent. Understanding the common causes like dehydration, exercise overuse, muscle fatigue, pregnancy, and some medical conditions enables targeting preventative lifestyle changes like hydrating properly and gradually increasing physical activity.
Muscle cramps frequently occur in regions like the calves, thighs, feet, and hands. Initial treatment when a cramp strikes involves gently stretching the muscle, massaging the area, and applying heat. Hydration and electrolyte replenishment also provide relief. Preventing cramps requires daily maintenance interventions like fluid intake, muscle conditioning exercise, proper footwear, managing underlying medical conditions proactively, and considering supplements in some cases.
Most muscle cramps resolve on their own without long-lasting consequences. Still, severe inflammation, torn muscle fibers, and aggravated strains represent some possible complications. And rarely, cramp disorders resulting from an underlying neurological or vascular pathology necessitate urgent medical attention to halt progression. Evaluating persistent and treatment-resistant cramping identifies these rarer secondary conditions.
In summary, for most healthy active adults, muscle cramps only pose a temporary nuisance that can be minimized through lifestyle optimization. Staying vigilant regarding changes, worsening symptoms, or linked health concerns ensures treatment-responsive secondary causes are discovered. With preventative care, individuals can achieve reliable muscle performance and mobility.
FAQs
Are muscle cramps serious?
For most people, muscle cramps are not a serious concern and are resolved on their own without needing significant intervention. They become serious if they recur frequently, fail to respond to treatment, are associated with other symptoms, or are from an underlying condition.
How can muscle cramps be prevented at night?
Nighttime muscle cramps can be prevented by staying hydrated before bed, doing regular stretching, having a snack if needed, wearing loose clothing that doesn’t constrict circulation, avoiding cool ambient temperatures, and supplementing magnesium or potassium if deficient.
What should I do when a muscle cramp strikes?
When a muscle cramp hits, stop what you’re doing and gently stretch and massage the cramped muscle. Apply heat packs or take a warm shower. Drink electrolyte fluids. Over-the-counter pain medication can provide relief too. Gently walk around if able to encourage circulation.
What nutrients help prevent muscle cramps?
Getting enough hydrating fluids, magnesium, calcium, potassium, sodium, and vitamin B complex in your diet aids muscle function and cramp prevention. Supplementing with magnesium, coconut water, or electrolyte tablets can also help those prone to frequent cramping.
Could my medication be causing muscle cramps?
Yes, certain medication classes like diuretics, statins, steroid medications, and some asthma medications are linked with muscle cramping as a side effect for some patients. Do not stop taking the prescription if you think there may be a connection; instead, talk to your doctor about possible changes or substitutes.
References
Muscle cramp – Symptoms and causes – Mayo Clinic. (2023, March 7). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/muscle-cramp/symptoms-causes/syc-20350820
Professional, C. C. M. (n.d.). Muscle Spasms (Muscle Cramps). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/muscle-spasms-muscle-cramps#management-and-treatment
Higuera, V. (2019, August 27). What Causes Muscle Cramps? Healthline. https://www.healthline.com/health/muscle-cramps#prevention
Barrell, A. (2023, April 11). Why do muscle spasms happen? https://www.medicalnewstoday.com/articles/muscle-spasms





One Comment