Parkinsonian Gait
The gait is the name given to our walking pattern. When we walk, our bodies are normally upright, not leaning forward or backward, with an even stride and arms swinging to the sides. When we stand upright, the center of gravity is held in place, allowing us to maintain good balance.
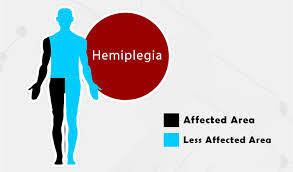
What is a Parkinsonian gait?
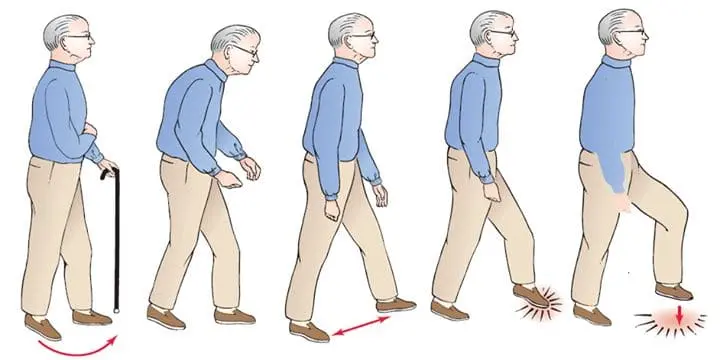
Parkinsonian gait is a clear sign of Parkinson’s disease, especially in its later stages. Compared to other Parkinson’s symptoms, it is commonly thought to have a worse impact on life quality. People with Parkinsonian gait typically take small, shuffling steps. It may be difficult for them to stand again.
Parkinsonian gait abnormalities can be periodic or constant. Periodic changes, like a stiff gait, might happen suddenly and unexpectedly. Continuous change refers to walking with ongoing adjustments to your gait, such as walking more slowly than you originally thought.
The capacity to start moving depends on a person’s capacity to flex the foot, bend the knee, and shift onto the ball of the foot. It can be challenging for people with Parkinsonian Gait to begin walking because it lacks the knee and foot flexion of normal movement. Turning can be slow and awkward due to the inability to swing or turn the leg, and uneven surfaces, slopes, and steps can be nearly impossible to negotiate.
Introduction
Parkinsonian gait is one of the many motor symptoms, such as tremors and slowness of movement, that are characteristic of Parkinson’s disease. Parkinson’s disease motor symptoms include difficulty beginning muscular movements and a loss of control over motions.
It is likely due to weaknesses in balance and postural stability that this patient group has a higher incidence of falls and fractures. When dealing with balance disruptions from a rear waist pull, individuals with Parkinson’s disease display unique weight-shift behaviors. Compared to healthy, age-matched controls, they perform a modified ankle joint action before takeoff and land with a posterior weight shift.
Although specific features of Parkinsonian gait can vary from person to person, the majority of people share several pervasive characteristics.
Among them are;
- Going more slowly than you should be moving at your age while festinating
- When your steps seem shorter and less deliberate than usual, as though you’re rushing
- Lowering your arms while walking,
- Falling a lot, and losing your gait
Individuals who suffer from Parkinson’s disease may become trapped in one spot because they are unable to stand up again. Dopamine insufficiency in the basal ganglia circuit, which results in motor impairments, is the cause of this illness. Although there are many other Parkinson’s disease symptoms, one of the most affected motor features of this ailment is gait.
Environmental circumstances including passing through a crowded area, changing directions, or walking through a tiny doorway might cause a person’s gait to freeze. Emotions can also set it off, particularly a rush of worry.
Small shuffling steps and general slowness of movement (hypokinesia), or in severe cases, complete immobility (akinesia), are characteristics of Parkinsonian gait sufferers. While double support duration is enhanced, patients with Parkinson’s disease (PD) have shorter stride lengths, walking speeds, and cadence rates during free ambulation. The patient not only has difficulty stopping once they start, but they also struggle to quit. Muscle hypertonicity is to blame for this. A person’s gait might freeze at any time. But that usually happens when you get up. You may discover that you are unable to stand up and move.
Parkinsonian gait can be managed with various treatments, such as medication, physical therapy, and assistive technology like canes or walkers. People with Parkinson’s disease should collaborate closely with their medical professionals to create a personalized treatment plan that takes into account their unique needs and symptoms.
How does the doctor assess freezing and gait?
An evaluation of your gait requires a doctor to inquire about your clinical history. A thorough neurological examination might also be required. Your first step, reduced arm swing, walking speed, stride length, difficulty making turns, and foot clearance are all things the doctor may check for.
Additionally, timed tests may be employed, and the physician may attempt to induce a freezing of gait by having you turn, walk through small spaces, or perform two tasks at once. Your physician might advise you to visit the physiotherapist for a more thorough evaluation and treatment.
What are the particular causes?
Dopamine production decreases and nerve cells in the basal ganglia, a region of the brain, start to break down in Parkinson’s disease. Dopamine helps the basal ganglia establish connections between neurons. This suggests that reduced levels of dopamine result in less interactions.
The smooth motion of your body is the result of the basal ganglia. When there are less connections in that area of the brain, it cannot perform its function as well. Parkinson’s disease movement symptoms, including Parkinsonian gait, result from this.
Abnormal gait characteristics:
Heel-to-toe characteristics:
People with Parkinson’s disease have different stride characteristics from healthy individuals.
In a normal gait, the heel touches the ground before the toes (a motion known as heel-to-toe walking). However, in a Parkinsonian gait, the entire foot touches the ground at the same time (a motion known as flat foot strike) or, less frequently and in the later stages of the disease, toe-to-heel walking (a motion in which the toes touch the ground before the heel). Furthermore, during the swing phase of gait, patients with Parkinson’s disease have decreased foot raising, resulting in a reduced gap between their toes and the ground.
Parkinson’s disease patients experience less impact when their heel strikes. Analyses have indicated that this progression is correlated with the severity of the ailment, and its influence decreases with time. Parkinson’s patients also tend for the forefoot regions to have larger relative loads along with a shift in load towards the medial foot parts. It is thought that this load shift aids in compensating for postural instability. When comparing Parkinson’s disease (PD) patients to normal individuals, it is discovered that the intra-individual diversity in foot strike patterns is remarkably reduced.
Ground reaction force vertically:
The push-off force from the ground causes the second peak on the vertical ground reaction force (GRF) plot, which appears during normal gait. The first peak appears when the foot hits the ground. InParkinson’s disease , the vertical GRF signal has an odd form. Lower forces (or peak heights) are observed in the early stages of the disease for heel contact and the push-off phase, similar to those of older participants. In patients with Parkinson’s disease (PD), the vertical GRF signal has only one narrow peak throughout the most advanced stages of the ailment, when short, shuffling steps characterize gait.
Falls and freezing of gait:
Parkinsonian gait is frequently characterized by two episodic phenomena: falls and freezing of movement. Falls and freezing of gait are commonly believed to be closely related in Parkinson’s disease (PD) for some reasons, chief among them being that both symptoms are more prevalent in the latter stages of the disease and less prevalent in the earlier stages, and freezing of gait frequently results in falls. Treatment with dopaminergic medication generally results in unsatisfactory and occasionally paradoxical responses from both symptoms, which may indicate a shared underlying pathophysiology. It is possible to show a poor and illogical dopamine-producing medication response with a demanding Approach that assesses gait both during the entire ON medication state and after medication withdrawal.
Freezing of Gait: Usually a brief episode lasting less than a minute, Freezing of Gait (FOG) is characterized by halted gait and complaints from the patient that his or her feet are immobile. Walking should be reasonably easy once the patient gets past the block. Though little is known about the pathophysiology of the phenomena, it most likely involves a dispersed functional-anatomic network. Unfortunately, the benefits of the existing treatments for FOG are somewhat limited.
The most frequent type of FOG is “start hesitation,” which occurs when the patient wishes to begin walking. “Turning hesitation” is next in frequency. Additionally, FOG can be felt when walking through a doorway or other small space, when rearranging one’s steps to get to a destination, and during stressful events such as when the doorbell or phone rings or the elevator door opens. As the illness worsens, FOG may manifest on its own even in an open runway area. It has been demonstrated that psychological therapies can lessen the detrimental effects of psychosocial factors, such as depression or anxiety, which might exacerbate tremors or freezing of gait in Parkinson’s patients. Accordingly, psychological intervention could be beneficial for all patients, not only to lessen pain, anxiety, despair, and sleeplessness but also to lessen the impact of psychosocial factors in exacerbating motor symptoms.
Falls: Similar to FOG, falls are uncommon in the early stages of the illness and increase in frequency as it worsens. The main causes of falls are abrupt alterations in posture, especially when the trunk is turned, or attempting to walk or balance while doing many tasks at once. Falls also frequently occur when transferring, like getting out of a chair or bed. In 45% of all falls, PD patients fall forward, and 20% fall laterally. Falls that happen often at an early stage of the disease could indicate that another diagnosis, like progressive supranuclear palsy, has to be taken into care.
Posture sway:
The inability to maintain balance during daily activities including walking, turning, and getting up from a chair is a common symptom of postural instability in end-stage Parkinson’s disease (PD). People with advanced Parkinson’s disease (PD) fall because they are unable to maintain proper bodily balance with their center of mass over the base of support and because their motions are inflexible due to increasing rigidity. When a patient has cerebellar ataxia, a stroke, or a head injury, their postural sway in a normal posture normally increases, although it frequently decreases in Parkinson’s disease patients. This is because not enough flexibility in changing postural responses seems to be the issue with Parkinson’s disease. These patients’ inclination to fall is increased by this inflexibility.
What causes gait issues in Parkinson’s disease?
It is unclear why some people with Parkinson’s disease have difficulty walking while others do not.
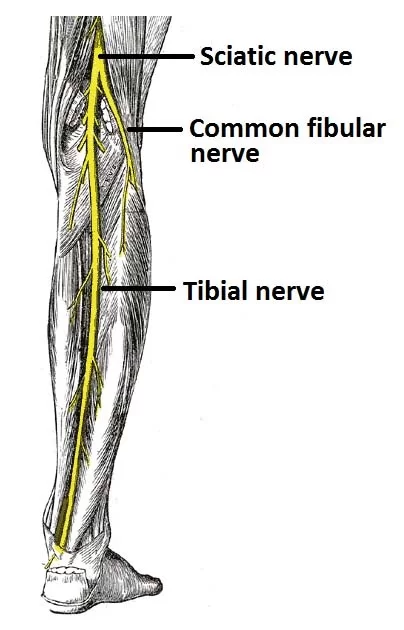
Walking is controlled by a very intricate brain circuit that has numerous connections between different parts of the brain, including;
- The motor cortex is in charge of organizing and triggering movement.
- Movement-regulating brain cells are found in the basal ganglia.
- The cerebellum facilitates motor coordination.
Signs of Parkinson’s gait changes:
A physician evaluating Parkinson’s disease is looking for a few typical signs.
They could consist of;
- Walking more slowly than usual
- Slow motion
- Lower movement of the body
- Close-together placement of the feet
- Very little or no arm swing
- Problems changing
- Instead of landing on the heel, the feet land flat.
- Tiny, rapid movements
Freezing, or not being able to lift one’s feet off the ground People most frequently freeze when they are turning, are just getting started, are passing through small spaces, or are approaching their destination. It can also happen when someone’s focus is diverted by something.
Typical Parkinson’s Disease Gait Pattern:
As the disease worsens and symptoms worsen, people with Parkinson’s disease frequently have additional abnormalities in their stride. Among the impairments are,
- Hypokinesia, or taking shorter steps at a slower pace
- Reduced ability to co-ordinate
- Destination, characterized by shorter steps and higher cadence
- The inability to produce effective steps at the beginning of gait or the total halt of stepping during gait is known as freezing of gait
- Having trouble multitasking while walking
These gait abnormalities are accompanied by a higher chance and frequency of falls. Elevated likelihood of falls impacts a person’s freedom and capacity to engage with others in the community, in addition to raising the risk of injuries like hip fractures. Furthermore, fear of falling has psychological repercussions and can cause sadness and self-isolation.
Kinematics of Gait:
Variations in the hip and ankle joint’s excursion are among the alterations in gait kinematics. As the condition progresses, the patient may have a toe-heel sequence or a flat foot in place of a heel-toe development. Parkinson’s patient walks in a more primitive manner as if they have lost their mature gait pattern. Walking across carpets or stepping over obstacles is made more difficult by the flat-footed gait. Based on a three-dimensional gait learning, plantar flexion is decreased at the terminal stance. Ankle excursion may be affected by changes observed in hip flexion as well. The time of the combined excursion appears to be intact in terms of quality, though.
Pathophysiology:
According a particular conceptual terms, festinating gait may be caused by reduced equilibrium responses. The person will either fall entirely or keep taking brief, running-like steps if walking is just a series of controlled falls and if usual reactions to falling are either delayed or insufficient. Bradykinesia is one condition where abnormal nervous system terminating may lead to ever shorter steps. The entire range of motion would be reduced if the motor unit is unable to increase its frequency to a sufficient level or if it stops in the middle of the motion. This would result in shorter strides when walking. Alterations in the gait’s kinematics may also lead to fascination.
How does it come out?
A variety of motor symptoms, such as Parkinsonian gait, are associated with Parkinson’s disease in addition to tremors and slowness of movement.
While individual differences may exist in the particulars of Parkinsonian gait. The majority of people have a few really different characteristics. Among them are the following;
You are walking slower than is appropriate for someone your age or when you start to take shorter, smaller steps, which can give the impression that you’re rushing. Gait freezing and frequent falls are the results of walking with fewer arm movements.
Festination, stooped posture, and freezing are examples of Parkinsonian movement patterns that are likely to worsen over time. Your range of motion may alter as you get older, which could make you less active. Your reflexes and muscles may become weaker as a result. This can therefore lead to musculoskeletal changes that worsen hunched shoulders and poor posture, which increases the chance of falling.
If you begin to become less mobile or feel unsteady, it is easy to lose confidence because of a fear of falling. It’s critical to get guidance on gait improvement since it may affect your social life and general quality of life.
Treatment:
As of right present, Parkinson’s disease has no recognized remedy. There are currently no medications that can halt or slow the disease’s natural course. The majority of Parkinsonian disease patients take medication to lessen their symptoms. Walking difficulties may be managed with the aid of dopamine-related medications, however, the more severe the condition, the less effective these medications are.
Parkinsonian gait can be treated with levodopa (L-dopa) and other drugs that increase the brain’s production of dopamine or improve its use of it. The primary treatment for all Parkinson’s disease symptoms is the use of these drugs. Carbidopa is a drug that is frequently taken in combination with levodopa (L-dopa). This drug prevents levodopa (L-dopa) from being broken down by the body before it reaches the brain.
When combined with levodopa (L-dopa), deep brain stimulation has also been proven to improve Parkinsonian gait in some patients. Little wires are inserted into the areas of the brain that regulate movement during deep brain stimulation. The wires are attached to an apparatus that supplies the brain with constant electrical pulses, just like a pacemaker does for the heart.
Deep brain stimulation and medication can assist in treating gait problems in Parkinson’s disease patients, but their efficacy is generally lower than that of other Parkinson’s symptoms. For instance, prolonged use of levodopa (L-dopa) and related drugs may raise the chance of gait freezing. This is because if you consume medications for an extended time, their effects may begin to change during the day. If this occurs, you may occasionally feel a freeze of gait when the medication’s effects aren’t as strong.
Focus strategies:
Parkinson’s disease (PD) patients have demonstrated improved gait by actively paying greater attention to walking and practicing each stride before taking it. Occasionally, a partner walking along with the patient prompts them to focus on their gait or gives them a visual cue to step over by placing a foot in front of the person with Parkinson’s disease. This diverts the patient’s attention from the involuntary activity of walking and forces them to focus on the stepping action, turning it into a voluntary effort and avoiding the malfunctioning basal ganglia pathway. It has also been demonstrated that Parkinson’s disease (PD) patients’ gaits can return to normal by avoiding simultaneous tasks that call for either motor or cognitive attention.
Exercise:
Exercise and physical treatment have been demonstrated to improve gait characteristics in people with Parkinson’s disease.
By developing training plans that lengthen a patient’s stride, widen their base of support, enhance their heel-toe gait pattern, straighten their posture, and enhance their arm swing patterns, physiotherapists can aid in improving their gait.
Walking on a treadmill while wearing an overhead harness can improve walking speed and stride length during gait training. The harness assists the patient in maintaining an upright posture by eliminating the need to use a mobility aid a practice that frequently promotes a forward-flexed posture. It is believed that the central pattern generator is activated, which leads to an improvement in gait patterns.
Increased balance and a better walking pattern have been linked to strengthening the lower extremities and core muscles as well as increasing trunk flexibility. Strengthening and balancing are also enhanced by cardiovascular exercises like water aerobics and cycling in pairs. Owing to the degenerative nature of Parkinson’s disease, maintaining an exercise regimen is crucial to preserving its advantages.
Enhanced upright postural alignment can also be achieved with techniques like employing a vertical walking pole. To help the patient put their feet more accurately and extend their base of support, the therapist may also utilize tiles or footprints on the floor. It has also been demonstrated that mentally practicing the desired movement and engaging in the creative imagination of walking with a more normalized gait pattern is beneficial.
Walking over a range of surfaces, such as grass, tile, carpet, or foamed surfaces, should also provide a challenge for the patient and help them get closer to normalizing their gait pattern.
Gait training:
The term “Parkinsonian gait” refers to a distinct, less steady walk caused by changes in posture, slowness of movement, and a shorter stride.
Physiotherapy aims to maintain your body in the best possible functional state so that you can continue to move independently and safely. Joining multidisciplinary teams, which are groups of specialists from various fields that collaborate to help you manage your symptoms and enhance your quality of life, is a common practice for physical therapists, also known as physiotherapists.
Physiotherapists use exercise and other forms of physical therapy to help you keep your independence in daily life. Physiotherapists practice in hospital and community settings in addition to in patients’ homes.
The primary goals of physical therapy for Parkinson’s disease are:
- To reduce the risk of falling, to keep an individual’s strength and flexibility
- To continue walking in a secure manner
- To preserve and enhance independence and functional ability
- To enhance and correct balance and posture
- To improve daily tasks (like rising from a chair and getting out of bed)
If freezing is obvious, coping strategies such as auditory or visual cues to increase manual tasks (reaching and grabbing), breathing exercises to maintain respiratory function, and teaching of relaxing techniques to inform caregivers and enhance freezing, may be taught.
Depending on the stage of the disease that a patient is experiencing, physiotherapy goals will be different.
Early phase:
- In the early stages of the condition, the main objectives are to prevent inactivity and improve physical ability in terms of muscle strength, joint mobility, and aerobic capacity.
- Your physiotherapist can provide you with advice on how to maintain your fitness levels as well as an exercise program that you can do on your own or with others.
Middle phase:
- At this point, the goals of physical therapy will be to improve posture, balance, gait, and transfers in addition to improving upper limb function, especially in terms of reaching and gripping.
- A range of exercises, including hand exercises to enhance manual adaptability so you can, for example, button a shirt more easily, may be suggested by your physical therapist to help with these tasks.
- Additionally, he or she may collaborate with an occupational therapist to secure your home and reduce your risk of falling.
Late phase:
- Currently, the goal of physiotherapy is to prevent problems that might arise from bedridden or wheelchair-using individuals.
- To do this, you will need to keep your breathing steady, avoid pressure sores, and work with your caregivers to make sure you are positioned correctly and they are safe while lifting you.
Focus on Balance:
- When your inner ear which helps with orientation interacts with what you see (visual feedback) and how your feet feel the ground beneath them, you get a proper balance.
- Your stride (the way you walk) may become unstable due to damage to this balancing system caused by Parkinson’s disease, which may cause anxiety in crowded or public places.
- Exercises involving walking, or gait training, have advantages.
- Any exercises designed to increase balance should be supervised by a physical therapist as they can help you identify any issues with balance and teach you how to get around them.
Stretching and flexibility:
- Patients with Parkinson’s disease often have a tense calf, hamstring, and hip flexor muscles.
- To combat that stiffness, it’s important to stretch regularly throughout the day as opposed to just once.
Strength Training:
- Everyone needs strength training because age-related muscle weakness exists.
- However, there’s an indication that people with Parkinson’s disease may find their lives more challenging as a result of muscular weakness.
- Depending on your condition’s stage, a therapist might ask you to do resistance exercises with light dumbbells or a resistance band (a thick rubber band).
- Exercises in a pool that develop muscle by using the resistance of the water can also be advantageous.
What self-care techniques can I use?
Given that the benefits of medication for improving gait are limited, it’s critical to consider how you can better yourself by modifying your gait and utilizing helpful signals.
You might benefit from the following advice:
- When you walk, look forward rather than down at your feet.
- When you walk, pay attention to keeping your posture straight.
- Standing up against a wall with your head, shoulders, hips, and heels all in contact with the wall will help you become more conscious of your posture.
- You can take longer steps by lifting your toes and firmly planting your heel on the ground after each step.
- Walk long and maintain focus on the length of your stride to prevent it from getting shorter over time.
- Keep your arms swinging by your sides.
- Steer clear of talking or doing anything else while you’re walking.
- Shoes with crepe soles or high heels should be avoided as they may “snap on the ground.
- Stretching exercises are a good way to increase the range of motion and decrease stiffness or rigidity.
- To lessen freezing, experiment with various methods.
When does Parkinsonian gait disappear?
Parkinson’s disease is a progressive condition. There is presently no treatment for the symptoms it causes, which include altered gait.
Yet the above-discussed therapies may lessen the symptoms of Parkinsonian gait and enhance a person’s quality of life. Consult a physician about beginning gait rehabilitation.
Summary
Parkinson’s disease (PD) is primarily described as a brain degenerative condition that damages brain regions involved in motor control. Among PD patients, shuffling gait, poor balance, and freezing gait are the most common motor dysfunctions.
Early-stage Parkinson’s disease may cause problems with postural control and walking. Slower gait, less arm swing, shorter steps, postural instability, and a loss of disassociated arm and trunk movements during gait are the characteristics that define them.
Some Parkinsonian gait characteristics, such as festination, stooped posture, and freezing, are likely to worsen with time. Your range of motion may change over time, making you less active and reducing muscle strength and reflexes. This, in turn, can cause musculoskeletal changes that worsen poor posture and stooped stance, increasing the risk of falling. It is simple to lose confidence due to a fear of falling if you become less mobile or feel unsteady. It’s crucial to get guidance on how to correct your gait because it could affect your social interactions and general quality of life.
Parkinson’s disease has no known treatment. Most individuals will experience a progressive Parkinsonian gait. Parkinson’s gait will worsen if therapy or treatment is not received. With treatment, it can get better.
Changes in nerve cells within the part of the brain responsible for controlling movement lead to changes in gait. It’s not a disease of the muscles. It can be beneficial to take part in therapies and exercises that stimulate the nervous system and brain.
FAQs
The neurological system and the body’s nerve-controlled areas are both impacted by Parkinson’s disease, an ongoing neurological condition. The onset of symptoms is gradual. A tremor in one hand that is hardly visible may be the initial symptom. Though tremors are typical, the illness can also make you stiff or move more slowly.
Loss of control in brain regions responsible for producing purposeful and smooth movements causes gait alterations and freezing, as do most motor symptoms that may be experienced by patients with Parkinson’s disease (PD), such as muscle stiffness, tremor, and slowness.
Parkinson’s disease (PD) is primarily described as a brain degenerative condition that damages brain regions involved in motor control. Among PD patients, shuffling gait, poor balance, and freezing gait are the most common motor dysfunctions.
Parkinsonian Gait, also known as Parkinson’s Walk, is distinguished from normal adult gait by very short, shuffling steps in which the feet do not lift very high off the ground.
Patients with Parkinson’s disease (PD) may exhibit an abnormal gait pattern in the early stages of the disease, which is identified by a shorter stride length, increased stride variability, decreased walking speed, and festinating gait.
Those with Parkinson’s disease (PD) had lower self-selected walking speeds, stride lengths, swing times, and hip excursion than healthy controls. Moreover, PD patients showed double support time and a higher cadence. Walking speed is decreased on both treadmills, though the difference is less for the treadmill.
During free walking, patients with Parkinson’s disease show recognized alterations in their foot’s heel-to-toe motion, even in mild or moderate stages of the disease. Parkinsonian gait elements are most likely the result of natural processes in patients that help them avoid becoming unsteady while walking.
Stubbornness or rigidity
Slow movement caused by bradykinesia.
Uncontrollably shaking or trembling body parts
Difficulties maintaining balance and posture.
Difficulties moving or walking.
Physical therapists are essential in helping people with their gait improvement. Together, you and your physical therapist will create a treatment plan that will help you achieve your unique objectives. Your physical therapist will create a customized treatment plan for your particular issue.
Keep your arms at your sides free and adaptable while maintaining a back-and-down stance with your shoulders. Retain a back-and-down stance with your shoulders and keep your arms at your sides free and flexible.
People with Parkinson’s disease usually have a narrow base of support when walking.
Early on in Parkinson’s disease (PD), postural control and gait dysfunction can arise. Their gait slows down, arm swing is lessened, steps are taken shorter, postural instability occurs, and disassociated arm and trunk movements during gait are lost.
Free Walking
Observing the patient’s gait constitutes the testing component. The patient should ideally walk back and forth several times in a hallway that is at least ten feet long in order to increase the possibility of detecting any abnormalities that may be present. Typical gait abnormalities related to Parkinson’s disease are these.
These walking disturbances can be divided into two categories based on how they appear.
Continuous
Episodic
Some drugs can help with Parkinson’s gait. Levodopa is the most widely used. When taking their medication as prescribed, some people report an improvement in their gait. For some, medication can effectively control other symptoms, but gait abnormalities persist.
Walking regularly can significantly enhance a person with Parkinson’s disease’s capacity to lead an autonomous and satisfying life. A mere 20 to 30 minutes of vigorous walking each day has been shown to improve flexibility, gait, balance, and tremor, and slow the progression of Parkinson’s symptoms.
References:
- Parkinsonian walk. January 16, 2024. Parkinsonian gait on Wikipedia, https://en.wikipedia.org Reference within the text: Parkinsonian Gait (2024)
- E. Hersh (2018) 18 September. Understanding Parkinsonian Gait. Parkinson’s disease: https://www.healthline.com/health/gait Reference within the text: Hersh, 2018
- Veazey, K. September 29, 2022. Knowledge about the gait of Parkinson’s patients. Parkinson’s disease gait and treatment: https://www.medicalnewstoday.com Reference within the text: Veazey, 2022
- Complete Citation: Key Information for Patients with Parkinson’s Disease About Gait Disorders and Freezing. (As of now). Gait disturbances and freezing in Parkinson’s disease: https://www.movementdisorders.org/MDS/Resources/Patient-Education.htm Reference inside text: (PARKINSON’S DISORDER AND FREEZING: ESSENTIAL INFORMATION FOR PATIENTS, n.d.)
- Gait. (No date). Parkinson’s Europe. Parkinson’s Europe’s website about the condition, symptoms, motor symptoms, and gait Citation within the text: Gait (n.d.)
- A., & A. (November 7, 2023). What Is Parkinsonian Gait and How Can It Be Made Better? NexStride *. What is a Parkinsonian gait and how can it be improved? https://www.getnexstride.com/blog/ Reference inside text: (2023)