Platelet Rich Plasma Therapy
Introduction
Platelet-rich plasma (PRP) is a regenerative medicine treatment that uses a patient’s own blood platelets to promote healing. Platelets are tiny blood cells that contain growth factors, which are proteins that help to repair and regenerate tissues.
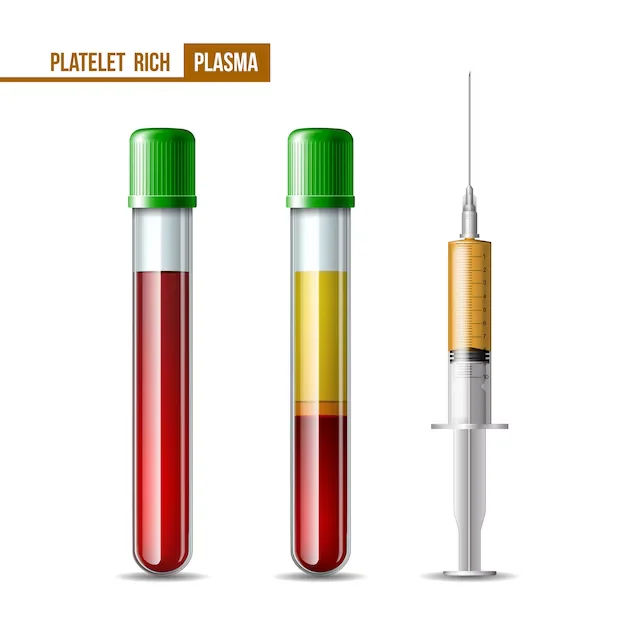
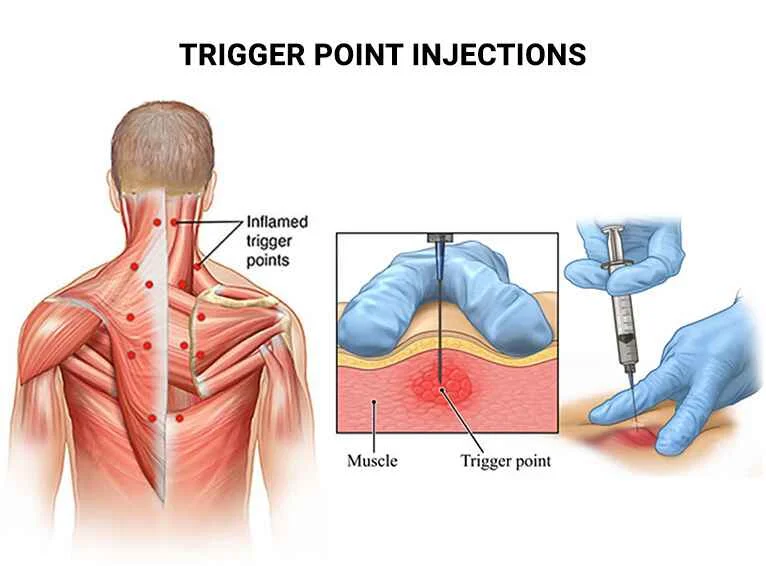
PRP therapy is typically performed by drawing a small amount of blood from the patient and then using a centrifuge to separate the platelets from the other blood cells. The concentrated platelets are then injected into the area of the body that needs to be healed.
Physicians and researchers alike face difficulties when treating chronic, complex musculoskeletal ailments that take a long time to recover. Orthobiologics is a relatively that offers intriguing new opportunities to encourage and hasten the healing of bones and soft tissues by using naturally occurring substances derived from biological sources (such as cell-based therapies). An orthobiologic called platelet-rich plasma (PRP) has lately acquired favor as an adjuvant therapy for musculoskeletal problems.
It is a quantity of platelet concentrate-containing fractionated plasma made from the patient’s own blood. Several growth factors, including platelet-derived growth factor, transforming growth factor-ß, insulin-like growth factor, vascular endothelial growth factor, and epidermal growth factor, are abundant in the alpha granules of the platelets and play important roles in tissue repair mechanisms.
Through the administration of supra-physiological quantities of autologous platelets at the site of tissue damage, PRP has found use in a variety of surgical domains to improve bone and soft tissue repair. PRP is a viable therapeutic strategy for upcoming regeneration treatments because of its relatively simple preparation, usefulness in the clinical setting, favorable safety profile, and potential positive outcome. PRP’s method of action is, however, poorly understood, and this has led to doubts about its potential effectiveness and application.
Definition
A component of the plasma fraction of autologous blood with a platelet concentration above baseline is known as platelet-rich plasma (PRP). ‘Orthobiologics’ is the name of a new medical field that focuses on this kind of therapy. The goal of this practice is to improve the body’s inherent ability to regenerate and restore itself. As a safe, non-surgical, biological treatment for osteoarthritis and musculoskeletal rehabilitation, PRP therapy has recently attracted a lot of attention.PRP needs to be utilized very carefully right now.
Platelet physiology and function
93% red blood cells, 6% platelets, and 1% white blood cells make up the majority of a blood sample. These are tiny discoid cells, and they have a lifespan of seven to ten days. Platelets are triggered after an injury that results in bleeding, and they group together to release their granules, which contain growth factors that promote the inflammatory cascade and healing process. The majority of the study over the last century has been concentrated on the primary function of platelets, which is hemostasis as well as the development of new connective tissue and revascularization. The body releases growth factors, which are proteins involved in healing when platelets are activated. There are many different types of growth factors, but their combined effects may speed up tissue and wound healing.
The idea behind PRP therapy is to reverse the red blood cell: platelet ratio by concentrating platelets that contain a potent combination of growth factors to 94% and reducing red blood cells to 5% (which are less helpful in the healing process). A healthy person’s normal platelet count ranges from 150,000 to 450,000 cells per microliter of blood. The tissue reparative efficacy with PRP can be expected with a minimum increase of five times the normal concentration of platelets (approximately 1 million platelets/l), whereas much higher concentrations did not show further enhancement of wound healing. Platelet concentrations of less than 1,000 106/ml were not reliable for enhancing wound healing. It is still unclear what concentration is optimal. It is still unclear what concentration is best. The wide range of platelet concentrating tools and procedures employed in various research may change platelet degranulation properties that could influence clinical outcomes, making it difficult to interpret the findings.
Clinical feature
The most frequent factor causing extreme chronic pain and physical impairment is “need.”. Including ligament and tendon injuries, soft tissue injury accounts for up to 45% of all musculoskeletal injuries. Chronic and degenerative musculoskeletal issues can be challenging to treat and have a protracted course, which can interfere with an otherwise active lifestyle. Due to overuse or sports-related injuries, many of these people may require surgery, protracted durations of rehabilitation, and uncertain results. Furthermore, there are currently not many medicines that could greatly enhance mending in the face of these ongoing issues. Interest in the use of PRP therapy for articular cartilage repair, the treatment can reduce the symptoms of osteoarthritis. If successful, this non-operative treatment method for osteoarthritis would be revolutionary.
Growth factors in platelet-rich plasma
The notable components of PRP presented include transforming growth factor (TGF)-ß, platelet-derived growth factors (PDGF-AB and PDGF-BB), insulin-like growth factor (IGF), vascular endothelial growth factors (VEGFs), epidermal growth factor (EGFs) and fibroblast growth factor (FGF)-2. TGF-ß1 and PDGF stimulate the proliferation of mesenchymal cells. TGF-ß1 also stimulates extracellular matrix production, including collagen. Principally, these factors stabilize the damaged tissue during the initial stages of tissue repair and direct the local mesenchymal and epithelial cells to migrate, divide, and increase collagen and matrix synthesis, which ultimately results in the creation of scar tissue and fibrous connective tissue.
VEGF and FGF-2 play an important part in promoting the growth of new blood vessels that provide nutrients and progenitor cells to the site of injury; however, other substances are also necessary for neo-vascularization.
By over-expressing IGF-1, PRP is hypothesized to enhance the early repair of tendon lesions. IGF-binding proteins carry the 70 amino acid polypeptide hormone, which is a typical component of plasma. It is unknown how IGF-1 is stored in platelets because IGF-1 in PRP whereas the majority of proteomic studies have found IGF-1 in platelets. Due consideration should be given to PRP as an adjunctive therapy for particular applications given its significance in numerous healing pathways.
Clinical Application For Platelet-Rich Plasma
PRP therapy was reportedly first used in an open heart surgery. PRP was used in the dental field to promote accelerated wound healing in cancer patients following jaw reconstruction. PRP has been utilized by doctors to help speed up soft tissue recovery after plastic surgery as well as bone repair after spinal injury. PRP became a popular but unproved therapy for sports-related injuries as a result of the media attention.
Currently, PRP injections are being used in various applications, including orthopedics, cardiovascular surgery, cosmetics, maxillary surgery, and urology As a result, PRP’s mechanism of action, refines the treatment and formally demonstrates efficacy in placebo-controlled trials.
Platelet-rich Plasma Treatment
Three steps explain how easy it is to apply for PRP. The doctor collects venous blood and transfers it to the centrifuge for the majority of orthopedic use, which is currently done in an outpatient environment. Depending on automation and centrifuge processing standards, processing blood typically takes between 5 and 20 minutes once it is in the machine.
A sterile barrier can also be required. According to the most recent recommendations, the platelet concentration should be increased by a factor of four to six above the baseline value. The doctor extracts PRP according to the centrifuge’s instructions when it completes processing. By adding thrombin and calcium chloride, which cause the release of these substances from the alpha granules, the platelets contained in PRP can easily be activated. With wider approval of PRP treatment, its application is selectively being adjusted for use in the operating room while surgery is in progress.
Variations In The Preparations Of Platelet-Rich Plasma
For researchers to better understand the relative success or failure of different PRP preparations, it is important to have this classification. This can also create an objective method for future study and progress.
Platelet-leukocyte-rich plasma (PLRP) merits special notice as a unique concept, even though the evidence is anecdotal. When treating wounds with soft tissue abnormalities, PLRP which is rich in growth factors and antimicrobial proteins has been used to address infection issues. the use of PLRP in a high-energy soft tissue injury that was also infected showed that the number and concentration of platelets and leukocytes were sufficient to start the healing process despite the presence of the infection.
Mechanisms of Action
Potential modes of action
PRP lacks proper reporting of the precise formulation used when treating orthopaedic disorders, ranging from acute rotator cuff injuries to chronic Achilles tendonitis. Because harvested platelets that have been activated by endogenous thrombin and promoted by the addition of calcium chloride deliver growth factors slowly, it is generally believed that the application of autologous plasma rich in growth factors is advantageous in restoring connective tissues. It is true that the particular processes via which PRP works are not well understood.
Benefit of PRT
Bone formation
In the presence of bone morphogenetic protein (BMP)-2, BMP-4, BMP-6, or BMP-7, bone formation PRP and its soluble fraction enhance the osteoblastic differentiation of myoblasts and osteoblastic cells in three-dimensional preparations. Additionally, in the presence of BMP-4, heparin-binding fractions isolated from serum enhanced osteoblastic differentiation. These findings suggested that platelets carry unique potentiators for BMP-dependent osteoblastic differentiation in addition to growth factors for proliferation.
Osteoarthritis
Hyaluronic acid (HA) generation is controlled by platelet-released growth factors (PRGFs), which lubricates and protects cartilage. Synovial fibroblasts isolated from arthritic patients secrete more HA and are stimulated to produce hepatocyte growth factor (HGF) by PRGF. The maximum level of fibroblast proliferation and PDGF concentration were produced in the various treatment lysates by pre-incubating platelets in an acidic environment (pH 5.0). Intra-articular PDGF delivery may help restore HA concentration and change angiogenesis to a more balanced state, but it does not stop IL-1ß’s effect on synovial cells.
Tendon healing
By stimulating cell proliferation and increasing the production of angiogenic factors throughout the healing process, administering autologous platelet-rich clots may be helpful in the treatment of tendon injuries. Cultured tendon cells produce VEGF and HGF in the presence of growth factors from PRP clots, with the levels produced being noticeably larger with supernatants from platelet-rich clots than with supernatants from platelet-poor clots.
Another noteworthy fact was that the thrombin inhibitor hirudin had no effect on the supernatants’ ability to induce mitosis. Both platelet-rich and platelet-poor clots improved cell proliferation and total collagen synthesis in human tenocyte cells. Matrix metalloproteinases (MMPs) and endogenous growth factors (TGF-ß and VEGF-a) are slightly more expressed in response to the former but not the latter.
Muscle healing
Anatomic continuity and function of the injured muscle are restored through the complex and dynamic process of muscle healing. In a small-animal model, local application of PRP has been shown to speed the healing process following a muscular strain injury.
Osteochondral defect repair
Macroscopic inspection, micro-computed tomography, and histological evaluation at 4 and 12 weeks with PRP in poly-lactic-glycolic acid revealed better healing in the osteochondral defect.
Tendon healing
PRP for tendon healing has been reported to improve IGF-1 overexpression-mediated tendon defect healing. The gene expression of the matrix proteins collagen type I (COL1A1), collagen type III (COL3A1), and cartilage oligomeric matrix protein (COMP) was found to be boosted in another investigation using equine tendons grown in 100% PRP without a related increase in the catabolic molecules MMP-3 and MMP-13.
According to certain research, PRP promotes neovascularization, which speeds up healing and increases the growth of scar tissue with higher histological quality. According to Lyras and colleagues, PRP has a substantial impact in the early stages of tendon regeneration since after 14 days, the mechanical properties of the regenerated tendon in the PRP-treated group showed a considerable improvement before returning to baseline at 28 days.
Applications for multiple medical disorders based on human clinical investigations
Even while doctors are increasingly embracing PRP as an alternative to drugs and surgery, it is still a relatively new treatment for orthopedic patients. There are a few RCTs on this topic, despite the fact that the majority of the literature has a low evidence level (case-control studies, case series, and anecdotal case reports). A new meta-analysis of six randomized trials from various clinical PRP applications indicated no significant effect from PRP use up to 24 months.
Articular cartilage repair
An arthroscopic fixation of a large (>2 cm) loose chondral body from the medial femoral condyle in the knee of an adolescent football player was followed by the injection of plasma rich in growth factors into the region between the defect and the fixed fragment. Despite the grim prognosis, total articular cartilage recovery was said to have been quickened, and the functional outcome was exceptional, accepting a quick return to athletic activity without symptoms.
Achilles tendon repair
A case-control (level 3 evidence) study comparing open suture repair with PRGF in six athletes and a retrospective comparison with six matched athletes who had a traditional surgical procedure for a complete Achilles tendon tear found that athletes receiving PRGF recovered their range of motion more quickly, showed no wound complications, and needed less time to resume light running and training activities. TGF-ß1, PDGF-aß, VEGF, EGF, and HGF significantly correlated with the number of platelets, and the cross-sectional area of the PRGF-treated tendons increased less.
These findings suggest that operative management of tendons combined with the use of autologous PRGF promoted enhanced healing and functional recovery. patients with surgical repair of Achilles tendon reported no extra benefit of PRP over standard therapy. The Achilles Tendon Total Rupture Score was lower in the PRP group, maybe indicating a harmful result. Although there was a variance in elasticity modulus, it was unclear how early biomechanics could be related to late clinical outcomes. In another independent RCT of patients with chronic Achilles tendinopathy, PRP therapy was no better in improving pain and activity compared to saline injection.
Anterior cruciate ligament repair
The ligamentization process after anterior cruciate ligament (ACL) restoration was evaluated in a human investigation to determine the impact of local platelet gel administration on graft healing in bone tunnels. Following ACL surgery, locally administered platelet gel accelerated early revascularization of the graft at the osteoligamentous interface zone. After 4 to 6 weeks, the group that had received platelet gel showed a noticeably higher amount of vascularization in the osteoligamentous interface, whereas neither group had evidence of revascularization in the intra-articular portion of the graft. Following ACL reconstruction surgery, the efficacy of local platelet-leukocyte gel administration on knee stability revealed dramatically improved anteroposterior knee stability at 6 months with PRP treatment.
Arthroplasty
The effect of autologous platelet gel given to exposed tissues, synovium, and the lining of the wound after closure following total knee arthroplasty has been looked at in a retrospective case-control investigation. Unexpectedly, patients who received platelet gel had less postoperative blood loss than control patients, as indicated by variations in preoperative and postoperative hemoglobin on day 3, less need for drugs, and a greater range of motion before discharge. Autologous platelet gel administration may result in better hemostasis, better pain management, and a shorter hospital stay. It was discovered that using autologous platelet gel and fibrin sealant during a unilateral total knee arthroplasty helped lower the number of blood transfusions after surgery.
Epicondylitis
PRP was found to be 25% more effective than normal corticosteroid therapy in reducing pain on the visual analog scale and Disabilities of the Arm, Shoulder, and Hand (DASH) outcome scores in patients with lateral epicondylitis. Both groups considerably improved over time when the baseline visual analog scale and DASH scores were compared to the results at the 2-year follow-up. The DASH scores of the PRP group remained noticeably improved whereas those of the corticosteroid group went back to their baseline levels. Additionally, there were no negative effects associated with the use of PRP. One platelet-rich plasma therapy improved pain and function scores in individuals who did not improve after six months of corticosteroid medication, according to another independent investigation.
Osteoarthritis
Following intra-articular infiltration of PRGF, patients with symptomatic knee osteoarthritis reported improvements in function and quality of life as assessed by both osteoarthritis-specific and general clinical assessment tools at 6-month follow-up. These results indicate that PRGF is a possible osteoarthritis treatment. With short-term efficacy, PRP injection therapy decreased pain and improved knee function and quality of life; the highest effect was seen at 12 months but reduced by 24 months.
Rotator cuff repair
Patients who had local administration of autologous PRP 30 days after surgery and had a full rotator cuff tear reported less pain. At three months following surgery, the treatment group’s scores on the Simple Shoulder Test, Constant, and strength in external rotation as assessed on a dynamometer were all significantly greater than those of the control group. After six months, however, no eternally noticeable changes were has been observed. Follow-up magnetic resonance imaging revealed a lack of variation between the two groups’ rotator cuff tear healing rates. The long-term outcomes of grade 1 and 2 tear subgroups indicate that PRP beneficially affected rotator cuff recovery. The use of an autologous platelet-rich fibrin matrix for the augmentation of a double-row repair of minor or medium rotator cuff injuries was not found to be effective by RCT. These findings, however, only apply to small and medium rotator cuff injuries, with a potential benefit of platelet-rich fibrin matrix for large and major rotator cuff tears that is not to be determined.
Sub-acromial decompression
patients evaluating the effect of platelet-leukocyte gel made from PLRP on the postoperative recovery of patients undergoing open sub-acromial decompression observed faster recovery, before return to daily actions, and reduced pain medicine necessity in the platelet-leukocyte gel-treated group.
Safety profile
Since PRP is made from autologous blood, there should be no chance of cancer, immune system responses, or disease transmission. The use of PRP is regarded as safe because to the unique and deep clinical expertise of the oral-maxillary sector with PRP and the thousands of patients treated thus far. Patients who receive a 6-month injection of plasma rich in growth factors (PRGF) into the knee joint do not experience any negative side effects in the musculoskeletal field.
While adverse reactions are uncommon, there is always a little possibility of injection site morbidity, infection, or damage to nerves or blood vessels. There have been reports of calcification and the development of scar tissue at the injection site. Modern procedures avoid using bovine thrombin because it has been shown to cause hypersensitivity. Life-threatening coagulopathies caused by the formation of antibodies against clotting factors V and IX have very occasionally been observed. There is currently no convincing proof that a local PRP injection has any systemic effects. The limited requirement for PRP injections in clinics (because PRP is not continuously provided) and RCTs that have thoroughly assessed the safety of PRP therapy are some likely defenses for these points.
Practical aspects and issues
The time commitment required to study and use the method, insurance coverage, informed consent, and sporting laws should all be taken into account by doctors who are considering adopting PRP in their practices.
Platelet-rich plasma therapy contraindications
Generally, PRP is well tolerated. Still, there are specific contraindications of PRP, such as:
- Blood cancer such as lymphoma or leukemia
- Active cancer on chemotherapy
- lower platelet count due to blood conditions like thrombocytopenia
- Pregnancy
- Chronic usage of blood thinners or anti-inflammatory medications like aspirin or ibuprofen
- Suspected septic arthritis or infection
- Injecting into a joint replacement
Limitations
PRP’s composition changes depending on the patient, the technology used to prepare it, the way and length of time it is stored until use, and whether or not it interacts with other biologics or substances. The current usage of PRP in orthopedics is patient-driven and based on anecdotal accounts of its use in elite athletes due to these inherent discrepancies. Platelet-rich plasma may improve soft tissue healing, particularly for tendons, but it may also prevent the development of new bone. During tissue repair, some doctors employ PRP to deliver and/or enhance growth factors and cytokines. Scar tissue and fibrous connective tissue can develop as a result of PRP. PRP is not osteoinductive, however.
Conclusion
PRP was a significant first step in the rapidly growing field of “orthobiologics,” which motivated researchers to take into account bone marrow aspirates and stem cells. The information that is now available indicates that PRP may be useful in increasing soft-tissue repair, especially for tendon and wound healing. PRP’s clinical use in bone healing and arthritis continues to be unclear. PRP is especially beneficial for specific revision operations with a poor healing environment as well as determined tendinopathies like patellar tendinitis and tennis elbow.
A lot of research is being done on the part of PRP in the focused stimulation of musculoskeletal and mesenchymal stem cells, and it shows promise as a short-term treatment that could help the simultaneous repair of several musculoskeletal tissues following trauma or elective surgery. As an additional method to bone grafting techniques, PRP has mixed rates of success. A healthy dose of caution should be used until clinical proof is available about the potential function of PRP in repairing musculoskeletal injuries, particularly in elite athletes. However, this is an interesting new area that could one day result in superior therapies. It needs to be prepared and used during surgery in the most effective way possible. Research is also required to evaluate the relative effectiveness of different treatments and to decide how to use them for improved recovery.
Note:
ACL: anterior cruciate ligament
BMP: bone morphogenetic protein
DASH stands for Arm, Shoulder, and Hand Disabilities.
EGF: epidermal growth factor
FGF: fibroblast growth factor
HA: hyaluronic acid
HGF: hepatocyte growth factor
IGF: insulin-like growth factor
IL: interleukin
MMP: matrix metalloproteinase
PDGF: platelet-derived growth factor
PLRP: platelet-leukocyte-rich plasma
PRGF: platelet released growth factor
PRP: platelet-rich plasma
RCT: a randomized controlled trial
TGF: transforming growth factor
VEGF: vascular endothelial growth factor
WADA: World Anti-Doping Association.
FAQs
Can I wash my face after plasma?
Avoid washing or using any other products. Continue keeping your skin dry and clean on the second and third days. FEIGN Plasma Aftercare Spray: LIGHTLY spritz the treatment region in the morning and the evening. You can sprinkle the region up to three more times per day if discomfort and itching persist (LIGHTLY; do not soak skin).
Does PRP treatment hurt?
Not at all. Blood removal from the elbow or forearm is easy. With ultrasound guidance, PRP injections into joints or tendons are also more tolerable. The injection may be a little bit more painful than other injections, though, because local anesthetic shouldn’t be utilized.
Resting the joint or tendon for at least a week is necessary after the injection. You should also take painkillers like paracetamol and codeine if necessary. It would be ideal if you stayed away from pain relievers like ibuprofen.
Generally, we estimate that 10% of patients get a short-term flare after PRP injections – more common in tendons than joints.
Does Platelet-rich plasma therapy work?
Yes, but not for all joint and tendon conditions.
PRP should be useful for the following musculoskeletal diseases:
Knee arthritis: We have 23 RCT trials showing PRP is better than placebo of other injectables.
Tennis elbow: A review of studies shows benefits compared to cortisone or placebo, but not all are positive.
Plantar fasciitis: 9 RCTs show PRP is better than cortisone for heel spurs or plantar fasciitis.
Gluteus medius tendonits or greater trochanteric syndrome. One good RCT shows PRP is better than cortisone.
In addition, there is increasing evidence that PRP is better than cortisone for rotator cuff tendonitis.
What happens after the PRP procedure?
The majority of people experience minimal to no discomfort after the injection, however, it is typical for the area to continue to swell and feel unpleasant for around 48 hours. Painkillers and ice can be used as needed during this time. On the fifth day after receiving an injection, the patient typically begins physical therapy and notices a dramatic improvement in their initial condition. Patients should avoid heavy lifting and intense activity for a few days after treatment but can resume work and other usual activities right away. When and if another injection is required, the doctor will follow the patient.
What are the advantages of this procedure?
PRP injections can significantly reduce pain and other symptoms for many patients, possibly negating the need for surgery or long-term medication. In comparison to other nonsurgical therapies, this one expedites the healing process and allows patients to resume their regular activities more rapidly. There is no chance of cross-reactivity, an immunological response, or the spread of a disease because the blood being injected is from the patient. PRP injections, as opposed to corticosteroid injections, promote recovery.
Are platelet-rich injections safe?
With any form of injection, there is always a chance of infection or clotting, but these issues are incredibly rare. Additionally, there is a small chance that a patient could experience an adverse reaction to a component of the operation. During this procedure, most people have no problems.
References
Dhillon, R. S., Schwarz, E. M., & Maloney, M. D. (2012). Platelet-rich plasma therapy – future or trend? Arthritis Research & Therapy, 14(4), 219. https://doi.org/10.1186/ar3914
Andia, I., Sánchez, M., & Maffulli, N. (2010). Tendon healing and platelet-rich plasma therapies. Expert Opinion on Biological Therapy, 10(10), 1415–1426. https://doi.org/10.1517/14712598.2010.514603
Andia, I., Sánchez, M., & Maffulli, N. (2011). Joint pathology and platelet-rich plasma therapies. Expert Opinion on Biological Therapy, 12(1), 7–22. https://doi.org/10.1517/14712598.2012.632765
Guadilla, J., Fiz, N., Andia, I., & Sánchez, M. (2011). Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip. Knee Surgery, Sports Traumatology, Arthroscopy, 20(2), 393–398. https://doi.org/10.1007/s00167-011-1587-9
Gupta, A. K., & Carviel, J. (2016). Meta-analysis of the efficacy of platelet-rich plasma therapy for androgenetic alopecia. Journal of Dermatological Treatment, 28(1), 55–58. https://doi.org/10.1080/09546634.2016.1179712






2 Comments