Spina Bifida
What is a Spina bifida (SPLIT SPINE)?
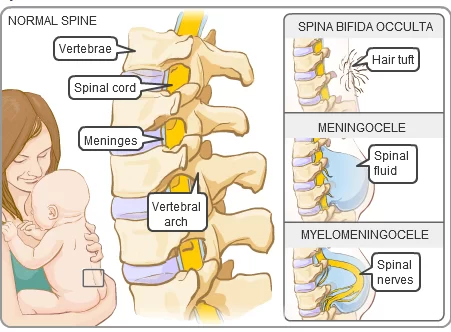
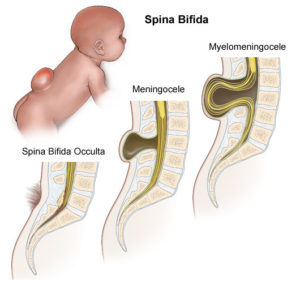
Spina bifida is one of the neural tube defects. In which the failure of the fusion of two vertebral arches in the embryological stages of the developmental spine.
- Spina bifida occulta: failure of fusion could be limited only to the spinous process.
- Spina bifida aperta: these include the neural elements(involving the vertebral arch, skin meninges, and cord) that may fail to fuse.
- Meningocele: In which there is a protrusion of meninges.
- Myelomeningocele: In which there is a protrusion of meninges and cord.
- Syringomyelocoele: IN which the central canal of the cord is dilated and the cord is protruded.
- Myelocoele: In which the central cord remains unfused and exposed.
Incidence of Spina Bifida:
Spina bifida is one of the most common birth defects, with a worldwide average incidence of 1-2 cases per 1000 births, but English and Europeans have a higher incidence than Asians.
The risk of recurrence after one affected child is 1 in 20, with a risk of a similar affected person passing defect After 2 affected risk of 1 in 10, and after 3 affected 1 in 4.
Causes of Spina Bifida:
Spina bifida is a neural tube defect ( often before the mother knows she is pregnant), normally closure of the neural tube occurs around 28 days after fertilization. However, if sometimes interferes and the tube fails to close properly, a neural tube defect occurs.
- UNKNOWN – the majority of the cases are unknown.
- MEDICATION – during pregnancy anti convulsants, diabetes.
- GENETICS – it could be run families and genetics basis.
- OBESITY – obese pregnant ladies are more prone.
- RAISED BODY TEMPERATURE – from fever or external sources such as hot tubes and electrical blankets.
- FOLIC ACID DEFICIENCY – contributing factor in the pathogenesis of neural tube defects.
Symptoms of Spina Bifida
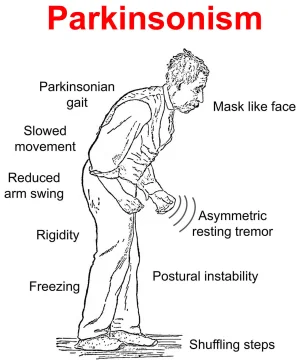
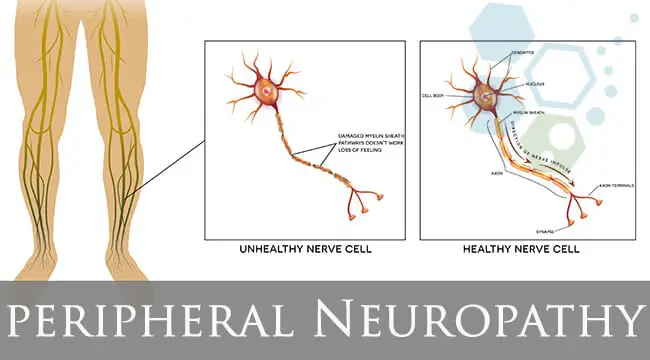
→ Muscle weakness of the legs, sometimes involving paralysis(flaccid or spastic)
→ Bowel and bladder problems.
→ Seizures, especially if the child requires a shunt.
→ depression or dimple in the lower back.
→ A small patch of dark hair.
→ Soft fatty deposits.
→ Port-wine nevi (deep red-purple macular lesions).
→ Saclike cyst that protrudes outside the spine.
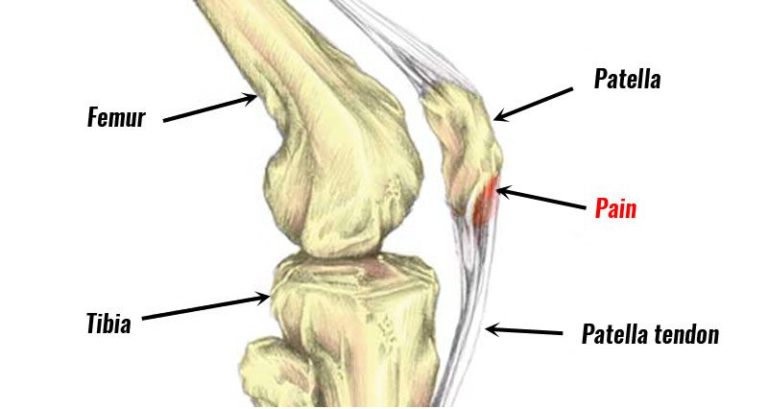
→ Musculoskeletal deformities (scoliosis, hip dysplasia, hip dislocation, club foot, hip/knee contracture).
→ Hydrocephalus, alone with Type I or II Arnold Chiari malformation.
→ Trunk hypotonia.
→ Delayed automatic postural reactions.
Diagnosis:
NEUROLOGICAL EXAMINATION
The purpose of the examination is to determine, the level at which normal cord function ceases, and to assess the presence and degree of hydrocephalus.
SKULL: for examination sutures and fontanelles were palpated for evidence of distension and increased pressure. Measurement of the occipital frontal circumference (OFC) should be carried out and charted.
CRANIAL NERVES: asses by observation of the movements of the face, tongue, and palate and by watching the baby suck.
SPINE: The spine should be palpated along its length as sometimes there are multiple lesion that are not always obvious. The length and width of the lesion should be measured and the position of the spinal cord noted.
LIMBS: check active movements of limbs by simulating the leg and eliciting neonatal reflexes. The power of muscle should be assed by with and without gravity and with and without resistance. these are useful in checking deformities such as talipes and congenital dislocation of the hip.
BOWEL AND BLADDER: sphincter tone and bladder function should be assessed. A patulous anus and dribbling incontinence are associated with a lesion at the level of S2,3and 4. Retention of urine is associated with a lesion at S1.
First physical assessment of a child. The movement of the leg in some babies appears after the back is repaired, but the movement of the back is lost after the back is repaired in some cases.
This assessment of both – sensation and movement both. First record general impression – abnormal position of the limb, deformities present, movement (if any) present.
Reflex assessment, muscle testing.
sensory chart completed and to do testing with a safety pin, testing the epicritic feeling or light touch as with cotton wool. The most reliable test at this stage is pinprick with a pin then baby cry.
Physiotherapy Treatment:
Physical therapy programs are designed to parallel the normal achievement of gross motor milestones.
1. Physical therapists in the intensive care unit address infant positioning needs and provide parent and family education.
2. Early-intervention physical therapists can provide physical therapy in the home or other community-based locations to help encourage the child’s development of strength, movement, and balance skills by teaching parents specific play-based exercises.
3. School-based physical therapists often consult with other educational team members to help students with spina bifida participate in curricular activities, and develop independence within the school setting. They may recommend special equipment for the student to use during the school day.
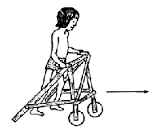
4. Physical therapists also recommend appropriate equipment, such as braces, walkers, and wheelchairs to help people with spina bifida increase their functional mobility.
5. Physical therapy is also important for the prevention of other possible problems, such as obesity, by identifying activities that encourage continued participation in sports or other fitness-based activities that promote lifelong health and wellness.
Neonatal physiotherapy:
Prone lying facilitates – educate the mother to place the baby in a prone position during playtime, preferably on the floor.
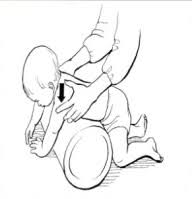
A passive movement must be given in a full range of motion possible to all joints starting with the toes, tarsal joints, ankle, knee, and hip. Mother must teach to how to carry a baby and move. Arm movement can be started as soon as possible as the baby responds to the exercise to strengthen the shoulder girdle.
Knowledge of developmental progress is the milestone of a normal child then starting to roll over, sitting up.
Play therapy with toys -facilitate mid-line activity, Bridging, knee to chest.
Ambulation
When the child is ready to stand, an assessment needs to be made of the degree of support required from orthosis. degree of support required according to a neurological level of affection.
FAQ
Can spina bifida be treated?
Although there is no known treatment, most spina bifida patients live long lives. Individuals with spina bifida have unique medical problems and abilities. Occulta, meningocele, myelomeningocele, and closed neural tube abnormalities are the four forms of spina bifida.
Can people with spina bifida ever walk?
Individuals with spina bifida use many methods of mobility. These include using wheelchairs; walking with braces, crutches, or walkers; and walking without any help at all. Individuals who have spina bifida in the region of the spine around the head may experience wheelchair-dependent paralysis in their legs.
Can you live a long life with spina bifida?
Individuals with milder forms of spina bifida who do not have any other significant health issues can anticipate a normal lifespan. However, life expectancy may be shortened for children with more severe forms of spina bifida or other related health issues (such hydrocephalus).
What deficiency causes spina bifida?
Lack of folic acid
One of the most significant variables that can raise your chances of having a kid with spina bifida is not getting enough folic acid during pregnancy. Some foods, like broccoli, peas, and brown rice, naturally contain folic acid, commonly referred to as vitamin B9.
Is spina bifida harmful?
The backbone that covers the spinal cord is not formed and closed properly when the neural tube closes partially. Nerve and spinal cord injury is a common outcome of this. Mild to severe intellectual and physical problems may result from spina bifida.



3 Comments