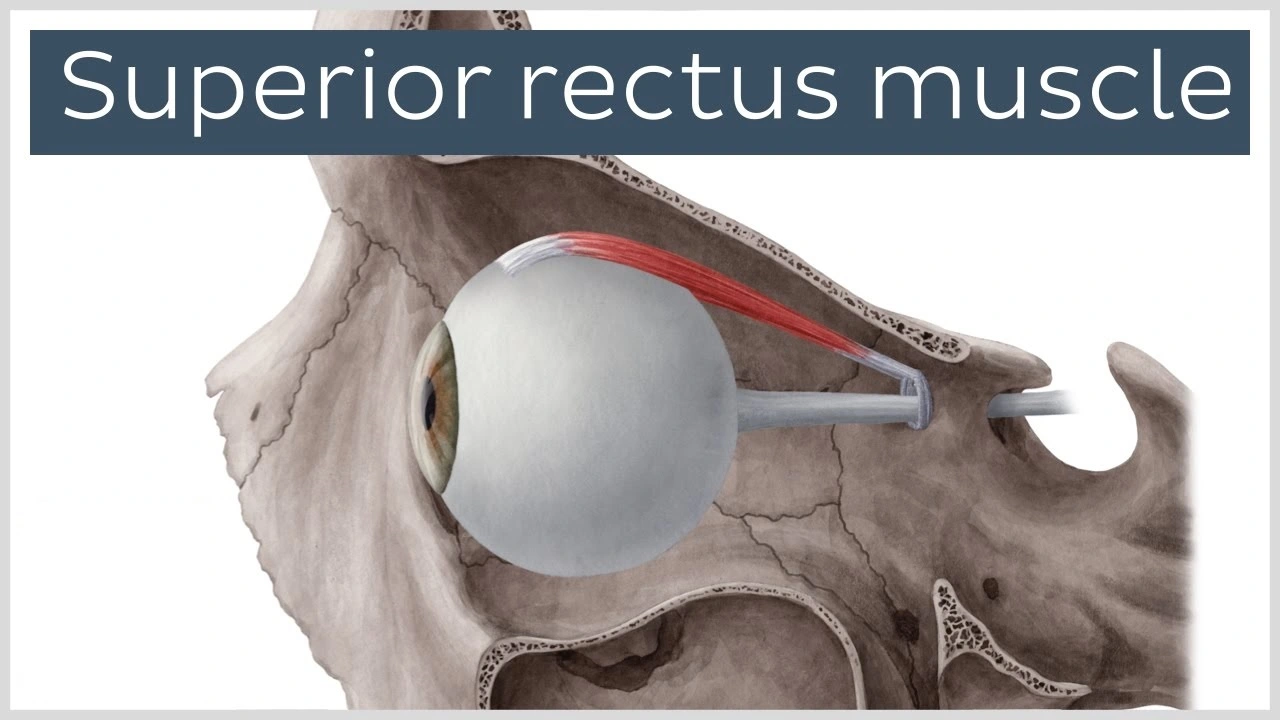
Superior Rectus Muscle
Introduction :
The superior rectus is one of the 7 extraocular muscles. There is a total of 4 rectus muscles, 2 oblique muscles, and the levator palpebrae superioris. The superior rectus is one of the 4 rectus muscles, which also include the superior rectus, the medial rectus, and the lateral rectus. The oblique muscles are the 1. superior and 2. inferior obliques. The levator palpebrae superioris is mostly responsible for eyelid elevation.
Structure and Function :
With the head and eyes facing straight forward, the eyes are said to be in primary gaze. From this position, an activity from an extraocular muscle produces a secondary or tertiary action. Although the globe can be moved about 50 degrees from its prior position, usually during normal eye movement only 15 degrees of extraocular muscle activity occur before head movement begins.
The annulus of Zinn is the common origin point for the rectus muscles and travels the superior orbital fissure and orbital apex. It consists of superior and inferior tendons. The superior tendon is involved with the entire superior rectus muscle as well as parts of the medial rectus and lateral rectus muscles. The inferior tendon is involved with the inferior rectus muscle and parts of the medial rectus and lateral rectus muscles.
The superior rectus has a primary action of elevating the eye, causing the cornea to roll superiorly. The superior rectus originates from the annulus of Zinn and goes anteriorly and superiorly over the globe, making an angle of 23 degrees with the visual axis. This angle induces the secondary and tertiary actions of the superior rectus muscle to be adduction and intorsion (incycloduction).
Each of the extraocular muscles has a functioning insertion point, which is at the closest point where the muscle first reaches the globe. This point creates a tangential line from the globe to the muscle origin and is known as the arc of contact. The superior rectus includes an arc of contact of 6.5 mm, as does the inferior rectus.
Embryology :
The mesenchyme of the head, including the orbit and its designs, arises in mesoderm and neural crest cells primarily. The extraocular muscles originate from the mesoderm, but the satellite and connective tissue of the muscle emanate from neural crest cells. Most of the remaining connective tissue of the orbit also is emanated from neural crest cells.
Blood Supply and Lymphatics :
The superior rectus obtains blood primarily from the superior muscular branches of the ophthalmic artery, with some contribution from two anterior ciliary arteries. The primary blood supply for all of the extraocular muscles is the muscular parts of the ophthalmic artery, the lacrimal artery, and the infraorbital artery. The two muscular units of the ophthalmic artery are the superior and inferior muscular branches.
Venous drainage is similar to the arterial system and drains into the superior and inferior orbital veins. Usually, there are a total of four vortex veins, and these are seen at the lateral and medial sides of the superior and inferior rectus muscles. These vortex veins empty into the orbital venous system.
Nerves :
The superior rectus is supplied by the superior division of cranial nerve III (oculomotor). Cranial nerve III is divided into upper and lower branches, with the upper branch innervating the superior rectus and levator palpebrae superioris and the lower division to the medial rectus, inferior rectus, and inferior oblique. The lateral rectus is supplied by cranial nerve VI (abducens), and the superior oblique is supplied by cranial nerve IV (trochlear).
Muscles :
The superior rectus and inferior rectus are vertical rectus muscles. Medial and lateral rectus muscles are both horizontal rectus muscles. Each of the rectus muscles arises posteriorly at the annulus of Zinn and courses anteriorly.
Each of the rectus muscles inserts on the globe at differing distances from the limbus, and the curved line drawn along the insertion points makes a loop that is known as the spiral of Tillaux. Beginning at the medial part of the globe, the medial rectus inserts at 5.5 mm from the limbus, the inferior rectus inserts at 6.5 mm from the limbus, the lateral rectus muscle inserts at 6.9 mm from the limbus, and the superior rectus muscle at 7.7 mm from the limbus. The medial and lateral recti insert with the horizontal meridian, while the inferior and superior recti insert along the vertical meridian.
The superior rectus has a 10.6 mm width at its insertion on the globe. The tendon is 5.8 mm, gauged from the origin. The total length of the muscle is 41.8 mm.
Extraocular muscles have a big ratio of nerve fibers to skeletal muscle fibers. The ratio is 1:3 to 1:5; additional skeletal muscles are 1:50 to 1:125. Extraocular muscles are a technical form of skeletal muscle with a variety of fiber types, including both slow tonic types, which oppose fatigue, and saccadic (rapid) type muscle fibers.
Physiologic Variants :
The size of the inferior rectus muscle, its insertion point on the globe from the limbus, and further anatomical measurements may vary widely from one individual to the next. The numbers defined in this article reflect average distances. Congenital discrepancies in extraocular muscles can cause ocular misalignment.
Surgical Considerations :
The nerves of the rectus muscles and superior oblique muscles insert into the muscles at one-third the distance from the origin to the insertion. This makes injury to these nerves during anterior segment surgery difficult but not impossible. Instruments that are advanced 26 mm posterior to the rectus muscle insertions can provoke injury to the nerve.
Blood vessels may be injured during surgery of the superior rectus muscle. The vessels which supply blood to the extraocular muscles also supply closely all the temporal half of the anterior segment of the eye. Most of the nasal half of the anterior segment circulation also emanates from blood vessels that supply the extraocular muscles. Therefore, care must be taken during surgery of the superior rectus or further extraocular muscles to avoid disrupting this blood supply.
Other complications of this may result from superior rectus surgery, which also may result from other rectus muscle surgery. Insufficient alignment is the most ordinary complication and may require additional surgery to correct. Refractive changes may happen when two rectus muscles of one eye are operated on; this may resolve over months. Other possible surgical complications contain diplopia, perforation of the sclera, and postoperative infections. Although uncommon, serious infections may result after the strabismus surgery, including pre-septal or orbital cellulitis and endophthalmitis.
The superior rectus muscle associates partially with the levator palpebrae superioris muscle; thus, procedures targeted toward the superior rectus may also cause changes in the upper eyelid. When the superior rectus is resected, the palpebral fissure may tighten, and the eyelid may come forward. When the superior rectus muscle is adjourned, the palpebral fissure may widen, and the eyelid may be pulled upward.
Clinical Significance :
The function of the superior rectus muscle can be assessed along with the additional extraocular muscles during the clinical exam. The action of the extraocular muscles can be assessed by having the patient look in nine directions starting with a first gaze, tracked by the second positions (up, down, left, and right) and the third positions (up and right, up and left, down and right, down and left). The clinician can test these positions by keeping the patient following the clinician’s finger and tracing a wide letter “H” in the air. The superior rectus muscle is isolated by asking the patient to heighten the eye in full abduction.
Ocular alignment can be tested also using several methods, including cover tests, corneal light reflexes, different image tests, and dissimilar target tests. Since many patients with extraocular muscle exceptions are young children, the clinician may need to employ various clever means such as using toys or other objects to evoke the cooperation of the child.
Strabismus, or ocular misalignment, can be generated by abnormalities in binocular vision or abnormalities of neuromuscular control. Weakness, injury, or paralysis that applies to the superior rectus muscle can be involved in strabismus.
Superior rectus palsy :
It is an eye condition resulting from injury to the third cranial nerve or a branch thereof. As the name indicates, the oculomotor nerve supplies the majority of the muscles controlling eye movements (four of the six extraocular muscles, excluding only the lateral rectus and superior oblique). Injury to this nerve will result in an inability to move the eye normally. This nerve also supplies the upper eyelid muscle (levator palpebrae superioris) and is accompanied by parasympathetic fibers innervating the muscles responsible for pupil contraction (sphincter pupillae). The limits of eye movement resulting from the condition are generally so severe that patients are often unable to maintain normal eye alignment when gazing straight forward, leading to strabismus and, as a consequence, dual vision (diplopia).
Oculomotor palsy can occur as a result of several different conditions. Non-traumatic pupil-sparing oculomotor nerve palsies are usually referred to as a “medical third,” with those affecting the pupil being known as a “surgical third.”
Superior rectus exercises :
Eye massage :
Eye massage works to assist relieve strain and stress while massaging the muscles that surround and support the eyeball. Conducting the exercise once per day will make sure the muscles are stretched and limber. See a comfortable position and close your eyes. Place the thumb gently below the eyebrow and on the inside corners of the eye close to where the eyes meet the nose. Place the other four fingers on the forehead. Apply force inward utilizing the thumbs and count to four. Using the index finger and thumb of either hand, massage the nose’s bridge and count to four as pressure is given. Reprise the exercise four times.
Exciting information about superior rectus :
When the eye is in a fully abducted position, the superior rectus is the best muscle that can elevate it. Traumatic injuries of the rectus muscle tend to be fairly rare. Rupturing of the inferior rectus muscle is usually referred to as a blowout fracture. When damage has been described following a trauma, it is usually associated with extensive ocular and orbital damage.
Severed or disinserted muscles are one of the main difficulties of strabismus surgery. When examining cases like these, the eye should not be forced into the opposite field of action where the suspected muscle is. It could generate the muscle to slip back and pierce the site within Tenon’s capsule.
FAQ :
What is the superior rectus?
The superior rectus is an eye muscle, that controls the eye as it moves up. This muscle is among four muscles — including the medial rectus, lateral rectus, and inferior rectus — which control the eye’s movement
What happens if the superior rectus muscle is weak?
Weakness of the superior rectus muscle has nominal clinical implication. In some patients, Bell’s phenomenon may be reduced, but this rarely changes the approach to therapy in children. On rare occasions, you may see a patient that cannot look up.
How does the superior rectus enter the eye?
At the site of its insertion, the superior rectus penetrates the fascial sheath of the eyeball (Tenon’s capsule), which in turn reflects on the muscle’s tendon and creates a thin fascial sleeve.
What is the superior rectus innervated by?
The superior rectus is a muscle that lives in orbit. As one of the extraocular muscles, it is innervated from the superior branch of the oculomotor nerve. When in its primary position, the muscle’s primary function is elevation, but it is also responsible for adduction and intorsion.
What is the action of the superior rectus?
superior rectus helps to elevate the eyeball.




2 Comments