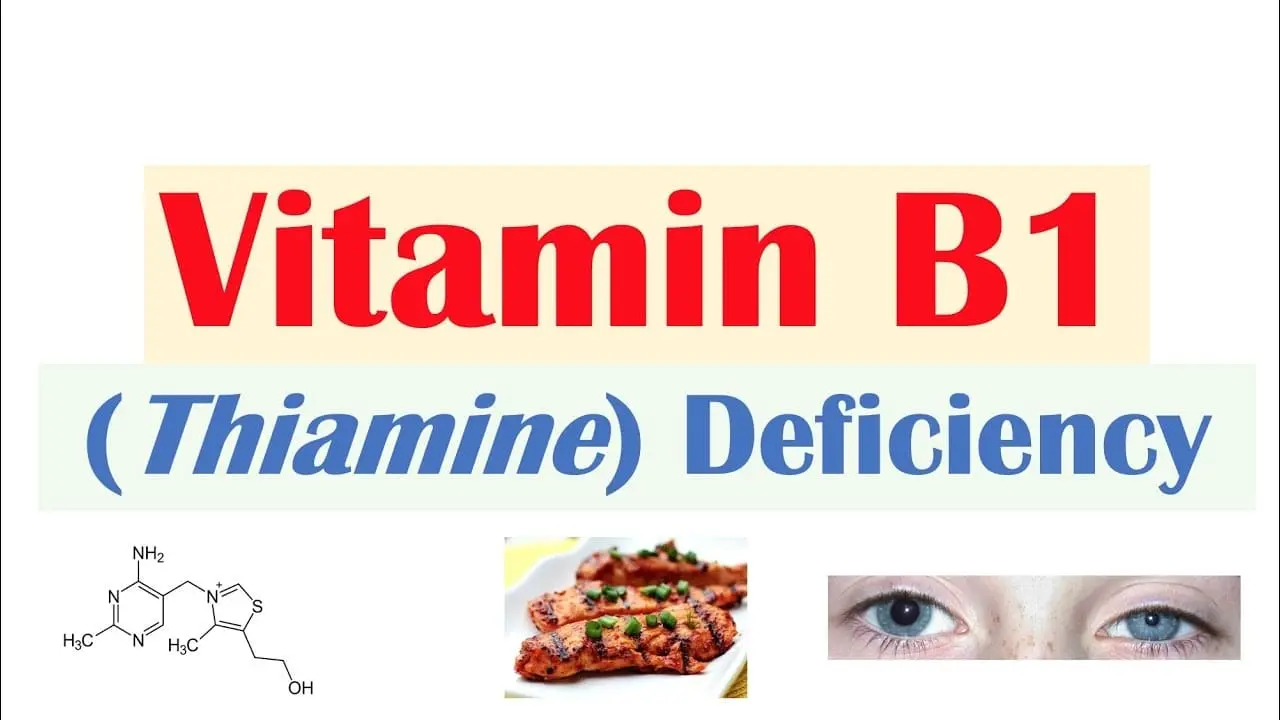
Thiamine (Vitamin B1) Deficiency
What is a Thiamine Deficiency?
Low levels of thiamine (Vitamin B1) are a medical condition known as thiamine deficiency. Beriberi is the name for a severe and long-lasting type. In adults, moist and dry beriberi are the two primary varieties.
Because wet beriberi affects the circulatory system, symptoms such as limb edema, dyspnea, and an accelerated heart rate might occur.
Due to its effects on the neurological system, dry beriberi can cause discomfort, disorientation, numbness in the hands and feet, and difficulty moving the legs. There may also be a variant that includes constipation and appetite reduction.
Acute beriberi is a different kind that primarily affects infants and is characterized by changes in heart rate, enlargement of the heart, vomiting, lactic acidosis, and appetite loss.
A diet heavy in white rice, drunkenness, dialysis, persistent diarrhea, and high diuretic dosages are risk factors. Rarely, it could be brought on by a hereditary disorder that makes it difficult for the body to absorb thiamine from meals.
Two types of dry beriberi are Wernicke encephalopathy and Korsakoff syndrome. The symptoms, high blood lactate, low thiamine levels in the urine, and improvement with thiamine supplementation are used to make the diagnosis.
Thiamine supplements, either orally or by injection, are the treatment method. Symptoms usually go away in a few weeks with therapy.
Food fortification is one way to avoid the illness at the community level. In the US, thiamine deficiency is uncommon. It’s still rather frequent in Africa’s sub-Saharan regions. There have been outbreaks in camps for refugees.
Asia has been reporting cases of thiamine deficiency for thousands of years; when rice processing intensified in the late 1800s, the condition became increasingly widespread.
Signs and Symptoms of Thiamine Deficiency
Weight loss, mental instability, decreased sensory awareness, limb weakness and discomfort, and erratic heartbeats are all signs of beriberi.
Body tissue swelling, or edema, occurs often. It could cause the blood’s levels of pyruvic and lactic acids to rise. Advanced forms of the condition may result in mortality from high-output heart failure.
Wernicke’s encephalopathy, a predominantly neurological disorder associated with thiamine deficiency, may present with concomitant symptoms. There are four categories for Beriberi. The fourth condition, gastrointestinal beriberi, was identified in 2004. The first three are historical:
- The peripheral nerve system is specifically affected by dry beriberi.
- Particularly affecting the cardiovascular system and other body systems is wet beriberi.
- Infants born to undernourished mothers are susceptible to infantile beriberi.
- The digestive system as well as other body systems are impacted by gastrointestinal beriberi.
Dry Beriberi
Because dry beriberi damages peripheral nerves, it results in wasting and partial paralysis. Another name for it is endemic neuritis. It is distinguished by:
- Having trouble walking
- Numerical tingling or lack of feeling in the hands and feet
- Diminished tendon reflexes
- loss of lower limb muscular function or paralysis
- Speech problems and mental disorientation
- Anguish
- Uncontrollably moving eyes (nystagmus).
- throwing up
A pronounced sensory ataxia, or loss of balance and coordination owing to loss of proprioceptive inputs from the periphery and loss of position sensation, might be the result of selective impairment of the vast proprioceptive sensory fibers without motor impairment.
Brain Disease
Dry beriberi manifests itself as Wernicke’s encephalopathy (WE), Korsakoff syndrome (also known as alcohol amnestic illness), and Wernicke–Korsakoff syndrome.
The most common sign of thiamine deficiency in Western society is Wernicke’s encephalopathy, though it can also happen to patients who are malnourished from other conditions like gastrointestinal disorders.
HIV/AIDS patients, improper parenteral glucose administration, or hyperalimentation without sufficient B-vitamin supplementation.
This is a remarkable neuropsychiatric condition distinguished by severely disturbed mental function, aberrant posture and gait, and paralysis of ocular movements.
Patients who are first diagnosed with WE are generally thought to experience a decline in brain function when they develop Korsakoff syndrome.
This amnestic-confabulatory condition is typified by diminished spontaneity and initiative, mental function impairment, and retrograde and anterograde amnesia.
Alcoholics may be deficient in thiamine due to.
- Inadequate nutritional intake: People who drink a lot of alcohol typically consume less thiamine than is advised.
- Reduced absorption of thiamine from the gastrointestinal tract: Acute alcohol exposure disrupts the active transport of thiamine into enterocytes.
- Hepatic fibrosis or steatosis reduces the amount of thiamine stored in the liver.
- Reduced thiamine utilization: Prolonged alcohol use also causes a magnesium deficiency, which is necessary for thiamine to attach to thiamine-consuming enzymes inside the cell. The thiamine shortage will worsen as a result of poor usage of the thiamine that does make it into the cells.
- In the gastrointestinal tract, ethanol itself hinders thiamine transport and prevents thiamine from being phosphorylated into its cofactor form (ThDP).
Some thiamine deficiency-related deficits, such as impaired brain function, are corrected with increased diet and cessation of alcohol usage; however, in more severe cases, Wernicke-Korsakoff syndrome results in permanent damage.
Wet Beriberi
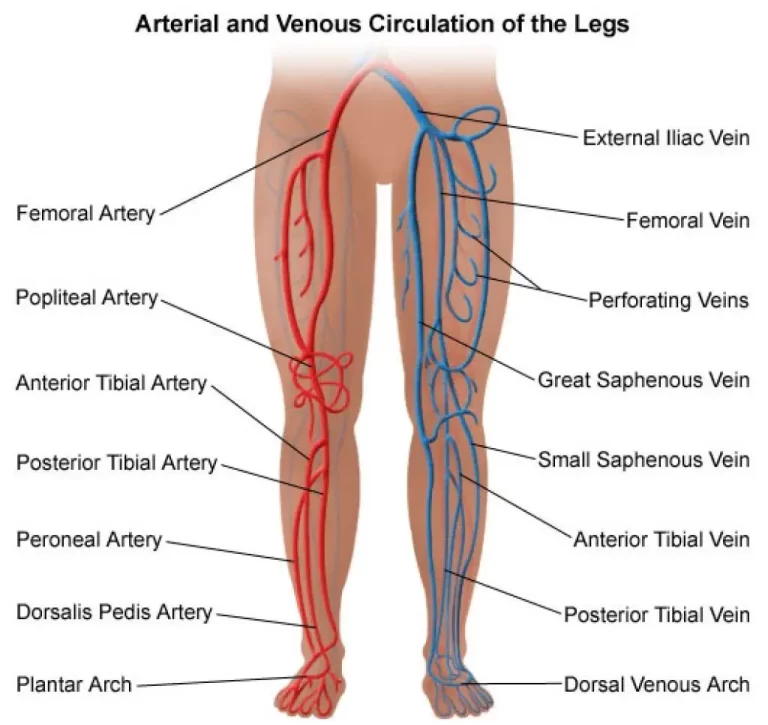
The circulatory system and heart are impacted by wet beriberi. Because it weakens capillary walls and induces heart failure, which makes the peripheral tissues edematous, it can occasionally be deadly.
What distinguishes wet beriberi?
- Elevated heart rate
- Vasodilation results in a reduction of systemic vascular resistance, and heart failure with high output
- Higher than normal jugular vein pressure
- Dyspnea, or difficulty breathing when exerted
- Paroxysmal dyspnea throughout the night
- Generalized or peripheral edema, or lower leg swelling 8edema (all over body swelling)
- dilated cardiomyopathy
Gastrointestinal Beriberi
Abdominal discomfort is a result of gastrointestinal beriberi. It is distinguished by:
- Nausea
- Vomiting
- Lactic acidosis
Infants
Infantile beriberi typically affects children whose moms consume insufficient amounts of thiamine between the ages of two and six months.
It might show up as dry or wet beriberi. When heart failure strikes a newborn in the acute form, they first feel dyspnea and cyanosis.
The following signs of infantile beriberi might be mentioned.
- Nerve paralysis causes hoarseness, in which a kid moves to moan but either produces no sound or just weak groans.
- Loss of weight, becoming slender, and eventually developing marasmic
- Vomiting
- Diarrhea
- Pale skin
- Edema
- Pale skin
- A bad attitude
- Changes in the cardiovascular system, particularly fast heart rate, or tachycardia
- Occasional convulsions seen in the last stages
Cause of Thiamine Deficiency
Eating a diet high in calories from polished rice (common in Asia) or cassava root (common in sub-Saharan Africa) and low in vegetables or animal products that contain thiamine is often the cause of beriberi.
It can also be brought on by deficiencies other than insufficient intake, such as hereditary deficits, alcoholism, dialysis, illnesses, or surgeries involving the digestive system.
These factors all primarily impact the central nervous system, which in turn triggers the onset of Wernicke’s encephalopathy. One of the most common neurological or neuropsychiatric conditions is Wernicke’s illness.
In around 2% of general cases in the autopsy series, Wernicke lesion characteristics are noted. Approximately 85% of cases, despite just 19% being asymptomatic, have not been diagnosed, according to a medical record study. Just 58% of children received a diagnosis.
Neurological injury was seen in alcohol drinkers at autopsy series rates of at least 12.5%. Wernicke’s illness accounts for 17% of all disease deaths, or 3.4/1000, or over 25 million of its contemporaries.
Given that early stages of the disease may have dysfunctions before the development of visible lesions during necropsy, the number of patients with Wernicke’s disease may be considerably greater.
Furthermore, countless numbers of individuals may suffer from disorders that develop from prenatal injury.
Genetics
Thiamine transport genetic disorders are uncommon yet dangerous. Mutations in the high-affinity thiamine transporter gene SLC19A2 produce thiamine-responsive megaloblastic anemia syndrome (TRMA), an autosomal recessive condition associated with diabetes mellitus and sensorineural hearing loss.
There may be redundancy in the thiamine transport system since TRMA patients do not exhibit symptoms of a systemic thiamine deficit.
As a result, SLC19A3, a second high-affinity thiamine transporter, was found. Subacute necrotizing encephalomyelopathy, often known as Leigh disease, is a hereditary condition that usually affects newborns in their early years and is always deadly.
Given the pathological similarities between Leigh’s illness and WE, a thiamine metabolism problem was thought to be the culprit.
An anomaly in the pyruvate dehydrogenase complex’s activity has been one of the most reliable results. Biotin-thiamine-responsive basal ganglia illness, which is treated with pharmaceutical dosages of thiamine and biotin, another B vitamin, has been associated with mutations in the SLC19A3 gene.
Subacute necrotizing encephalomyelopathy, opsoclonus myoclonus syndrome (a paraneoplastic illness), and Nigerian seasonal ataxia (also known as African seasonal ataxia) are other conditions in which thiamine may have a role.
Furthermore, a number of hereditary illnesses involving ThDP-dependent enzymes have been documented; these disorders may benefit from thiamine therapy.
Pathophysiology
The human body quickly runs out of thiamine, especially when intake is insufficient to meet metabolic needs. Its half-life is 17 days.
Thiamine pyrophosphate (TPP), a thiamine derivative, is a cofactor in the citric acid cycle and serves as a link between the citric acid cycle and the breakdown of carbohydrates.
The creation of several molecules, including the neurotransmitters glutamic acid and GABA, is inhibited by the disruption of the citric acid cycle, a major metabolic route involved in the control of carbohydrate, lipid, and amino acid metabolism, caused by thiamine deficiency. Furthermore, thiamine could possibly have a direct role in.
Diagnosis
Measuring the activity of the transketolase enzyme in erythrocytes is a positive diagnostic test for thiamine deficiency (Erythrocyte transketolase activation assay).
As an alternative, thiamine can be directly detected in whole blood, tissues, foods, animal feed, and pharmaceutical preparations after being separated by a thiochrome test and converted to fluorescent thiochrome derivatives.
Liquid chromatography with high performance (HPLC). Alternative methods for measuring and tracking thiamine levels in materials have arisen, including capillary electrophoresis (CE) techniques and in-capillary enzyme reaction methods. In EDTA blood, the typical thiamine content ranges from 20 to 100 µg/L.
Treatment of Thiamine Deficiency
Thiamine alone can be used to treat beriberi in many cases. When thiamine is administered intravenously (and then orally), recovery happens quickly and dramatically, usually in less than a day. Peripheral neuropathy may not improve for several months after starting thiamine therapy.
Epidemiology
Even in this century, dietary diseases like beriberi are a common occurrence in correctional facilities. A beriberi epidemic happened at a Taiwanese correctional facility in 1999.
The custom of washing rice before boiling removed a nutrient coating that had been added after manufacturing, which contributed to the high incidence of disease and mortality from beriberi in crowded Haitian jails in 2007. (enhanced white rice).
Among a group of convicts in the Ivory Coast receiving harsh sentences, 64% had beriberi. Prior to starting therapy, the inmates had neurological symptoms (tingling: 41%), cardiovascular symptoms (dyspnea: 42%), thoracic discomfort (35%), and lower leg edemas (51%).
Healing occurred at a rate of almost 97% after therapy. Extremely stressed populations may be more susceptible to beriberi. People who have been uprooted, like war refugees, are more vulnerable to micronutrient deficiencies like beriberi.
Beriberi can also result from severe nutritional deficiency brought on by famine, however, symptoms may be missed in a clinical examination or confused with other famine-related issues. Rarely, a severe weight-loss diet may cause beriberi or the following famine-like syndrome.
The basic diet of high carbohydrates and extended intervals between shoring put workers aboard Chinese squid ships in danger for beriberi. 15 personnel on 14 ships have passed away from beriberi symptoms between 2013 and 2021.
History
The first documented accounts of thiamine insufficiency date back to ancient Chinese medicine. One of the first is found in Ge Hong’s book Zhou Hou Bei Ji Fang, which was written in the third century and contains emergency formulas to have up your sleeve.
The ailment was referred to by Hong as jiao qi, which means “foot qi” in Chinese. He listed the symptoms as including numbness, weakness, and edema in the feet.
In addition, he stated that consuming specific foods, such as fermented soybeans in wine, may treat the sickness, even though it could be fatal.
BetterEarly accounts of “foot qi” have been documented by Sun Simiao (581–682) in his book Bei Ji Qian Jin Yao Fang (Essential Emergency Formulas Worth a Thousand in Gold) and by Chao Yuanfang (550–630) in his book Zhu bing yuan hou lun.
Takaki Kanehiro, a Japanese physician in the Imperial Japanese Navy with training in Britain, examined beriberi in the late 1800s.In the Japanese navy, beriberi was a major concern.
Between 1878 and 1881, sailors became ill an average of four times a year, with 35% of those instances being related to beriberi.
Takaki discovered in 1883 that cadets on a training trip from Japan to Hawaii, via New Zealand and South America, had an extremely high frequency of beriberi.
On a ship carrying 376 men, the journey, which lasted more than nine months, resulted in 169 cases of illness and 25 fatalities. With the backing Using the Japanese Navy, he carried out an experiment in which.
A different ship was sent on the same journey but its crew was fed a meal consisting of beans, rice, barley, and fish. This crew had just 14 instances of beriberi at the conclusion of the expedition, and no one had died.
Takaki and the Japanese Navy were persuaded that nutrition was the root reason for this. Takaki noted in 1884 that beriberi was more common in low-ranking crew members who received free rice often and ate nothing other than that, but not in crews of Western warships or Japanese commanders who had a more diverse diet.
Dutch physician and pathologist Christiaan Eijkman proved in 1897 that a bad diet is the cause of beriberi and that preventing the disease in hens could be achieved by giving them unpolished rice rather than the polished kind.
The next year, Sir Frederick Hopkins proposed that certain diets had “accessory factors” in addition to proteins, carbs, fats, and salt, which were essential for human bodily processes. body.
The diagnosis of beriberi as a deficiency condition was made accurately in 1901 by Gerrit Grijns, a Dutch physician who worked as Christiaan Eijkman’s assistant in the Netherlands. Later, in 1910–1913,
Edward Bright Vedder proved that beriberi could be treated using an extract of rice bran.[Reference required] For their findings, Eijkman and Hopkins were given the 1929 Nobel Prize in Physiology or Medicine.
Etymology
The phrase “beriberi” has dubious origins, even though the Oxford English Dictionary states that it originates from a Sinhalese phrase that means “weak, weak” or “I cannot, I cannot,” with the word being repeated for emphasis.
Its origins in Hindi, Arabic, and a few other languages have also been proposed. Its various meanings include “sheep,” “weakness,” and “sailor.”
Heinrich Botho Scheube was one of the people who enumerated these proposed origins. According to Edward Vedder, “It is impossible to definitely trace the origin of the word beriberi” (Beriberi, 1913).
Diogo do Couto first used the word “berbere” in writing in 1568 when he discussed the shortage in India. The Japanese term for thiamine deficiency, kakke (脚気), derives from the pronunciation of “jiao qi” in that language.
Beriberi is referred to in Chinese medicine by the ancient term “jiao qi”. It is believed that “Kakke” first appeared in the Japanese language during the sixth and ninth centuries.
Other Animals
Poultry
Vitamin shortages do not arise with commercial diets for chickens since the majority of feedstuffs used in their diets include sufficient amounts of vitamins to suit the needs of this species. In the 1960s, at least, this was the consensus.
Three weeks into being fed an inadequate diet, mature hens begin to exhibit symptoms. It can show up in young chicks before they are two weeks old. In young girls, the onset is abrupt, accompanied by anorexia and a shaky walk.
Later on, there is evidence of locomotion, including what seems to be toe flexor paralysis. The afflicted animal assumes the so-called “stargazing” posture, which involves sitting on its hocks and reversing its head into an opisthotonos-like position. The vitamin is administered, and the response happens within a few hours afterward.
Ruminants
The most prevalent thiamine deficiency condition in young ruminant and nonruminant animals is polioencephalomalacia (PEM).
PEM symptoms include circular motions, stargazing or opisthotonus (head dragged back over the neck), trembling in the muscles, and copious but temporary diarrhea.
The most frequent reason is high-carbohydrate diets, which promote the development of bacteria that produce thiaminase.
Other potential causes include dietary thiaminase consumption (found in bracken fern, for example) or excessive sulfur intake, which inhibits the absorption of thiamine.
An infection with Bacillus aneurinolyticus or Clostridium sporogenes is another cause of PEM. The afflicted animal may experience an acute thiamine deficit as a result of the thiaminases produced by these bacteria.
Snakes
Thiamine insufficiency can occur in snakes whose diet consists mostly of feeder minnows and goldfish. Since goldfish are the only fish that can break down thiamine, thiaminase, an enzyme found in goldfish, is sometimes an issue when raising garter and ribbon snakes in captivity.
Wild Birds and Fish
A paralytic sickness that has been afflicting wild birds in the Baltic Sea region since 1982 has been linked to thiamine deficiency.
This illness is characterized by difficulties folding the wings to the side of the body while at rest, loss of voice and flight ability, and finally paralysis of the legs and wings leading to death. It mostly affects birds weighing between 0.5 and 1 kg.
Including common starlings (Sturnus vulgaris), European herring gulls (Larus argentatus), and common eiders (Somateria mollissima).
The counties of Blekinge and Skåne have witnessed the devastating loss of several bird species during the early 2000s, most notably the European herring gull. Other classes of animals appear to be impacted as of late.
There have been reports of abnormally high death rates for animals like the Eurasian elk (Alces alces) and high salmon (Salmo salar) mortality in the Mörrumsån River. Where analysis is done, the common denominator is thiamine deficiency.
The issue was sufficiently concerning that the County Administrative Board of Blekinge urged the Swedish government to organize a more thorough investigation in April 2012.
FAQ
What are the symptoms of low thiamine?
The early signs of thiamin insufficiency are not very clear. These include exhaustion, agitation, impaired memory, appetite loss, insomnia, tummy aches, and weight loss. Beriberi, a severe thiamin deficit marked by problems in the brain, heart, and nerves, may eventually occur.
Is thiamine B1 or b12?
Vitamin B1 also referred to as thiamin, aids in the body’s energy release and digestion of meals. maintain the health of the neurological system.
What is the best indicator of thiamine deficiency?
The most accurate way to diagnose thiamine deficiency is to use a thiamine loading test in combination with whole blood or erythrocyte transketolase activity preloading and postloading. A definite indicator of deficiency is an increase in enzyme activity of greater than 15%.
How much thiamine to reverse deficiency?
For severe deficiency, 25–30 mg intravenously in babies and 50–100 mg in adults is the suggested course of therapy. After that, 10 mg daily is provided intramuscularly for about a week, and for at least six weeks, 3–5 mg of thiamin is taken orally.
What is the main cause of thiamine deficiency?
People with alcohol use disorders and those whose diet mostly consists of highly processed carbohydrates or white rice are more likely to suffer from thiamin deficiency, which can lead to beriberi and other issues. These nations also have high rates of food instability.
How do you treat thiamine deficiency?
The patient should switch to 10 mg/day oral thiamine until the anticipated recovery is achieved. Until symptoms subside or improvement reaches a plateau, 200 mg intravenous (IV) or oral (PO) thiamine should be administered three times a day.
Is thiamine and folic acid the same?
The majority of these vitamins, which go by different names often, are presumably more well-known. For instance, people often associate vitamin B1 with thiamine, vitamin B2 with riboflavin, vitamin B3 with niacin, and vitamin B9 with folic acid or folate.