Tibia Bone
Introduction
The second-longest bone in your body is the tibia bone. It has a significant impact on how you walk, stand, and maintain your balance.
Usually, only severe injuries like auto accidents cause the tibia to break.
However, osteoporosis weakens bones, increasing the risk of fractures that you may not even be aware of.
In vertebrates, the tibia, sometimes referred to as the shinbone or shankbone, is the larger, stronger, more anterior bone that connects the knee to the ankle.
The tibia is located nearer the middle plane and on the medial side of the leg, adjacent to the fibula. The leg’s interosseous membrane connects the tibia to the fibula, creating a syndesmosis type of extremely little-moving fibrous joint.
The flute tibia inspired the tibia’s name. After the femur, it is the second-largest bone in the human body.
Given that they bear the weight of the entire body, the leg bones are the strongest long bones.
The larger and inner of the two lower leg bones in vertebrates is called the tibia; the other is called the fibula. In humans, the tibia forms the inner ankle protuberance below and the lower portion of the knee joint above.
The upper portion comprises two prominences, or condyles, with relatively flat tops that articulate with the condyles of the femur, or thighbone, above.
The knee joint is completed by the patella, or kneecap, ligament’s attachment to the front tibial tuberosity.
The place where the fibula articulates is part of the greater lateral condyle. The tibia’s cross-sectional shape is roughly triangular, and the strength of the muscles that are linked to it affects how it is marked.
Anatomy
The tibia’s shaft has three surfaces and three edges, making it triangular in cross-section.
The lateral, medial (anterior), and posterior are the three surfaces, and the three borders are the anterior, medial, and interosseous.
The lateral and posterior surfaces are divided by the interosseous border, the medial and posterior surfaces by the anterior border, and the medial and posterior surfaces by the medial border.
Where is the tibia situated?
The larger of the two bones inside your lower leg is called the tibia. The fibula, or calf bone, is the other. The tibia extends to your ankle from slightly below your knee. Compared to the fibula, it is more proximal to the inside of your body.
Tibia vs Fibula
| Measures | Tibia | Fibula |
| Bone type | The large bone, which occurs in the lower front portion of the leg | the outer and usually smaller of the bones between the knee and the ankle |
| AKA | Shinbone | Calf bone |
| Size | Larger | Smaller |
| Width | Wider | Thinner |
| Appear side in body | Occurs anteriorly | Occurs laterally |
| Articulation | Connects the knee to the ankle joint | The head of the bone occurs below the ankle joint and lower extremity of the bone forms the lower part of the ankle joint |
| Function | Bears the body weight | Stabilizes the ankle joint |
Your lower leg is made up of two bones: the tibia and fibula.
The tibia is lengthier and consists of your ankle at the lower (distal) end and a portion of your knee at the top (proximal). The lateral (near to the exterior of the body) fibula is compared to the tibia.
Because the tibia bears weight, it sustains your body as you walk and stand.
Overview
What is a tibia bone?
Your shinbone is called the tibia. Being the second-most long bone in your body, it plays a crucial role in your capacity to move and stand. Numerous significant muscles, tendons, nerves, and ligaments are also supported by your tibia.
Because tibiae are so sturdy, breaking them usually requires a major trauma, such as a vehicle accident or fall. Should you suffer a fracture, you probably require both physical therapy that helps you to restore your strength and mobility and surgery to fix your broken bone.
Osteoporosis can affect your tibia just like it can affect other bones.
The tibia is one of the two bones which make up the leg. Compared to the fibula, it is much bigger and stronger than the weight-bearing bone.
Together with the femur, the tibia creates the knee joint proximally, and with the fibula and talus, it makes the ankle joint distally.
The interosseous membrane connects the tibia to the fibula as it travels medially from close to the knee joint to the ankle joint.
The inferior part of the knee joint is formed by the medial and lateral condyles, which are located on the proximal part of the tibia.
The anterior collateral ligament, posterior collateral ligament, and menisci attach to the intercondylar region, which is located between the two condyles.
The back surface connects the posterior compartment of the leg, the lateral surface connects the anterior compartment, and the medial surface is primarily subcutaneous.
Structure
The tibia is the second biggest bone in the human body, after the femur.
Like in other vertebrates, the tibia is a component of the joints of the knee and ankle and is one of two bones in the lower leg, with the other being the fibula.
Three locations—one in the shaft and one in each extremity—are where the ossification, or creation, of the bone, begins.
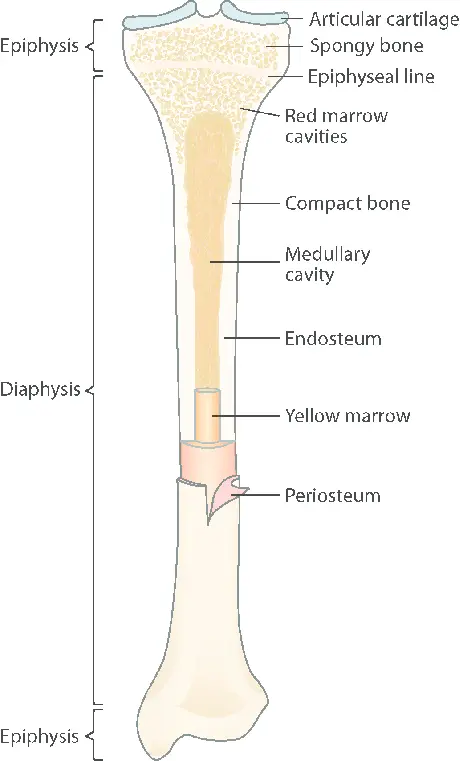
The tibia is divided into two epiphyses and a diaphysis, making it a lengthy bone. The middle part of the tibia, referred to as the shaft or body, is called the diaphysis.
The two rounded ends of the bone, the lower nearest to the foot and the upper closest to the thigh are called epiphyses.
A proximal end of the Tibia
Condyles of Tibia
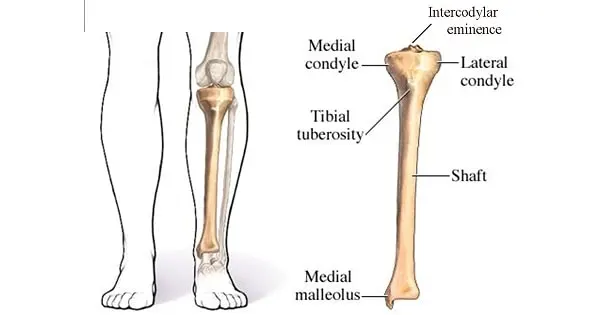
With a medial and lateral condyle that are both flattened in the horizontal plane, the proximal or upper part of the tibia is enlarged in the transverse plane.
Out of the two, the medial condyle is bigger and has superior support over the shaft.
The tibiofemoral joint, which bears weight in the knee joint, is formed by the articulation of the condyles’ top surfaces with the femur.
The intercondylar region, where the menisci and cruciate ligaments attach, divides the medial and lateral condyles.
The intercondylar eminence is formed in this instance by the medial & lateral intercondylar tubercle. The intercondylar region, in conjunction with the medial and lateral condyles, creates the tibial plateau. This region is anchored to the lower end of the femur and articulates with it.
The anterior and posterior halves of the intercondylar region are separated by the intercondylar eminence.
Numerous tiny apertures for nutritional arteries are perforated in the anterolateral region located in the anterior intercondylar area.
Both condyles’ articular surfaces are concave, especially in the center. The menisci are in touch with the flatter outer edges.
Its oval-shaped superior surface extends laterally onto the side of the medial intercondylar tubercle in the medial condyle.
The medial border of the superior surface of the lateral condyles extends onto the side of the lateral intercondylar tubercle, giving it a more circular shape.
Facets
There are two smooth articular facets on the superior articular surface.
The oval-shaped medial facet is somewhat concave from front to rear and from side to side.
The lateral, which is almost round, is concave from side to side but slightly convex from the front to the back, particularly in the posterior region where it extends briefly onto the posterior surface.
These facets’ center sections articulate with the femur’s condyles, while their periphery supports the knee joint’s menisci, which in this case act as an intermediary between the two bones.
Lateral condyle
the tibia’s lateral proximal portion where it articulates with the femur
Middle condyle
The tibia’s medial proximal portion where it articulates with the femur
Lateral tibial plateau
The lateral condyle’s superior articular surface
Medial tibial plateau
The medial condyle’s superior articular surface
Intercondylar area
- Anterior area
situated between the lateral and medial condyles anteriorly. the anterior cruciate ligament’s attachment site.
- Posterior area
situated between the lateral and medial condyles posteriorly. the posterior cruciate ligament attachment site.
- Intercondyloid eminence
The intercondyloid eminence, or spine of the tibia, is located between the articular facets in the intercondylar area, but closer to the posterior than the anterior aspect of the bone.
which comprises a medial and lateral tubercle, and is situated in between the articular facets. The menisci and cruciate ligaments attach to the depression behind the intercondyloid eminence.
It is topped on either side by a prominent tubercle, on which the articular facets are prolonged.
Rough depressions for the attachment of the menisci and the anterior and posterior cruciate ligaments are located in front and behind the intercondyloid eminence.
Surfaces
- The anterior surfaces
The condyles’ anterior surfaces blend together to form a sizable, somewhat leveled region that is triangular in shape, broad above, and punctured by large vascular foramina; it is narrow below and ends in the tibia’s tuberosity, a large oblong elevation that serves as the patellar ligament’s attachment point.
A bursa sits between the ligament’s deep surface and the area of the bone directly above the tuberosity.
- Posterior surfaces
A portion of the posterior cruciate ligament at the knee joint attaches to the posterior intercondyloid fossa, a shallow depression that divides the condyles from one another posteriorly.
The tendon of the semimembranosus inserts into a deep transverse groove that is seen posteriorly on the medial condyle.
- Medial surface
The medial collateral ligament attaches to its conspicuous, rough, and convex medial surface.
A nearly round, flat articular facet oriented downward, backward, & lateralward is presented posteriorly by the lateral condyle in preparation for articulation with the fibula head.
- Lateral surface
Its lateral surface is rough, convex, and noticeable in front.
On it is an elevation for the iliotibial band to connect, level with the top border of the tuberosity and at the intersection of its anterior and lateral surfaces.
A portion of the extensor digitorum longus originates just below, and a slip from the biceps femoris tendon is inserted.
Shaft
The triangular cross-section of the tibia’s body produces three borders: the anterior, medial, lateral, or interosseous, borders.
The medial, lateral, and posterior surfaces are formed by these three borders. The fibia, which is frequently mistaken for the fibula, is the forward, flat portion of the tibia.
Borders
The anterior border
The most noticeable of the three is the anterior crest or border, which begins at the tuberosity above and terminates at the anterior boundary of the medial malleolus below.
It provides attachment to the leg’s deep fascia and is curved and prominent in the top two-thirds of its length, smooth and rounded below.
The medial border
The medial border is more noticeable in the middle and is smooth and rounded above and below. It starts at the rear of the medial condyle and finishes at the posterior edge of the medial malleolus.
Its upper portion attaches to the popliteus muscle’s fibers and extends to the knee joint’s tibial collateral ligament by about 5 centimeters.
The lateral border
The thin and prominent interosseous crest, also known as the lateral border, provides attachment for the interosseous membrane.
It starts above, in front of the fibular articular facet, and splits below to form the boundaries of a triangular rough surface where the interosseous ligament that connects the tibia and fibula is attached.
Surfaces
The medial surface
The medial surface is smooth, convex, and wider above than below.
The aponeurosis from the sartorius tendon, as well as the tendons of the Gracilis and Semitendinosus, cover its upper third, which is directed forward and medialward.
These tendons are inserted almost as far forward as the anterior crest, leaving the remaining portion of the surface subcutaneous.
The lateral surface
The lateral surface is narrower than the medial; the tendons of the Tibialis anterior, Extensor hallucis longus, and Extensor digitorum longus, which are arranged from the medial side, cover its lower third, which is smooth, convex, and curve gradually forward to the anterior aspect of the bone.
The upper two-thirds of the lateral surface presents a shallow groove for the origin of the Tibialis anterior.
The posterior surface
The popliteal line, which ascends obliquely from the rear of the fibula’s articular facet to the medial border at the intersection of its upper and middle thirds, is a prominent ridge on the posterior surface.
It marks the lower limit of the Popliteus’s insertion, serves as the site of the fascia covering this muscle, and provides origin to a portion of the Soleus, Flexor digitorum longus, and Tibialis posterior.
The Popliteus inserts into the triangular region above this line. A vertical ridge splits the middle third of the posterior surface into two sections.
The ridge starts at the popliteal line and is prominent above but less so below.
The Flexor digitorum longus originates from the medial, broader portion of the ridge, while the Tibialis posterior is partially located in the narrower, lateral portion.
Flexor digitorum longus, Flexor hallucis longus, and Tibialis posterior cover the smooth remaining portion of the posterior side.
The big, obliquely downward-directed nutritive foramen is located directly below the popliteal line.
The distal end of Tibia
The tibia’s distal end is considerably shorter than its proximal end and has five surfaces.
The medial malleolus, a robust pyramidal projection, extends downward on the distal side of the tibia.
The ankle joint is formed by the tibia, fibula, and talus in the lower extremities.
Surfaces
The Inferior surface
For articulation with the talus, the inferior articular surface is smooth and quadrilateral in shape.
It is wider in front than behind, concave from before backward, and crosses two depressions with a small elevation between them. That and the one on the medial malleolus are continuous.
The anterior surface
The tendons of the extensor muscles cover the smooth, rounded anterior surface of the lower extremity, which has a rough transverse depression at its bottom edge where the articular capsule of the ankle joint is attached.
The posterior surface
A shallow groove that runs obliquely downward and medially over the posterior surface allows the tendon of the Flexor hallucis longus to pass through. This groove is connected with one on the posterior side of the talus.
The lateral surface
The lateral side has a triangular rough depression where the inferior interosseous ligament attaches to connect it to the fibula; the lower portion of this depression articulates with the fibula and is smooth, coated with cartilage in its fresh form.
The anterior and posterior colliculi, which form the surface’s two conspicuous boundaries and are continuous with the interosseous crest above, provide attachment points for the lateral malleolus’ anterior and posterior ligaments.
Embryology
Three ossification centers are present in the tibia: one for each epiphysis and diaphysis.
About the seventh week of pregnancy is when it starts in the shaft.
Beginning at birth, the proximal ossification center closes at age 16 for females and age 18 for males.
Beginning at birth, the distal ossification center closes at age 15 for females and age 17 for males.
Blood Supply and Lymphatic System
The tibia receives its blood supply from the periosteal vessels and the nutritional artery.
The nutritional artery penetrates the bone posteriorly distal to the soleal line, branching off from the posterior tibial artery.
The anterior tibial artery is the source of the periosteal vessels.
Nerves
All of the principal nerves that supply neighboring compartments are branches that supply the tibia.
The tibial nerve provides branches that feed the tibia’s posterior side in the leg’s posterior compartment, while the deep fibular nerve provides branches that supply the tibia’s anterior aspect in the leg’s anterior compartment.
Muscle attachment
Insertion of Muscles on the tibia
- The lateral tubercle of the tibia, also referred to as the Gerdy tubercle, is where the tendon fasciae latae inserts.
- The tibial tuberosity is where the quadriceps femoris inserts anteriorly.
- On the pes anserinus, the gracilis, semitendinosus, and arthritis insert anteromedially.
- The medial condyle is where the horizontal head of the semimembranosus muscle inserts.
- On the posterior tibia’s soleal line, the popliteus inserts.
Origin of Muscles from the Tibia
- The upper two-thirds of the lateral tibia are the source of the tibialis anterior.
- The lateral condyle of the tibia is the site of origin of the extensor digitorum longus.
- On the sole line, the posterior portion of the tibia is the origin of the soleus and flexor digitorum longus.
Joints
The knee, ankle, superior and inferior tibiofibular joints, and the tibia are the four joints that make up the body.
Often known as the tibiofemoral bones of the knee joint, the tibia and femur form one of the two articulations of the knee.
It is the knee joint’s weight-bearing component.
The articulations between the tibia and fibula that permit relatively little movement are called tibiofibular joints.
The little plane joint is known as the proximal tibiofibular joint.
The head of the fibula and the underside of the lateral tibial condyle form the joint.
The anterior and posterior ligaments of the fibula head support the joint capsule.
The proximal end of the talus is connected to the distal ends of both the fibula and tibia in the lower limb by the synovial hinge joint that makes up the talocrural joint of the ankle.
More weight is placed on the articulation in the tibia and talus than on the smaller fibula and talus.
Development
A primary center for each diaphysis (shaft) and a secondary center for each of the epiphysis (extremity) make up the ossified tibia.
Around the seventh week of fetal development, ossification starts in the center of the body and progressively moves outward toward the extremities.
The tuberosity is formed by a thin tongue-shaped process in front of the flattened upper epiphysis center, which originates before or shortly after birth at approximately 34 weeks gestation. The lower epiphysis center appears in the second year of life.
Around the age of eighteen, the lower epiphysis fuses with the tibial shaft, and around the age of twenty, the upper epiphysis fuses.
Strength
Walking can exert an axial stress on the tibia of up to 4.7 bodyweight, according to models.
In the late stance phase, its bending moment in the sagittal plane can reach up to 71.6 bodyweight times millimeters.
Clinical Anatomy
Fracture in tibia
The medical word for shattering a bone is a bone fracture.
Because the tibia is incredibly sturdy, severe trauma falls, and auto accidents are typically the only things that can break one.
Among the signs of a fracture are:
- Pain.
- Swelling.
- Tenderness.
- Unable to move your leg as freely as you normally can.
- Any Discolouration or bruises.
- a lump or malformation that is unusual for your body.
If you believe you may have a fracture or have suffered trauma, get to the emergency department as soon as possible.
The osteoporosis
Fractures that happen suddenly and unexpectedly are more likely to occur because osteoporosis weakens bones.
Many people don’t become aware that they have osteoporosis until the moment it breaks a bone. Usually, there aren’t any overt signs.
Individuals who are born with a female gender assignment, women, and adults over 50 are more likely to develop osteoporosis.
See your physician about scheduling a bone density test, which can identify osteoporosis early on and prevent fractures.
The Osgood-Schlatter illness
Tendons pulling on the top of the shinbone can produce pain in the upper shin and knee in people with Osgood-Schlatter disease.
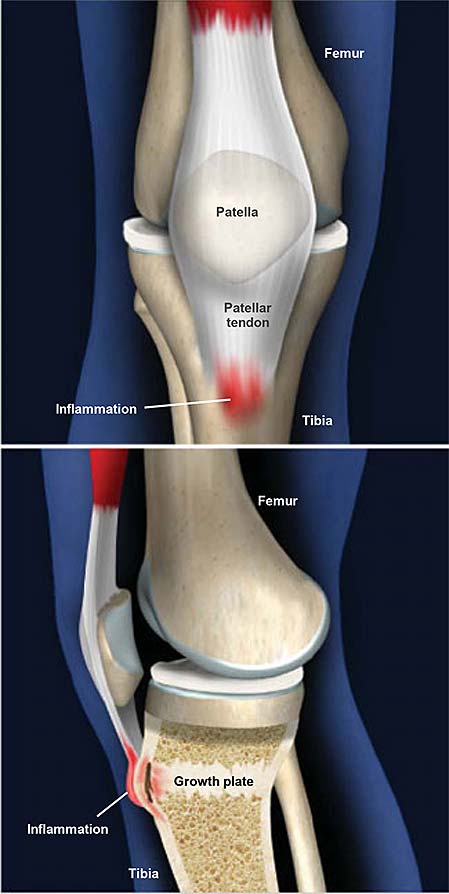
It typically impacts growing children and teenagers. It is also referred to as a jumper’s knee.
Among the symptoms are:
- Growing.
- Sensitivity.
- Soreness directly below the knee.
Should your child develop new knee pain, have a conversation with your provider.
Paget’s disease of the bone
Osteitis deformans, often known as Paget’s disease of the bone, is a long-term bone condition. Your impacted bones continually deteriorate and grow back as a result.
Those over 50 and those descended from Northern Europe are typically affected. Among the symptoms are:
- Ache in the joints or bones.
- Larger head size.
- Bent legs or arms.
- The curved shape of the back.
- Bone fractures.
Medial Tibial Stress Syndrome
Shin splints, sometimes called medial tibial stress syndrome, are characterized by widespread, repeated pain in the lower leg.
It is believed that biomechanical abnormalities causing excessive force on the tibia are the cause, albeit the precise process is not known.
It is most frequently observed in runners and aerobic dancers, who frequently apply excessive power to their legs. It is frequently linked to osteoporosis, low caloric intake, and amenorrhea—the trinity of conditions that affect female athletes.
A significant region of the distal, medial tibia can be palpated to reproduce discomfort, which is indicative of medial tibial stress syndrome. Traction periostitis is the etiology.
Rest and ice are usually used as treatments until the discomfort subsides, at which point activity is gradually resumed.
Ankle Apophysitis of the tibia
Osgood-Schlatter disease, or apophysitis of the tibial tubercle, is characterized by pain beneath the knee that worsens with movement and goes away with rest.
The proximal tibia’s epiphyseal plate experiences recurrent tension as a result of misuse of the knee and excessive physical strain at the point where the patellar tendon inserts into the tibia.
Males between the years of 10 and 15 are the most common ones to have it.
A palpable bony protrusion at the tibial tuberosity may be present at the time of diagnosis and may continue to be so even after the pain subsides.
In order to reduce inflammation, treatment consists of rest, ice, and avoiding high-impact exercises like leaping. Usually, the symptoms go away as the epiphyseal plates close.
IO Access
In emergency situations where vascular access cannot be successfully achieved, interosseous access is employed.
The technique enters the bone marrow of long bones, which supplies the systemic circulation with a rich venous plexus. An IO access point is frequently made use of in the tibia.
The most frequent site is the proximal tibia, which is followed by the distal section.
The proximal humerus is another bone that is frequently used.
Keeping the tibia in good health
You can keep your bone (and general) health in check by maintaining a healthy diet and exercise routine as well as by visiting your doctor for routine examinations.
Speak with your healthcare practitioner about getting a bone density scan if you are over 50 or if osteoporosis runs in your family.
To lower your chance of an accident, abide by these general safety advice:
- Wear your seatbelt at all times.
- When taking part in any sport or activity, wear the proper protective gear.
- Ensure that nothing could trip you or others in your house or business.
- It’s crucial to always reach for objects around the house with the appropriate tools or equipment. Never stand on worktops, tables, or chairs.
- Adhere to a diet and exercise regimen that will support the health of your bones.
- Use a walker or cane if you have difficulty walking or are prone to falls.
FAQs
What is the tibia bone short note?
The tibia is the primary bone of the lower leg, producing the shin as it is more widely known. It stretches at the ends closest to it and farther away from it, articulating at the ankle and knee joints, respectively. The tibia is an essential weight-bearing structure and the second largest bone in the body.
Where are the tibia bones?
The two long bones of the lower leg are called the fibula and tibia. Inside, the tibia is a larger bone than the fibula, which is smaller externally. The fibula is substantially thinner than the tibia. Of the two, it is the primary weight-bearing bone.
What is the tibia known as?
Also called: shinbone, shin shin. Composed and verified by. Updated December 4, 2023 • History of this article. The larger and inner of the two lower leg bones in vertebrates is called the tibia; the other is called the fibula. In humans, the tibia forms the inner ankle protuberance below and the lower portion of the knee joint above.
What is the anatomy of the tibia bone?
The triangular cross-section of the tibia’s body produces three borders: the anterior, medial, lateral, or interosseous, borders. The medial, lateral, and posterior surfaces are formed by these three borders. The fiber, which is frequently mistaken for the fibula, is the forward, flat portion of the tibia.
What are the parts of the tibia of the leg?
The tibia and fibula are the two bones that make up our lower legs. The largest of the two, the tibia or shinbone, is where most of our weight is supported. We are all too familiar with the agony that can result from a direct strike to the shinbone, whether it comes from the notorious scooter or the edge of a chair.
How does the tibia grow?
Children’s growth plates are cartilage zones located at the ends of our long bones, such as the femur and tibia, according to pediatric spine specialist Robert Lark, MD, of Duke University. New bone from the development plate contributes to the growth of these bones.
Reference
- Professional, C. C. M. (n.d.). Tibia. Cleveland Clinic. https://my.clevelandclinic.org/health/body/23026-tibia
- Bourne, M. (2023, August 8). Anatomy, Bony Pelvis and Lower Limb: Tibia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK526053/
- Tibia. (2023, December 9). Wikipedia. https://en.wikipedia.org/wiki/Tibia#
- Tibia | Definition, Anatomy, & Facts. (2023, December 4). Encyclopedia Britannica. https://www.britannica.com/science/tibia