Pulmonary Vein
Introduction
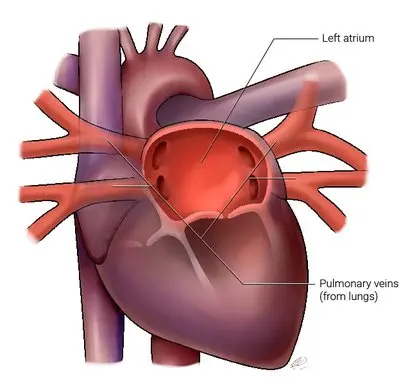
The pulmonary veins are a group of blood vessels that play a crucial role in the circulatory system. The transport of oxygenated blood in the human body leans on the pulmonary veins. Surprisingly, the veins rearrange oxygen-rich blood from the lungs and carry it to the heart, specifically from the pulmonary circulation to the left atrium of the human heart.
The pulmonary veins are the vessels that carry oxygenated blood from the lungs to the heart, and they possess unique attributes. The four main pulmonary veins are the largest and take blood from a lung to the left atrium of the heart. The pulmonary circulation is made up of the pulmonary veins.
Function of the Pulmonary Vein
It is established that each of the pulmonary veins’ purpose is to keep the body’s tissues and organs oxygenated. Here is a comprehensive look at their functions:
- Transport of Oxygenated Blood: The preliminary function of the pulmonary veins is to transport oxygen-rich blood from the lungs back to the heart. After the blood has been oxygenated in the lungs through a process of respiration (where oxygen is absorbed and carbon dioxide is released), it enters the pulmonary veins.
- From Lungs to Heart: Oxygenated blood from the lungs enters the pulmonary veins via small vessels that collect blood from the capillary networks surrounding the alveoli (air sacs). These small vessels gradually merge into the larger pulmonary veins as they move further toward the heart of humans.
- Entry into the Heart: The pulmonary veins enter in the heart at the left atrium of the human body structure. Here, the oxygenated blood mixes with blood returning from the body (deoxygenated blood) through the superior and inferior vena cava. After that, the left atrium accords to drive the oxygenated blood into the left ventricle.
- Distribution to the Body: Once it reaches the left ventricle, the oxygenated blood is expelled from the heart via the aorta and its branches, supplying oxygen to all the body’s tissues and organs. This oxygen is essential for cellular respiration, which produces energy (in the form of ATP) needed for various physiological processes.
- Role in Circulatory System: The pulmonary veins are integral to the systemic circulation, which distributes oxygenated blood all over the body. This ensures that all cells receive the oxygen required for their metabolic activities and survival.
- Pressure Regulation: The pulmonary veins might also play a role in regulating the pressure within the pulmonary circulation in the human being. They have thinner walls compared to arteries, allowing them to accommodate the relatively lower pressure of the pulmonary circulation system.
- Clinical Importance: Problems with the pulmonary veins can lead to significant health issues. Conditions such as pulmonary vein stenosis (narrowing of the veins), anomalous pulmonary venous connection (abnormal connection to the heart), or pulmonary hypertension (elevated pressure in the pulmonary arteries) can affect the efficiency of oxygenation and circulation, necessitating medical intervention.
In abridgment, the pulmonary veins are necessary for returning oxygenated blood from the lungs to the heart, where it is pumped out to the mortal body. This process ensures that tissues receive the oxygen necessary for energy production and overall physiological function.
Anatomy of the Pulmonary Vein
The anatomy of the pulmonary veins concerns their structure, alliance, and how they encourage the flow of oxygenated blood from the lungs to the heart. Here’s a detailed overview:
Structure of Pulmonary Veins:
- Number and Location: In human beings, there are normally two pulmonary veins in each lung and/or four in the total structure of human anatomy.
- Left Lung: It usually has two pulmonary veins – There is one superior and one inferior.
- Right Lung: It also typically has two pulmonary veins.
- Origin: The source of the pulmonary veins is the pulmonary capillary networks, where the blood acquires oxygen due to the respiration comes to pass in the alveoli (air sacs) within the mortal lungs.
- Course: Blood passes through tiny venules that eventually combine to form larger veins when it becomes oxygenated in the lungs’ capillaries.
- These veins then merge into larger vessels as they approach the hilum (central area) of each lung.
- Left Atrium Connection: Each lung’s pulmonary veins merge into one or two larger veins that eventually enter the left atrium of the heart.
- The junctions where the pulmonary veins enter the left atrium are guarded by valves to prevent the backflow of blood.
- Histology: The walls of the pulmonary veins consist of three typical layers of veins: an inner endothelial layer, a middle smooth muscle layer, and/or an outer connective tissue layer.
- The veins in the lungs have thinner walls than arteries because they pass on blood at a lower pressure.
- Anatomic Variations: Anomalous pulmonary venous connections are rare but can occur, where one or more pulmonary veins do not connect to the left atrium but instead to another location in the heart or venous system.
Pathway of the Pulmonary Vein
Certainly! Let’s glance at the accurate course of the pulmonary veins, paying attention to how oxygenated blood reaches from the lungs back to the heart:
Oxygenation in the Lungs
- Pulmonary Capillaries: The lungs receive deoxygenated blood from the right ventricle of the heart in humans via the pulmonary arteries.
- Gas Exchange: In the pulmonary capillaries surrounding the alveoli (air sacs), both carbon dioxide and oxygen move from the blood into the alveoli and from the alveoli into the blood.
- Oxygenation: This exchange process oxygenates the blood, transforming it from deoxygenated to oxygenated blood.
Collection and Formation of Pulmonary Veins
- Pulmonary Venules: The pulmonary venules are tiny veins that collect oxygenated blood from the pulmonary capillaries.
- Convergence: As they approach the lung hilum, pulmonary venules combine to produce more expansive veins known as pulmonary veins.
Pulmonary Veins in Each Lung
- Left Lung: The left lung typically contains two pulmonary veins regularly.Superior Pulmonary Vein: It Drains the upper lobe of the left lung in the human body.
- Inferior Pulmonary Vein: It supplies air to the left lung’s lower lobe.
- Right Lung: On an ordinary basis, the right lung also has two pulmonary veins: Superior Pulmonary Vein: Drains the upper lobe of the right lung.
- Inferior Pulmonary Vein: The inferior pulmonary vein is accountable for draining the middle lobes and lower lobes of the right side of the right lung.
Pathway Towards the Heart
- Convergence at the Hilum: The superior and inferior pulmonary veins from each lung converge near the hilum of the lung, where they join together to form larger vessels.
- Left Atrium: The merged pulmonary veins from both lungs enter the left atrium of the heart through its posterior surface.
- Valves: The entry points of the pulmonary veins into the left atrium are guarded by valves that prevent the backflow of blood.
Return to Systemic Circulation
- Left Atrium to Left Ventricle: Upon entering the left atrium, oxygenated blood mixes briefly with deoxygenated blood returning from the body via the pulmonary veins.
- Left Ventricle: The left atrium contracts, pushing the oxygenated blood through the mitral valve into the left ventricle.
- Aorta: Blood that has been oxygenated is pumped from the left ventricle through the aortic valve into the aorta and then into the systemic circulation, where it is delivered to tissues and organs throughout the body.
Clinical Relevance –
Malformations: Anomalous pulmonary venous connections or stenosis (narrowing) can impair blood flow and oxygenation.
Conditions: Pulmonary hypertension or heart failure can affect the function of the pulmonary veins and circulation of oxygenated blood. Understanding the detailed pathway of the pulmonary veins is crucial for comprehending the circulation of oxygenated blood and diagnosing and treating conditions that affect pulmonary vein function.
Clinical Importance
The clinical relevance of the pulmonary veins lies in their essential role in oxygenating blood and their involvement in various medical conditions. Here are some key clinical aspects related to pulmonary veins:
- Anomalous Pulmonary Venous Connections: This condition occurs when one or more pulmonary veins connect abnormally to the heart or other blood vessels instead of the left atrium. It can also lead to the mixing of oxygenated blood and deoxygenated blood, reducing overall oxygen delivery to the body.
- Pulmonary Vein Stenosis: The pulmonary veins can become narrowed, which may limit the flow of blood from the lungs to the heart and cause higher pressure in the pulmonary circulation, resulting in decreased oxygenation of tissues.
- Pulmonary Hypertension: Elevated pressure in the pulmonary arteries and veins can occur due to various underlying conditions. The heart may experience strain as a result of pulmonary hypertension, and it might also result in complications such as heart failure in body organs.
- Atrial Fibrillation: A common heart rhythm disorder where the atria (including the left atrium) beat irregularly. The pulmonary veins are often a focus of treatment for this condition, as abnormal electrical activity originating from the pulmonary veins can trigger atrial fibrillation.
- Surgical Interventions: During certain cardiac surgeries, such as repairing congenital heart defects or treating atrial fibrillation, surgeons may manipulate the pulmonary veins directly. This includes techniques like pulmonary vein isolation to control abnormal electrical impulses.
- Imaging and Diagnosis: Imaging modalities such as echocardiography, CT scans, and MRI are employed to imagine the pulmonary veins and analyze abnormalities such as aberrant connections or stenosis.
- Management and Treatment: Management of conditions involving the pulmonary veins often involves a multidisciplinary approach including cardiologists, cardiothoracic surgeons, and sometimes interventional radiologists or electrophysiologists. Treatments may include medications to manage pulmonary hypertension, surgical repair of aberrant connections, or catheter-based procedures to correct arrhythmias.
Understanding the clinical relevance of the pulmonary veins is crucial for diagnosing, managing, and treating various cardiovascular conditions that affect oxygenation and overall heart function.
Variation of pulmonary veins
Variations in pulmonary veins can involve differences in their number, size, course, and even their connection to the heart. Here are some notable variations:
Number of Pulmonary Veins:
- While the typical anatomy includes two pulmonary veins from each lung (superior and inferior), variations can occur where additional veins are present or where one or more veins may be absent.
- For instance, some individuals may have three pulmonary veins from one lung due to an extra branch or an aberrant connection.
Anomalous Pulmonary Venous Connections:
- This is a significant variation in which the pulmonary veins do not typically connect to the left atrium.
- Scimitar Syndrome: Anomalously, the right superior pulmonary vein rather than the left atrium links to the inferior vena cava, one of the pulmonary veins.
- Total Anomalous Pulmonary Venous Connection (TAPVC): All pulmonary veins connect to a systemic vein or directly to the right atrium.
Pulmonary Vein Stenosis:
- Pulmonary veins might become restricted or develop stenosis, which could also influence the flow of blood from the lungs to the heart.
- This can be congenital or acquired, and it can also lead to increased pressure in the pulmonary circulation and decreased oxygenation.
Size and Course Variations:
- Pulmonary veins can vary in size and course as they traverse through the lung tissue towards the hilum.
- Variations in size might also affect the efficiency of oxygenated blood transport in the body.
Bilateral Symmetry:
- While most people have a symmetrical arrangement of pulmonary veins (two from each lung), there can be asymmetrical patterns where the number or course differs between the left and right lungs.
Clinical Significance:
- Variations in pulmonary veins can impact surgical planning, particularly in procedures involving cardiac surgeries, catheter interventions for arrhythmias (like atrial fibrillation), or treatment of congenital heart defects.
- These variations may also pose challenges in imaging and diagnosis, requiring detailed evaluation using imaging techniques such as CT angiography or MRI of humans.
Understanding variations in pulmonary veins is crucial for cardiologists, cardiothoracic surgeons, and other healthcare providers involved in diagnosing and managing cardiovascular conditions. These variations highlight the complexity and diversity in cardiovascular anatomy, influencing treatment strategies and patient outcomes.
What are the pulmonary vein’s branches and tributaries?
The main function of the pulmonary veins is to carry oxygenated blood from the lungs back to the heart. Here’s a list of their contributing vessels and offshoots:
Contributing Vessels of Pulmonary Veins: The contributing vessels of the pulmonary veins possess:
Superior Pulmonary Vein:
- Upper Lobe Tributaries: Receives blood from the veins draining the upper lobes of both lungs.
- Accessory Tributaries: In some individuals, there may be additional small veins contributing to the superior pulmonary vein.
Inferior Pulmonary Vein:
- Middle and Lower Lobe Tributaries: Blood from the middle and lower lobes of both lungs is drained by the middle and lower lobe tributaries.
- Accessory Tributaries: Identical to the superior pulmonary vein, there might be deviations in the numeral or size of veins contributing to the inferior pulmonary vein.
Branches of Pulmonary Veins
- The pulmonary veins themselves do not have traditional branches in the way arteries do. Instead, they collect blood from smaller pulmonary venules and gradually merge to form larger vessels that eventually enter the heart.
Additional Details:
- Variations: There can be variations in the number of pulmonary veins, with some individuals having additional small veins contributing to the main pulmonary veins.
- Clinical Considerations: Understanding the anatomical variations and the specific tributaries of pulmonary veins is crucial for surgical planning, especially in procedures involving the correction of congenital heart defects or treatment of conditions like pulmonary vein stenosis.
In overview, the leading tributaries of the pulmonary veins possess veins draining from the upper, middle, and lower lobes of both lungs. These veins unite to assemble the superior and/or inferior pulmonary veins, which then transport oxygenated blood around to the heart for allocation to the rest of the human body.
How do you Identify pulmonary veins?
Identifying pulmonary veins involves understanding their anatomical location, course, and characteristics in various imaging modalities. Here is a thorough method for recognizing the pulmonary veins: Take the above text and rephrase each sentence. Ensure that none of the meaning is lost and do not add new sentences.
Imaging Modalities:
Echocardiography:
- Transthoracic Echocardiography: Provides a non-invasive method to visualize the heart and its structures, including the pulmonary veins.
- Transesophageal Echocardiography: Offers higher resolution images of the heart and pulmonary veins by using an ultrasound probe inserted into the esophagus.
Computed Tomography (CT) Angiography:
- Contrast-enhanced CT: A common method to image pulmonary veins and assess their anatomical details, including size, course, and presence of anomalies.
- Multi-detector CT: Provides high-resolution 3D images that can delineate the pulmonary veins and their relationship to surrounding structures.
Magnetic Resonance Imaging (MRI):
- MRI Angiography: Employ magnetic fields and radio waves to create comprehensive images of blood arteries, including the pulmonary veins.
- Magnetic Resonance Venography (MRV): Specifically focuses on imaging veins, including the pulmonary veins, to assess their anatomy and function.
What conditions can affect pulmonary veins?
Several conditions may also interfere with the pulmonary veins’ function and potentially jeopardize blood oxygenation. Here are some notable conditions:
Anomalous Pulmonary Venous Connection (APVC):
- This congenital condition occurs when one or more pulmonary veins connect abnormally to the heart or other veins rather than the left atrium.
- Types include Total Anomalous Pulmonary Venous Connection (TAPVC) where all the pulmonary veins connect elsewhere, often to the right atrium and/or systemic veins in the human body.
Pulmonary Vein Stenosis:
- Narrowing or obstruction of pulmonary veins can occur congenitally or as a result of scarring (from previous surgeries, radiofrequency ablation, etc.).
- Stenosis restricts blood flow from the lungs to the heart, leading to increased pressure in the pulmonary circulation and reduced oxygenation.
Pulmonary Hypertension:
- Elevated pressure in the pulmonary arteries and/or veins can also occur due to numerous underlying disorders.
- Additionally, pulmonary hypertension can also put stress on the heart and might also interfere with the pulmonary vein function, which could also result in heart failure.
Atrial Fibrillation (AF):
- AF is a common arrhythmia where the atria (including the left atrium where pulmonary veins enter) beat irregularly.
- Treatments like pulmonary vein isolation are also necessary because abnormal electrical impulses coming from the pulmonary veins might cause and prolong Atrial fibrillation.
Heart Failure:
- In cases of severe heart failure, increased pressure in the left atrium can affect the function and dilation of the pulmonary veins.
- This might also contribute to congestion in the lungs (pulmonary edema) and/or exacerbate symptoms of heart failure.
Congenital Heart Defects:
- Some congenital heart abnormalities, like atrial septal defects (ASDs) or ventricular septal defects (VSDs), may also impact the structure and operation of the pulmonary veins.
- These abnormalities can also cause irregular blood flow and impact the oxygenation of the heart or body.
Thrombosis and Embolism:
- Blood clots can occasionally form within the pulmonary veins or migrate from other parts of the body (e.g., deep vein thrombosis in the legs).
- Pulmonary embolism can also restrict the flow of blood and oxygen when a clot gets ensconced in a pulmonary vein or pulmonary artery within an individual.
Pulmonary Vein Obstruction Post-Surgery:
- In some cases, surgeries involving the heart or pulmonary veins may inadvertently cause scarring or narrowing, leading to obstruction and impaired blood flow.
Clinical Management:
- Diagnosing and managing conditions affecting the pulmonary veins often involves imaging studies (such as echocardiography, CT, or MRI), cardiac catheterization, and sometimes surgical intervention.
- Treatment approaches may include medications to manage hypertension or arrhythmias, surgical repair or reconstruction of anomalous connections or stenosis, and interventions to alleviate symptoms and improve oxygenation.
Understanding these conditions is crucial for timely diagnosis and appropriate management to maintain optimal cardiovascular health and function.
What treatments are available for pulmonary vein conditions?
The potential treatments for conditions impacting the pulmonary veins are determined by the particular diagnosis and the specific underlying cause. Here are the main treatment approaches:
Medications:
- Anticoagulants: Anticoagulants are utilized to prevent blood clots from forming in the pulmonary veins and/or to treat the pulmonary embolism.
- Antiarrhythmic Drugs: Prescribed to control irregular heart rhythms, particularly in cases of atrial fibrillation (AF) originating from the pulmonary veins.
- Vasodilators: Medications that relax and widen blood vessels, often used to manage pulmonary hypertension.
Surgical Interventions:
- Repair of Anomalous Connections: In cases of total anomalous pulmonary venous connection (TAPVC), surgical correction is typically required to redirect the veins to the correct drainage pathway into the left atrium.
- Pulmonary Vein Stenosis Repair: Surgical techniques such as angioplasty (balloon dilation) or stent placement may be used to widen narrowed pulmonary veins.
- Thrombectomy: Surgical removal of blood clots within the pulmonary veins or embolized material.
Catheter-based Procedures:
- Pulmonary Vein Isolation (PVI): A procedure used to treat atrial fibrillation (AF) by creating scar tissue around the pulmonary veins to block abnormal electrical signals that trigger AF.
- Balloon Pulmonary Vein Angioplasty: Similar to coronary angioplasty, this involves using a balloon catheter to widen narrowed pulmonary veins.
Lifestyle Modifications and Supportive Therapies:
- Oxygen Therapy: Supplemental oxygen may be prescribed to improve oxygenation in cases of severe pulmonary vein stenosis or pulmonary hypertension.
- Management of Underlying Conditions: Treating conditions such as heart failure or congenital heart defects that contribute to pulmonary vein dysfunction.
Follow-up Care and Monitoring:
- Regular follow-up visits with a cardiologist or cardiovascular specialist are essential to monitor the effectiveness of treatment and manage any potential complications.
- Imaging studies such as echocardiography, CT angiography, or MRI may be performed periodically to assess the condition of the pulmonary veins and overall cardiac function.
Treatment selections are tailored to specific patient needs, taking into account aspects such as the severity of the ailment, overall health state, and response to first treatments. Patients require assistance to work closely with their healthcare team to determine the most appropriate treatment plan and upgrade long-term cardiovascular health.
What are the common symptoms of pulmonary vein disorders?
Pulmonary vein disorders can present with a variety of symptoms depending on the specific condition and its severity. Here are some common symptoms associated with pulmonary vein disorders:
Shortness of Breath (Dyspnea):
- Trouble in breathing, especially during physical activity and/or when lying flat (orthopnea).
- A lack of breath might also be gradual and/or worsen with time.
Chest Pain or Discomfort:
- Pain in the chest area, which may be sharp or dull.
- Distress or tension in the chest, often exacerbated by exertion.
Fatigue and Weakness:
- Feeling unusually tired, even after adequate rest.
- Generalized weakness and decreased stamina.
Swelling (Edema):
- Swelling in the ankles, feet, or abdomen (ascites), may indicate fluid retention due to impaired circulation or heart failure.
Palpitations and Irregular Heartbeat:
- The sensation of rapid, fluttering, or irregular heartbeats, particularly in cases of atrial fibrillation originating from the pulmonary veins.
Cough:
- Persistent or chronic cough, which may be dry or produce frothy sputum.
- Coughing might also worsen at night or with exertion.
Syncope (Fainting):
- Loss of consciousness or near-fainting episodes can occur due to reduced oxygen delivery to the brain in severe cases.
Cyanosis:
- Bluish discoloration of the lips, fingertips, or skin, indicating poor oxygenation of blood.
Exercise Intolerance:
- Difficulty performing physical activities or exercise due to inadequate oxygen supply to muscles and tissues.
Signs of Pulmonary Hypertension:
- Symptoms such as dizziness, chest pain, and/or feeling faint during physical activity might also indicate issues.
Key Anatomical Features:
- Location: The Pulmonary veins are encountered within the lung tissue, joining towards the hilum of individual lungs where they depart and/or enter into the left atrium of the heart in the human body.
- Course: Pulmonary veins traditionally run parallel to the pulmonary arteries, but they provide oxygenated blood to the heart. Understanding their course helps in distinguishing them from other structures.
- Connection to the Heart: Pulmonary veins enter into the left atrium of the heart, usually in the posterior aspect of the heart. Their entry points are often visualized to ensure normal connection and function.
Identifying Anomalies:
- Anomalous Connections: Examine for any abnormal associations where pulmonary veins may bond to systemic veins or directly to the right atrium rather than the left atrium.
- Stenosis or Narrowing: Assess for any narrowing or stenosis in the pulmonary veins, which can affect blood flow and oxygenation.
Clinical Considerations:
- Congenital Anomalies: Understanding variations in pulmonary vein anatomy is crucial for diagnosing and managing congenital heart defects.
- Surgical Planning: Precise identification of pulmonary veins aids in surgical planning for procedures such as repair of congenital defects, treatment of pulmonary vein stenosis, or ablation procedures for atrial fibrillation.
Summary
Identifying pulmonary veins involves utilizing various imaging modalities to visualize their anatomical details, including location, course, connections, and any anomalies. This information is critical for accurate diagnosis and effective management of cardiovascular conditions involving the pulmonary veins.
Disclaimer
This information is provided solely for informational purposes and should not be used as medical advice. It is not meant to take the place of speaking with a licensed healthcare provider. The content is based on general knowledge and understanding as of the current date and may not encompass all possible conditions, treatments, or outcomes related to pulmonary veins. Medical conditions involving pulmonary veins might also vary widely in their presentation and management. Diagnosis and treatment should be tailored to individual patient circumstances and should only be undertaken by healthcare professionals with access to patient-specific information.
While efforts are made to ensure the accuracy and relevance of the information presented, medical knowledge is constantly evolving. Therefore, users are encouraged to consult their healthcare provider for personalized medical advice and treatment recommendations regarding pulmonary vein disorders or any other health concerns. Any specific tests, practices, goods, or viewpoints stated on this site are not supported or promoted by us. It is entirely the user’s choice and risk to rely on any information found here. We expressly disclaim any responsibility for any damage or harm caused by using or relying on this material.
This disclaimer helps ensure that readers understand the limitations of the provided information and emphasizes the importance of consulting healthcare professionals for personalized medical advice and care.
FAQ
How many pulmonary veins enter each lung?
The standard design of four pulmonary veins possesses two pulmonary veins for individual lungs, which open individually into the left atrium. The right superior pulmonary vein drains the blood from the right superior lobes and right middle lobes. The right inferior pulmonary vein drains the blood from the right inferior lobe in the human body.
Do pulmonary arteries carry oxygenated blood?
From the right ventricle, the pulmonary artery transports blood with low oxygen coverage to the lungs, where oxygen is sponged into the blood. The left atrium of the heart receives blood rich in oxygen from the pulmonary veins. The left ventricle disperses blood that is excessively oxygenated to the body through the aorta of the heart.
What are pulmonary veins?
Pulmonary veins are the blood vessels that carry oxygenated blood from the lungs and back to the heart in humans. They are unique among veins because they transport oxygen-rich blood, whereas most veins carry deoxygenated blood.
How do pulmonary veins differ from other veins?
Unlike most of the veins that bring deoxygenated blood, pulmonary veins bring oxygen-rich blood in humans. They also have more delicate walls compared to arteries because they transport blood beneath lower pressure.
Why are pulmonary veins important?
Pulmonary veins play a crucial role in maintaining the oxygenation of tissues and organs throughout the body. Their proper function ensures the effective delivery of oxygenated blood from the lungs to the heart and systemic circulation.
Can pulmonary vein issues be prevented?
Some congenital anomalies may not be preventable, but maintaining overall cardiovascular health through regular exercise, a balanced diet, and avoiding smoking can reduce the risk of developing certain conditions affecting the pulmonary veins.
Reference
A good reference for information on the pulmonary vein would typically be a comprehensive anatomy textbook or a specialized medical reference book on cardiology or pulmonary medicine. Here are a few specific recommendations:
- “Gray’s Anatomy for Students,” authored by Richard Drake and others, is the source of the original text. My task is to rephrase each sentence without altering the original meaning or adding new sentences. This is a widely used anatomy textbook that provides detailed information on the structure and function of the pulmonary vein clearly and also concisely.
- Netter’s Atlas of Human Anatomy by Frank H. Netter – Known for its detailed illustrations, this atlas includes images and descriptions of the pulmonary vein within the context of human anatomy.
- The Heart, edited by Valentin Fuster and others, is a book by Hurst- This is a comprehensive cardiology textbook that covers the anatomy, physiology, and pathology of the cardiovascular system, including the pulmonary vein.
- Vinay Kumar and colleagues authored the book Robbins and Cotran Pathologic Basis of Disease – Although primarily a pathology textbook, it provides insights into the structural aspects and functional aspects of the various organs, including the pulmonary vein.
- UpToDate (online resource) – This clinical decision support system offers authoritative, evidence-based information on various medical topics, including detailed articles on the anatomy and function of the pulmonary vein.
These resources should provide a solid foundation of knowledge regarding the pulmonary vein, suitable for both medical professionals and students seeking detailed information.